NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
LiverTox: Clinical and Research Information on Drug-Induced Liver Injury [Internet]. Bethesda (MD): National Institute of Diabetes and Digestive and Kidney Diseases; 2012-.

LiverTox: Clinical and Research Information on Drug-Induced Liver Injury [Internet].
Show detailsOVERVIEW
Introduction
Hydroxyurea is an antimetabolite that is used in the treatment of cancer and to stimulate fetal hemoglobin production in sickle cell disease. Hydroxyurea is associated with a low rate of transient serum enzyme and bilirubin elevations during therapy, and has been implicated in rare cases of clinically apparent acute liver injury with jaundice.
Background
Hydroxyurea (hye drox” ee ure ee’ a) is a hydroxylated analogue of urea and an antimetabolite which inhibits the enzyme ribonucleotide reductase, which is necessary for DNA synthesis and cell cycle replication. Blocking the enzyme results in cell cycle arrest in the S phase, but does not interfere with RNA or protein synthesis. Hydroxyurea is used in the treatment of solid tumors and myeloproliferative diseases, the latter because of its effects in reducing excessive production of red blood cells (polycythemia vera), white blood cells (chronic myelogenous leukemia) or platelets (essential thrombocythemia). Hydroxyurea also increases the production of fetal hemoglobin, via an unknown mechanism of action, which increases overall hemoglobin levels and decreases sickling in patients with sickle cell anemia. In controlled clinical trials, hydroxyurea has been shown to increase hemoglobin concentrations, decrease transfusion requirements and lessen painful crises in patients with sickle cell disease. Hydroxyurea was first approved for use in the United States in 1967 as an antineoplastic agent for therapy of melanoma, chronic myelogenous leukemia, ovarian carcinoma, and head and neck cancers. The indications were expanded to sickle cell disease in 1998, which is the major indication for its use at present. Hydroxyurea is available in capsules of 200, 300, 400 and 500 mg generically and under brand names as Droxia (for sickle cell disease) and Hydrea (for cancer). The usual dose in sickle cell disease is 15 mg/kg/day, with subsequent dose adjustments based upon efficacy and tolerance to a maximum of 35 mg/kg/day. Common side effects include bone marrow suppression (particularly thrombocytopenia), nausea, vomiting, anorexia, diarrhea, mucositis, hair loss, headache, rash and fever. Uncommon, but potentially severe adverse reactions include severe vasculitic skin ulcers, neuropathy, renal dysfunction, severe bone marrow suppression, pulmonary fibrosis, and embryo-fetal toxicity. Long term hydroxyurea therapy may increase the risk of cancer.
Hepatotoxicity
Serum aminotransferase and bilirubin elevations occur in a small proportion of patients on conventional doses of hydroxyurea and a greater proportion at higher doses. However, the serum enzyme elevations are rarely associated with symptoms and are generally self-limited and resolve rapidly, rarely requiring dose modification.
Cases of clinically apparent liver injury attributed to hydroxyurea have been reported, but are rare. Two clinical presentations have been described: an acute syndrome of drug fever and mild hepatitis that resolves rapidly with stopping, and a less well characterized acute hepatitis-like injury which can be severe and even fatal, arising after several months of treatment and usually in patients on other hepatotoxic medications.
Drug fever occurs in up to 1% of patients treated with hydroxyurea, typically arising within 1 to 3 weeks of starting and presenting with high fevers and mild constitutional symptoms of fatigue and nausea (Case 1 below). The fevers are typically cyclic and temperature can rise to 41oC at intervals of every 1 to 3 days as long as therapy is continued. The fevers are generally well tolerated, although they may be accompanied by nausea, diarrhea, anorexia or fatigue. Approximately one third of patients will also have some degree of serum enzyme elevations, typically increases in both aminotransferase and alkaline phosphatase levels, with minimal increases in serum bilirubin. The liver injury is usually mild and asymptomatic and the symptom of fever predominates. White blood cell and eosinophil counts are usually normal at the time of onset, but may arise if therapy is continued. Rash and other signs of hypersensitivity are uncommon. Both the fever and liver test abnormalities resolve promptly once hydroxyurea is stopped–the fever within 24 to 48 hours and the liver test elevations within 2 to 4 weeks. The fever recurs with reexposure, generally within 24 hours.
In addition, rare instances of acute hepatitis that can be severe and lead to hepatic failure and death have been described in patients taking hydroxyurea and antiretroviral therapy for HIV/AIDS. This presentation is clearly different from the hepatitis that accompanies drug fever from hydroxyurea, and resembles acute viral hepatitis with marked elevations in serum aminotransferase levels and jaundice and only mild-to-moderate elevations in alkaline phosphatase. Immunoallergic and autoimmune features are not usually present. Some cases have been fatal; others have been marked by slow, but ultimately full recovery. The cases of severe hepatitis attributed to hydroxyurea have been described largely in patients with HIV infection on antiretroviral regimens that include agents associated with hepatotoxicity, but the addition of hydroxyurea appeared to be responsible for the liver injury, these patients later tolerating resumption of antiretroviral therapy without recurrence.
Likelihood score: C (probable cause of clinically apparent liver injury).
Mechanism of Injury
The syndrome of fever and acute hepatitis arising within 1 to 3 weeks of starting hydroxyurea is probably due to hypersensitivity. The cause of acute liver failure attributed to hydroxyurea is unknown, but may be related to drug-drug interactions with other potentially hepatotoxic agents. Hydroxyurea is metabolized in the liver via the cytochrome P450 enzymes at least in part, but its drug-drug interactions have not been well characterized.
Outcome and Management
The severity of the liver injury linked to hydroxyurea therapy is usually mild and self-limited. It has not been linked to cases of chronic hepatitis or vanishing bile duct syndrome. There is no information to suggest that there is cross sensitivity to hepatic injury between hydroxyurea and other antimetabolites or anticancer agents.
Drug Class: Antineoplastic Agents, Miscellaneous; Genetic Disorder Agents, Hematologic Agents, Sickle Cell Disease Agents
CASE REPORT
Case 1. Fever and hepatitis due to hydroxyurea.(1)
A 46 year old woman with polycythemia vera developed spiking fevers 3 weeks after starting hydroxyurea [500 mg twice daily]. She had no history of liver disease, alcohol abuse or drug allergies or risk factors for viral hepatitis. Her only other medication was hydroxyzine. She was admitted to the hospital and continued to have spiking fevers to as high as 41.5 oC for 8 days until hydroxyurea was stopped, whereupon the fever resolved within 24 hours. Liver test results were also abnormal, with peak values of bilirubin of 1.0 mg/dL, ALT 271 U/L, AST 135 U/L, alkaline phosphatase 1047 U/L and GGT 585 U/L. Tests for viral hepatitis were negative. In follow up, the liver test abnormalities evidently resolved. One year later, she was rechallenged with hydroxyurea and developed fever 24 hours later.
Key Points
| Medication: | Hydroxyurea, 500 mg twice daily |
|---|---|
| Pattern: | Cholestatic (R=1.0) |
| Severity: | 1+ (enzyme elevations and symptoms without jaundice) |
| Latency: | 3 weeks |
| Recovery: | Not given |
| Other medications: | Hydroxyzine |
Comment
Drug fever occurs in approximately 1% of patients treated with hydroxyurea, but is generally benign and rapidly reversible with drug discontinuation. Liver tests abnormalities are reported in about one third of cases, but typically in patients in whom the drug is continued for several days or weeks in the face of recurrent fevers, as occurred in this case. The liver test abnormalities are usually mild, anicteric and resolve within 2 to 4 weeks of stopping the medication. The pattern of serum enzyme elevations is typically mixed or cholestatic, but hepatocellular instances have also been reported. In rare instances, jaundice has occurred, but there have been no reports of acute liver failure, chronic hepatitis or vanishing bile duct syndrome attributed to hydroxyurea associated hepatitis with drug fever.
PRODUCT INFORMATION
REPRESENTATIVE TRADE NAMES
Hydroxyurea – Generic, Hydrea® (for cancer), Droxia® (for sickle cell disease)
DRUG CLASS
Antineoplastic Agents; Sickle Cell Disease Agents
Product labeling at DailyMed, National Library of Medicine, NIH
CHEMICAL FORMULA AND STRUCTURE
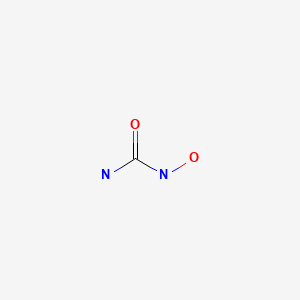
| DRUG | CAS REGISTRY NO. | MOLECULAR FORMULA | STRUCTURE |
|---|---|---|---|
| Hydroxyurea | 127-07-1 | C-H4-N2-O2 |
|
CITED REFERENCES
- 1.
- Westerman DA, Schwarer A, Grigg AP. Hydroxyurea-induced fever and hepatitis. Aust N Z J Med. 1998;28:657–9. [PubMed: 9847957]
ANNOTATED BIBLIOGRAPHY
References updated: 12 July 2021
- Zimmerman HJ. Oncotherapeutic and immunosuppressive agents. In, Zimmerman HJ. Hepatotoxicity: the adverse effects of drugs and other chemicals on the liver. 2nd ed. Philadelphia: Lippincott, 1999, pp. 673-708.(Expert review of hepatotoxicity of cancer chemotherapeutic agents published in 1999; mentions that hydroxyurea resembles urethane in structure and has been associated with hypersensitivity and hepatitis).
- DeLeve LD. Cancer chemotherapy. In, Kaplowitz N, DeLeve LD, eds. Drug-induced liver disease. 3rd ed. Amsterdam: Elsevier, 2013, pp. 541-67.(Review of hepatotoxicity of cancer chemotherapeutic agents; does not discuss hydroxyurea).
- Wellstein A, Giaccone G, Atkins MB, Sausville EA. Hydroxyurea. Cytotoxic drugs. In, Brunton LL, Hilal-Dandan R, Knollman BC, eds. Goodman & Gilman's the pharmacological basis of therapeutics. 13th ed. New York: McGraw-Hill, 2018, pp. 1195-6.(Textbook of pharmacology and therapeutics).
- Moschella SL, Greenwald MA. Psoriasis with hydroxyurea. An 18-month study of 60 patients. Arch Dermatol. 1973;107:363–8. [PubMed: 4692124](Among 60 patients with severe psoriasis treated with hydroxyurea for up to 18 months, 63% had a beneficial response and side effects included marrow suppression, but none had AST elevations or hepatotoxicity; six patients developed fever and an influenza-like syndrome shortly after starting therapy and two redeveloped fever on rechallenge, but liver enzymes remained normal).
- Heddle R, Calvert AF. Hydroxyurea induced hepatitis. Med J Aust. 1980;1:121. [PubMed: 7374520](64 year old male with psoriasis developed fatigue, nausea and fever, 18 days after starting hydroxyurea [bilirubin 1.6 mg/dL, AST 524 U/L, Alk P 128 U/L], resolving rapidly upon stopping and recurring with fever of 40 oC, drowsiness, delirium and mild elevations of serum enzymes within 5 hours, resolving within 2 days).
- Bauman JL, Shulruff S, Hasegawa GR, Roden R, Hartsough N, Bauernfeind RA. Fever caused by hydroxyurea. Arch Intern Med. 1981;141:260–1. [PubMed: 7458524](56 year old woman with psoriasis developed spiking fevers without eosinophilia or rash after starting hydroxyurea, resolving rapidly on stopping and rapidly recurring on reexposure [liver enzymes were "mildly elevated", but bilirubin was normal]).
- Sharon R, Tatarsky I, Ben-Arieh Y. Treatment of polycythemia vera with hydroxyurea. Cancer. 1986;57:718–20. [PubMed: 3943010](Among 36 patients with polycythemia vera treated with hydroxyurea for 1-5 years, 2 developed fever, 1 hyperbilirubinemia and 2 renal failure; ALT elevations and hepatotoxicity not mentioned).
- Blonk MC, Ossenkoppele GJ. Hydroxyurea as a cause of drug fever in chronic myeloid leukaemia. Neth J Med. 1988;32:240–2. [PubMed: 3164836](63 year old man with CML developed fever 10 days after starting hydroxyurea, resolving rapidly on stopping and recurring rapidly with reexposure; no mention of liver test results).
- Charache S, Terrin ML, Moore RD, Dover GJ, Barton FB, Eckert SV, McMahon RP, Bonds DR. Effect of hydroxyurea on the frequency of painful crises in sickle cell anemia. Investigators of the Multicenter Study of Hydroxyurea in Sickle Cell Anemia. N Engl J Med. 1995;332:1317–22. [PubMed: 7715639](Among 299 patients with sickle cell disease treated with hydroxyurea or placebo for up to 2 years, pain crises were fewer in hydroxyurea treated subjects and hemoglobin levels were higher; serious adverse events included one patient with fulminant hepatitis in the hydroxyurea treated group, but no details provided).
- Starmans-Kool MJ, Fickers MM, Pannebakker MA. An unwanted side effect of hydroxyurea in a patient with idiopathic myelofibrosis. Ann Hematol. 1995;70:279–80. [PubMed: 7599291](79 year old man with myelofibrosis developed fever and diarrhea 20 days after starting hydroxyurea [normal white counts, no mention of liver tests], which resolved within 24 hours of stopping).
- Lossos IS, Matzner Y. Hydroxyurea-induced fever: case report and review of the literature. Ann Pharmacother. 1995;29:132–3. [PubMed: 7756710](63 year old man with essential thrombocytosis developed fever and flu-like symptoms within 24 hours of starting hydroxyurea [39 oC] with normal white count and liver tests, resolving within 30 hours of stopping and recurring with reexposure 1 week and again 1 year later).
- in 't Veld BA, Slappendel AM, Feenstra J, Veen C, van Aken J, Runhaar EA, Stricker BH. Fever attributed to the use of hydroxyurea. Neth J Med. 1997;51:110–3. [PubMed: 9360411](3 patients with essential thrombocythemia, 2 men and 1 woman, ages 67 to 70 years, developed fever [39-40 oC] within 1-3 weeks of starting hydroxyurea accompanied by constitutional symptoms, resolving rapidly on stopping and recurring rapidly on restarting hydroxyurea; no mention of liver enzymes or jaundice).
- van der Klooster JM, Sucec PM, Stiegelis WF, Hagenbeek A. Fever caused by hydroxyurea: a report of three cases and review of the literature. Neth J Med. 1997;51:114–8. [PubMed: 9360412](3 patients with myeloproliferative syndromes, 2 men and 1 woman, ages 54 to 80 years, developed fever [39-40 oC] 2-4 weeks after starting hydroxyurea, resolving rapidly with stopping and recurring upon reexposure; two patients had mild liver enzyme abnormalities as well [bilirubin 1.1 mg/dL, ALT 108-124 U/L, Alk P 104-140 U/L]).
- Westerman DA, Schwarer A, Grigg AP. Hydroxyurea-induced fever and hepatitis. Aust N Z J Med. 1998;28:657–9. [PubMed: 9847957](Four adult patients with myeloproliferative disorders [ages 45 to 68 years] developed fever [39-41 oC] and hepatitis 3 weeks after starting hydroxyurea therapy [bilirubin 1.0, 1.5, 3.5 and 8.2 mg/dL, ALT 44, 208, 271, and 366 U/L, Alk P 530, 784, 909, and 1047 U/L], fever resolving within 24 hours of stopping and liver abnormalities within one month, with recurrence of fever within hours of reexposure).
- Rutschmann OT, Opravil M, Iten A, Malinverni R, Vernazza PL, Bucher HC, Bernasconi E, et al. A placebo-controlled trial of didanosine plus stavudine, with and without hydroxyurea, for HIV infection. The Swiss HIV Cohort Study. AIDS. 1998;12:F71–7. [PubMed: 9631134](Controlled trial of hydroxyurea vs placebo in 145 patients with HIV infection on didanosine and stavudine found no excess toxicity with addition of hydroxyurea, no mention of ALT elevations, hepatitis, liver failure or drug fever).
- Gwilt PR, Tracewell WG. Pharmacokinetics and pharmacodynamics of hydroxyurea. Clin Pharmacokinet. 1998;34:347–58. [PubMed: 9592619](Hydroxyurea is hydroxylated analogue of urea and suppresses DNA replication by inhibition of ribonucleotide reductase, a necessary step in deoxyribonucleic acid synthesis; its hepatic metabolism is not well characterized, but is probably via the cytochrome P450 system; discussion of side effects mentions liver enzyme elevations).
- Cheung AY, Browne B, Capen C. Hydroxyurea-induced fever in cervical carcinoma: case report and review of the literature. Cancer Invest. 1999;17:245–8. [PubMed: 10225002](52 year old woman with cervical cancer developed cyclic episodes of fever 4 weeks after starting hydroxyurea, stopping only with permanent discontinuation [eosinophils eventually rising to 14% with the third episode]).
- Weissman SB, Sinclair GI, Green CL, Fissell WH. Hydroxyurea-induced hepatitis in human immunodeficiency virus-positive patients. Clin Infect Dis. 1999;29:223–4. [PubMed: 10433603](Two patients with HIV infection developed liver injury 2-3 months after adding hydroxyurea to an antiretroviral regimen of didanosine, stavudine and a protease inhibitor; a 45 year old woman developed acute liver failure [bilirubin 20 mg/dL, ALT 1245 U/L, Alk P 178 U/L] and died, and a 42 year old man developed mild jaundice [bilirubin 3.8 mg/dL, ALT 197 U/L, Alk P 166 U/L] and recovered slowly after stopping all drugs, and was later able to restart the antiretroviral regimen).
- Shuster J. Hydroxyurea and hepatitis. Nursing. 2000;30:77. [PubMed: 10855204](Commentary on Weissman [1999] discusses the hepatotoxicity of the combination of hydroxyurea with antiretroviral agents).
- Tsurumi H, Goto H, Hara T, Moriwaki H. Hydroxyurea-induced fever in a patient with chronic myelogenous leukemia. Int J Hematol. 2000;72:386–7. [PubMed: 11186000](57 year old man with CML developed fever and leg edema within a few months of starting hydroxyurea [albumin 2.1 g/dL], which persisted despite stopping interferon and resolved rapidly with stopping hydroxyurea, albumin levels slowly rising thereafter).
- Rutschmann OT, Vernazza PL, Bucher HC, Opravil M, Ledergerber B, Telenti A, Malinverni R, et al. Long-term hydroxyurea in combination with didanosine and stavudine for the treatment of HIV-1 infection. Swiss HIV Cohort Study. AIDS. 2000;14:2145–51. [PubMed: 11061656](Among 102 patients treated with hydroxyurea, didanosine and stavudine, only 24% remained on therapy long term, adverse events being common including fatigue, headache, neuropathy and thrombocytopenia; ALT or AST elevations occurred in 58% of patients receiving hydroxyurea vs 50% of those on didanosine and stavudine alone).
- Braester A, Quitt M. Hydroxyurea as a cause of drug fever. Acta Haematol. 2000;104:50–1. [PubMed: 11111124](64 year old woman with essential thrombocytosis developed fever without liver test abnormalities 3 weeks after starting hydroxyurea, which resolved rapidly after stopping).
- Pavic M, Sève P, Le Scanff J, Gomard E, Charhon A, Broussolle C. Rev Med Interne. 2004;25:603. [An uncommon case of hydroxyurea-induced fever] French. [PubMed: 15276294](75 year old woman with polycythemia vera developed high fevers within 3 weeks of starting hydroxyurea, which resolved rapidly upon stopping and recurred within 12 hours of restarting; no mention of serum enzyme elevations).
- Randi ML, Ruzzon E, Tezza F, Luzzatto G, Fabris F. Toxicity and side effects of hydroxyurea used for primary thrombocythemia. Platelets. 2005;16:181–4. [PubMed: 16011962](Among 152 patients with thrombocytosis treated with hydroxyurea [for a median of 8.3 years] at a single referral center, notable side effects included 5 patients with macrocytic anemia, 2 drug fever, 2 allergic reactions, 4 leg ulcers and 3 leukemia or myelodysplasia; no mention of ALT elevations or hepatotoxicity).
- Hallam MJ, Kolesar JM. Hydroxyurea induced acute elevations in liver function tests. J Oncol Pharm Pract. 2008;14:61–3. [PubMed: 18337443](82 year old man with polycythemia vera developed nausea and fever 8 days after starting hydroxyurea, which resolved rapidly on stopping and recurred with liver test abnormalities on restarting [bilirubin 1.5 mg/dL, AST 50 U/L, Alk P 353 U/L], resolving within 7 days of stopping).
- Lanzkron S, Strouse JJ, Wilson R, Beach MC, Haywood C, Park H, Witkop C, et al. Systematic review: Hydroxyurea for the treatment of adults with sickle cell disease. Ann Intern Med. 2008;148:939–55. [PMC free article: PMC3256736] [PubMed: 18458272](Systematic review of the efficacy and safety of hydroxyurea in the therapy of sickle cell disease discusses embryotoxicity, myelosuppression and potential carcinogenesis of hydroxyurea, but does not mention ALT elevations or hepatotoxicity).
- Brawley OW, Cornelius LJ, Edwards LR, Gamble VN, Green BL, Inturrisi C, James AH, et al. National Institutes of Health Consensus Development Conference statement: hydroxyurea treatment for sickle cell disease. Ann Intern Med. 2008;148:932–8. [PubMed: 18458271](Consensus statement on use of hydroxyurea in patients with sickle cell disease).
- Platt OS. Hydroxyurea for the treatment of sickle cell anemia. N Engl J Med. 2008;358:1362–9. [PubMed: 18367739](Review of the mechanism of action, efficacy and safety of hydroxyurea therapy of sickle cell disease mentions potential of embryotoxicity, myelotoxicity and cancer, but does not discuss ALT elevations or hepatotoxicity).
- Rees DC, Williams TN, Gladwin MT. Sickle-cell disease. Lancet. 2010;376(9757):2018–31. [PubMed: 21131035](Review of the pathogenesis, clinical features, natural history, complications, management and therapy of sickle cell disease).
- Italia KY, Jijina FF, Jain D, Merchant R, Nadkarni AH, Mukherjee M, Ghosh K, et al. The effect of UGT1A1 promoter polymorphism on bilirubin response to hydroxyurea therapy in hemoglobinopathies. Clin Biochem. 2010;43:1329–32. [PubMed: 20709051](Genetic analyses of 112 patients with hemoglobinopathies receiving hydroxyurea found higher total bilirubin levels in patients with [TA]7/[TA]7 repeats, typical of Gilbert syndrome).
- Steinberg MH, McCarthy WF, Castro O, Ballas SK, Armstrong FD, Smith W, Ataga K, et al. Investigators of the Multicenter Study of Hydroxyurea in Sickle Cell Anemia and MSH Patients' Follow-Up. The risks and benefits of long-term use of hydroxyurea in sickle cell anemia: A 17.5 year follow-up. Am J Hematol. 2010;85:403–8. [PMC free article: PMC2879711] [PubMed: 20513116](Long term follow up of patients with sickle cell disease in a clinical trial of hydroxyurea found evidence of improved survival without apparent severe adverse events; liver disease occurred in 6% of patients and was less in hydroxyurea treated subjects and person who survived more than 10 years).
- Ebert EC, Nagar M, Hagspiel KD. Gastrointestinal and hepatic complications of sickle cell disease. Clin Gastroenterol Hepatol. 2010;8:483–9. [PubMed: 20215064](Review of the liver complications of sickle cell disease mentions hepatic crises, infarction, viral hepatitis, iron overload, and nodular regenerative hyperplasia, but not drug induced liver injury).
- Miller ST, Rey K, He J, Flanagan J, Fish BJ, Rogers ZR, Wang WC, Ware RE., BABY HUG Investigators. Massive accidental overdose of hydroxyurea in a young child with sickle cell anemia. Pediatr Blood Cancer. 2012;59:170–2. [PMC free article: PMC3193862] [PubMed: 21744485](A 2 year old child with sickle cell disease on long term hydroxyurea ingested an entire bottle of drug [~612 mg/kg], but remained well and asymptomatic during follow up with no change in serum ALT and only mild decrease in white blood cell counts, later restarting hydroxyurea).
- Antonioli E, Guglielmelli P, Pieri L, Finazzi M, Rumi E, Martinelli V, Vianelli N, et al. AGIMM Investigators. Hydroxyurea-related toxicity in 3,411 patients with Ph'-negative MPN. Am J Hematol. 2012;87:552–4. [PubMed: 22473827](Retrospective analysis of side effects of hydroxyurea therapy in 3411 patients treated in multiple Italian centers between 1980 and 2000, found notable side effects in 184 [5%], including 16 with fever, 167 with skin ulcers and one with pneumonitis; no mention of ALT elevations or hepatotoxicity).
- Hua J, Iwaki Y, Inoue M, Hagihara M. Tumor lysis syndrome soon after treatment with hydroxyurea followed by nilotinib in two patients with chronic-phase chronic myelogenous leukemia. Int J Hematol. 2013;98:243–6. [PubMed: 23649869](Two patients with CML developed tumor lysis syndrome 1 and 4 days after starting nilotinib, both having been pretreated with hydroxyurea to decrease the white count; the first patient recovering and subsequently tolerating hydroxyurea and nilotinib treatment without recurrence; the second patient developing renal insufficiency followed by acute hepatic necrosis [bilirubin 4.4 mg/dL, ALT 1031 U/L], disseminated intravascular coagulation and multiorgan failure and death).
- Doutrelon C, Lazaro E, Ribeiro E, Greib C, Pellegrin JL, Viallard JF. Rev Med Interne. 2015;36(2):73–7. [Hydrocycarbamide induced fever: Four cases and literature review.] French. [PubMed: 24406312](Description of 4 new cases of hydroxyurea induced fever and review of the literature identified 42 cases, mean age 65 years, median onset at 21 days, one third with accompanying hepatitis or pulmonary complications).
- Shimizu T, Mori T, Karigane D, Kikuchi T, Koda Y, Toyama T, Nakajima H, et al. Rinsho Ketsueki. 2014;55:125–9. [Hydroxyurea (hydroxycarbamide)-induced hepatic dysfunction confirmed by drug-induced lymphocyte stimulation test] Japanese. [PubMed: 24492045](Abstract only: 62 year old man with myelodysplastic syndrome developed fever and nausea 8 days after starting hydroxyurea [bilirubin not given, ALT 5098 U/L], with resolution within 2 weeks of stopping).
- Malik A, Merchant C, Rao M, Fiore RP. Rare but lethal hepatopathy-sickle cell intrahepatic cholestasis and management strategies. Am J Case Rep. 2015;16:840–3. [PMC free article: PMC4671447] [PubMed: 26613743](31 year old man with sickle cell disaese developed a vaso-occlusive crises with abdominal pain and jaundiced [bilirubin 4.0 rising to 50 mg/dL, ALT 78 U/L, Alk P 274 U/L]).
- Barrier A, Willy S, Slone JS. Extramedullary hematopoiesis of the liver in a child with sickle cell disease: a rare complication. Pediatr Int. 2015;57:770–2. [PubMed: 26171586](7 year old girl with sickle cell disease with large hepatic mass was found to be due to severe extramedullary hematopoiesis, dying of respiratory failure despite treatment with hydroxyurea and blood transfusions).
- Chalasani N, Bonkovsky HL, Fontana R, Lee W, Stolz A, Talwalkar J, Reddy KR, et al. United States Drug Induced Liver Injury Network. Features and outcomes of 899 patients with drug-induced liver injury: The DILIN Prospective Study. Gastroenterology. 2015;148:1340–52. [PMC free article: PMC4446235] [PubMed: 25754159](Among 899 cases of drug induced liver injury enrolled in a US prospective study between 2004 and 2013, none were attributed to hydroxyurea).
- Koh C, Turner T, Zhao X, Minniti CP, Feld JJ, Simpson J, Demino M, et al. Liver stiffness increases acutely during sickle cell vaso-occlusive crisis. Am J Hematol. 2013;88:E250–4. [PMC free article: PMC3808506] [PubMed: 23828202](Among 23 patients with sickle cell disease evaluated before and during an acute vaso-occlusive crisis, serum liver enzyme elevations did not change appreciably but hepatic stiffness increased [measured by ultrasound transient elastography] as did serum total and indirect bilirubin and reticulocyte counts, while serum albumin and hemoglobin decreased).
- Feld JJ, Kato GJ, Koh C, Shields T, Hildesheim M, Kleiner DE, Taylor JG 6th, et al. Liver injury is associated with mortality in sickle cell disease. Aliment Pharmacol Ther. 2015;42:912–21. [PMC free article: PMC6478018] [PubMed: 26235444](Among 247 patients with sickle cell disease, liver disease was common, elevations in ALT were present in 16% and alkaline phosphatase in 33%; factors associated with mortality during follow up were iron indices [serum ferritin, transferrin, and iron] and liver abnormalities [direct bilirubin, albumin and alkaline phosphatase levels]; liver biopsy done in 40 patients revealed nodular regenerative hyperplasia in 36% and portal venopathy in 23%).
- Fitzhugh CD, Hsieh MM, Allen D, Coles WA, Seamon C, Ring M, Zhao X, et al. Hydroxyurea-increased fetal hemoglobin is associated with less organ damage and longer survival in adults with sickle cell anemia. PLoS One. 2015;10:e0141706. [PMC free article: PMC4648496] [PubMed: 26576059](Among 383 adults with sickle cell disease followed for up to 19 years [median=2.6 years], 59 [15%] died largely from pulmonary or cardiac disease, sickle crises or infections, and use of higher doses of hydroxyurea were associated with higher HbF levels, lower ALT values and better survival).
- Malik A, Merchant C, Rao M, Fiore RP. Rare but lethal hepatopathy-sickle cell intrahepatic cholestasis and management strategies. Am J Case Rep. 2015;16:840–3. [PMC free article: PMC4671447] [PubMed: 26613743](31 year old man with sickle cell disease presented with a severe vaso-occlusive crisis, right upper quadrant pain and marked jaundice [total bilirubin 50 mg/dL, direct 38 mg/dL, ALT 40 U/L, AST 155 U/L, Alk P 320 U/L], eventually recovering with blood transfusions and supportive care).
- Tisdale JF, Thein SL, Eaton WA. Treating sickle cell anemia. Science. 2020;367(6483):1198–9. [PMC free article: PMC7299198] [PubMed: 32165573](Review of mechanism of action and efficacy of current [hydroxyurea and voxelotor] and the promise of future therapies of sickle cell anemia [including bone marrow transplantation and gene therapy], mentions that the increase in HbF induced by hydroxyurea dilutes HbS concentrations making sickling less likely to occur in the time of transit of red cells through the microvasculature).
- Osunkwo I, Manwani D, Kanter J. Current and novel therapies for the prevention of vaso-occlusive crisis in sickle cell disease. Ther Adv Hematol. 2020;11:2040620720955000. [PMC free article: PMC7534097] [PubMed: 33062233](Review of the pathogenesis of vaso-occlusive crises in sickle cell disease and drugs that target different components of the multifactorial process including increasing fetal hemoglobin [hydroxyurea], decreasing oxidative stress [L-glutamine], increasing oxygen affinity of hemoglobin [voxelotor], and decreasing adhesion of sickled cells to platelets, neutrophils and endothelium [crizanlizumab]; no mention of ALT elevations with therapy or hepatotoxicity).
- Darbari DS, Sheehan VA, Ballas SK. The vaso-occlusive pain crisis in sickle cell disease: definition, pathophysiology, and management. Eur J Haematol. 2020;105:237–46. [PubMed: 32301178](Extensive review of the pathogenesis of vaso-occlusive crisis in patients with sickle cell disease and therapies that target different steps in the process including inflammation, adhesion, oxidative stress and oxygen affinity and stability of hemoglobin; discusses efficacy of L-glutamine, voxelotor and crizanlizumab, mentioning that all three are well tolerated; no mention or discussion of hepatotoxicity).
- PMCPubMed Central citations
- PubChem SubstanceRelated PubChem Substances
- PubMedLinks to PubMed
- Augmentation by erythropoietin of the fetal-hemoglobin response to hydroxyurea in sickle cell disease.[N Engl J Med. 1993]Augmentation by erythropoietin of the fetal-hemoglobin response to hydroxyurea in sickle cell disease.Rodgers GP, Dover GJ, Uyesaka N, Noguchi CT, Schechter AN, Nienhuis AW. N Engl J Med. 1993 Jan 14; 328(2):73-80.
- Sustained long-term hematologic efficacy of hydroxyurea at maximum tolerated dose in children with sickle cell disease.[Blood. 2004]Sustained long-term hematologic efficacy of hydroxyurea at maximum tolerated dose in children with sickle cell disease.Zimmerman SA, Schultz WH, Davis JS, Pickens CV, Mortier NA, Howard TA, Ware RE. Blood. 2004 Mar 15; 103(6):2039-45. Epub 2003 Nov 20.
- Treatment of sickle cell anemia with hydroxyurea and erythropoietin.[N Engl J Med. 1990]Treatment of sickle cell anemia with hydroxyurea and erythropoietin.Goldberg MA, Brugnara C, Dover GJ, Schapira L, Charache S, Bunn HF. N Engl J Med. 1990 Aug 9; 323(6):366-72.
- Review Hydroxyurea induction of fetal hemoglobin synthesis in sickle-cell disease.[Semin Oncol. 1992]Review Hydroxyurea induction of fetal hemoglobin synthesis in sickle-cell disease.Dover GJ, Charache S. Semin Oncol. 1992 Jun; 19(3 Suppl 9):61-6.
- Review Hydroxyurea therapy: improving the lives of patients with sickle cell disease.[Pediatr Nurs. 2006]Review Hydroxyurea therapy: improving the lives of patients with sickle cell disease.Anderson N. Pediatr Nurs. 2006 Nov-Dec; 32(6):541-3.
- Hydroxyurea - LiverToxHydroxyurea - LiverTox
Your browsing activity is empty.
Activity recording is turned off.
See more...