NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
LiverTox: Clinical and Research Information on Drug-Induced Liver Injury [Internet]. Bethesda (MD): National Institute of Diabetes and Digestive and Kidney Diseases; 2012-.

LiverTox: Clinical and Research Information on Drug-Induced Liver Injury [Internet].
Show detailsOVERVIEW
Introduction
Lenvatinib is orally available multi-kinase inhibitor and antineoplastic agent that is used in treatment of advanced, metastatic medullary thyroid cancer and refractory renal cell carcinoma. Lenvatinib is associated with a modest rate of serum enzyme elevations during treatment and has been implicated to rare instances of clinically apparent, acute liver injury some of which have been fatal.
Background
Lenvatinib (len va' ti nib) is an orally available, small molecule, multi-kinase inhibitor with activity against vascular endothelial growth factor receptor (VEGFR) 1, 2 and 3 as well as fibroblast growth factor (FGF) 1, 2, 3 and 4, platelet derived growth factor receptor (PDGFR) alpha, cKit and the RET proto-oncogene. Several of these receptors are overexpressed in cancer cells and can cause unregulated cell growth. Lenvatinib has been evaluated as therapy of several forms of advanced and metastatic carcinomas and has shown efficacy in thyroid and renal cell carcinoma. Lenvatinib received accelerated approval for use in the United States in 2015 for therapy of metastatic, refractory thyroid cancer after failure of other therapies. Indications were expanded in 2016 to include advanced, refractory renal cell carcinoma. Lenvatinib is available as capsules of 4 and 10 mg under the brand name Lenvima. The recommended dose for thyroid cancer is 24 mg orally once daily and for renal cell cancer is 18 mg (in combination with 5 mg of everolimus) orally once daily. Side effects are common and can include hypertension, fatigue, diarrhea, nausea, vomiting, anorexia, weight loss, abdominal pain, stomatitis, headache, joint and muscle pain, peripheral edema, cough, dyspnea, rash, hemorrhagic events and proteinuria. Other uncommon, but potentially severe side effects include severe hypertension, heart failure, arterial thrombotic events, proteinuria, severe diarrhea, renal impairment, gastrointestinal perforation or fistulae, prolongation of the QTc interval, hypocalcemia, reversible posterior leukoencephalopathy and embryo-fetal toxicity.
Hepatotoxicity
In large clinical trials of lenvatinib, elevations in serum aminotransferase levels were common, occurring in 52% of patients. Values greater than 5 times the upper limit of normal (ULN), however, occurred in only 3% to 5% of recipients. Serum alkaline phosphatase elevations were also common occurring in 28% of patients and were above 3 times ULN in 2%. In addition, fatal hepatic failure was reported in 3 of 1160 patients treated in preregistration clinical trials and another patient developed symptomatic but self-limited acute hepatitis with jaundice. The degree of relatedness of these events to lenvatinib therapy, however, was not defined. In the product label for lenvatinib, serum ALT, AST and alkaline phosphatase elevations are listed as adverse reactions, and acute hepatitis is mentioned as a rare occurrence. Monitoring of serum enzymes before, every 2 weeks for 2 months and monthly thereafter during treatment is recommended with dose reduction or discontinuation depending upon the degree and persistence of the abnormalities.
Likelihood score: D (possible cause of clinically apparent liver injury).
Mechanism of Injury
The mechanism of liver injury accounting for serum enzyme elevations during lenvatinib therapy is not known, but injury may be a direct effect of inhibition of cellular kinases by this multi-specific tyrosine kinase inhibitor. Lenvatinib is metabolized in the liver, predominantly by the cytochrome P 450 system and specially by CYP 3A4. Nevertheless, lenvatinib is not significantly affected by CYP 3A4 inducers or inhibitors or to cause clinically relevant drug-drug interactions.
Outcome and Management
Routine monitoring of liver tests before and periodically throughout treatment with lenvatinib is recommended. Serum aminotransferase elevations above 5 times the upper limit of normal (if confirmed) should lead to dose reduction or temporary cessation. Clinically apparent liver injury should prompt immediate interruption of lenvatinib therapy. There is little information on cross reactivity in risk for hepatic injury between lenvatinib and other protein kinase inhibitors.
Drug Class: Antineoplastic Agents, Protein Kinase Inhibitors
Related Drugs: Everolimus
PRODUCT INFORMATION
REPRESENTATIVE TRADE NAMES
Lenvatinib – Lenvima®
DRUG CLASS
Antineoplastic Agents
Product labeling at DailyMed, National Library of Medicine, NIH
CHEMICAL FORMULA AND STRUCTURE
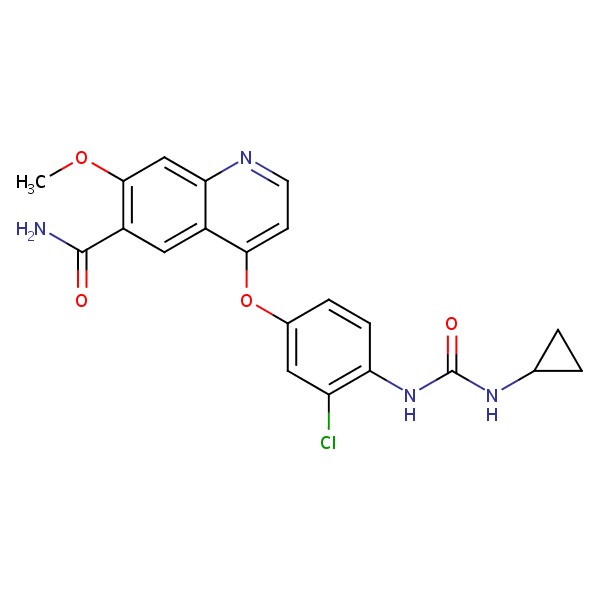
| DRUG | CAS REGISTRY NO. | MOLECULAR FORMULA | STRUCTURE |
|---|---|---|---|
| Lenvatinib | 417716-92-8 | C21-H19-Cl-N4-O4 |
 |
ANNOTATED BIBLIOGRAPHY
References updated: 01 June 2017
- Zimmerman HJ. Hepatotoxicity: the adverse effects of drugs and other chemicals on the liver. 2nd ed. Philadelphia: Lippincott, 1999.(Review of hepatotoxicity published in 1999 before the availability of kinase inhibitors such as lenvatinib).
- DeLeve LD. Kinase inhibitors. Cancer chemotherapy. In, Kaplowitz N, DeLeve LD, eds. Drug-induced liver disease. 3rd ed. Amsterdam: Elsevier, 2013, pp. 556-7.(Review of hepatotoxicity of cancer chemotherapeutic agents including the kinase inhibitors gefitinib, erlotinib and crizotinib; lenvatinib is not discussed).
- Wellstein A, Giaccone G, Atkins MB, Sausville EA. Targeted therapies: monoclonal antibodies, protein kinase inhibitors, and various small molecules. In, Brunton LL, Hilal-Dandan R, Knollman BC, eds. Goodman & Gilman's the pharmacological basis of therapeutics. 13th ed. New York: McGraw-Hill, 2018, pp. 1203-36.(Textbook of pharmacology and therapeutics).
- Boss DS, Glen H, Beijnen JH, Keesen M, Morrison R, Tait B, Copalu W, et al. A phase I study of E7080, a multitargeted tyrosine kinase inhibitor, in patients with advanced solid tumours. Br J Cancer 2012; 106: 1598-604. [PMC free article: PMC3349182] [PubMed: 22516948](Among 82 patients with various forms of advanced cancer who received escalating doses of lenvatinib, objective responses occurred in 7 patients [9%] including 4 of 9 with renal cell cancer, while adverse events included hypertension, diarrhea, nausea, vomiting and stomatitis; no mention of ALT elevations or hepatotoxicity).
- Molina AM, Hutson TE, Larkin J, Gold AM, Wood K, Carter D, Motzer R, et al. A phase 1b clinical trial of the multi-targeted tyrosine kinase inhibitor lenvatinib (E7080) in combination with everolimus for treatment of metastatic renal cell carcinoma (RCC). Cancer Chemother Pharmacol 2014; 73: 181-9. [PMC free article: PMC3889692] [PubMed: 24190702](Among 27 patients with metastatic, refractory renal cell cancer treated with lenvatinib and everolimus, objective responses occurred in 6 [33%] and adverse events were common; no mention of ALT elevations or hepatotoxicity).
- Cabanillas ME, Schlumberger M, Jarzab B, Martins RG, Pacini F, Robinson B, McCaffrey JC, et al. A phase 2 trial of lenvatinib (E7080) in advanced, progressive, radioiodine-refractory, differentiated thyroid cancer: A clinical outcomes and biomarker assessment. Cancer 2015; 121: 2749-56. [PMC free article: PMC4803478] [PubMed: 25913680](Among 58 patients with advanced refractory thyroid cancer treated with lenvatinib [24 mg daily], the objective response rate was 50%, but adverse events were common with more than half developing hypertension, weight loss, diarrhea, proteinuria, fatigue and anorexia; no mention of ALT elevations or hepatotoxicity).
- Schlumberger M, Tahara M, Wirth LJ, Robinson B, Brose MS, Elisei R, Habra MA, et al. Lenvatinib versus placebo in radioiodine-refractory thyroid cancer. N Engl J Med 2015; 372: 621-30. [PubMed: 25671254](Among 261 patients with progressive and refractory thyroid cancer treated with lenvatinib [24 mg daily] or placebo, median progression free survival was improved by lenvatinib [18.3 vs 3.6 months], although side effects were frequent and sometimes severe; liver failure was report in 0.4% of recipients).
- Lenvatinib (Lenvima) for thyroid cancer. Med Lett Drugs Ther 2015; 57 (1475): e120-1. [PubMed: 26262885](Concise review of the mechanism of action, clinical efficacy, safety and costs of lenvatinib shortly after its approval for use in advanced, refractory thyroid cancer; mentions that side effects led to dose reductions in 68% of patients and discontinuation in 18%, and that adverse events included hepatotoxicity and fatal hepatic failure).
- PMCPubMed Central citations
- PubChem SubstanceRelated PubChem Substances
- PubMedLinks to PubMed
- Review Cabozantinib.[LiverTox: Clinical and Researc...]Review Cabozantinib.. LiverTox: Clinical and Research Information on Drug-Induced Liver Injury. 2012
- Review Lenvatinib: Role in thyroid cancer and other solid tumors.[Cancer Treat Rev. 2016]Review Lenvatinib: Role in thyroid cancer and other solid tumors.Cabanillas ME, Habra MA. Cancer Treat Rev. 2016 Jan; 42:47-55. Epub 2015 Dec 2.
- NEOADJUVANT LENVATINIB IN ADVANCED UNRESECTABLE MEDULLARY THYROID CARCINOMA: A CASE REPORT.[AACE Clin Case Rep. 2020]NEOADJUVANT LENVATINIB IN ADVANCED UNRESECTABLE MEDULLARY THYROID CARCINOMA: A CASE REPORT.Golingan H, Hunis B, Golding AC, Bimston DN, Harrell RM. AACE Clin Case Rep. 2020 Mar-Apr; 6(2):e73-e78. Epub 2019 Dec 20.
- Response to Lenvatinib in Children with Papillary Thyroid Carcinoma.[Thyroid. 2018]Response to Lenvatinib in Children with Papillary Thyroid Carcinoma.Mahajan P, Dawrant J, Kheradpour A, Quintanilla NM, Lopez ME, Orth RC, Athanassaki I, Venkatramani R. Thyroid. 2018 Nov; 28(11):1450-1454. Epub 2018 Oct 16.
- Lenvatinib, everolimus, and the combination in patients with metastatic renal cell carcinoma: a randomised, phase 2, open-label, multicentre trial.[Lancet Oncol. 2015]Lenvatinib, everolimus, and the combination in patients with metastatic renal cell carcinoma: a randomised, phase 2, open-label, multicentre trial.Motzer RJ, Hutson TE, Glen H, Michaelson MD, Molina A, Eisen T, Jassem J, Zolnierek J, Maroto JP, Mellado B, et al. Lancet Oncol. 2015 Nov; 16(15):1473-1482. Epub 2015 Oct 22.
- Lenvatinib - LiverToxLenvatinib - LiverTox
Your browsing activity is empty.
Activity recording is turned off.
See more...