NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
LiverTox: Clinical and Research Information on Drug-Induced Liver Injury [Internet]. Bethesda (MD): National Institute of Diabetes and Digestive and Kidney Diseases; 2012-.

LiverTox: Clinical and Research Information on Drug-Induced Liver Injury [Internet].
Show detailsOVERVIEW
Introduction
Vandetanib is a multi-kinase inhibitor that is used in the therapy of advanced or metastatic medullary thyroid cancer. Vandetanib therapy is commonly associated with transient elevations in serum aminotransferase during therapy, but has not been linked to cases of clinically apparent acute liver injury with jaundice.
Background
Vandetanib (van det’ a nib) is an orally available, multi-kinase inhibitor with activity against vascular endothelial growth factor (VEGF) and epidermal growth factor (EGF) receptor families as well as RET (rearranged-during-transfection), BRK, TIE2 and Src kinases. Vandetanib has potent anti-angiogenesis activity and specific potency against mutant RET tyrosine kinases that are found in most hereditary and a large proportion of spontaneous medullary thyroid cancers. Clinical trials of vandetanib in advanced or metastatic medullary thyroid cancer have documented significant prolongation of progression free survival. Vandetanib received approval for use in the United States in 2011 and current indications are for symptomatic or progressive, unresectable or metastatic medullary thyroid cancer. Vandetanib is available in tablets of 100 and 300 mg under the brand name Caprelsa, and the recommended initial dose is 300 mg once daily. Side effects are common and can be problematic and even fatal. The most frequent adverse events include diarrhea, nausea, fatigue, rash, acne, hypertension, headache, anorexia and abdominal pain. Less common, but potentially severe side effects include prolongation of the QTc interval, heart failure, sudden death, severe skin toxicity, Stevens Johnson syndrome, interstitial lung disease, hemorrhage, ischemic cerebrovascular events, reversible posterior leukoencephalopathy syndrome and embryo-fetal toxicity. Vandetanib is available only through a restricted distribution program that requires certification and regular monitoring.
Hepatotoxicity
In large clinical trials of vandetanib, abnormalities in routine liver tests were common with serum aminotransferase elevations, occurring in up to half of patients and rising above 5 times the upper limit of normal (ULN) 2% to 5% of patients. In prelicensure trials of vandetanib in thyroid cancer, there were no reports of clinically apparent liver injury with jaundice or hepatic failure. Since approval and more wide scale use, there have been no published reports of hepatotoxicity due to vandetanib and the product label does not include discussion of hepatotoxicity. However, many of the kinase inhibitors used in cancer chemotherapy have been implicated in cases of clinically apparent liver injury which typically arises within the first 2 to 12 weeks of therapy, presenting with symptoms of fatigue, nausea and jaundice and a hepatocellular pattern of serum enzyme elevations without immunoallergic or autoimmune features. Several tyrosine kinase inhibitors (imatinib, nilotinib) have also been implicated in causing reactivation of hepatitis B.
Likelihood score: E* (unproven but suspected rare cause of clinically apparent liver injury).
Mechanism of Injury
The mechanism of injury accounting for serum enzyme elevations during vandetanib therapy is not known. Vandetanib has a long plasma half life (~19 days). Small amounts are metabolized in the liver through the CYP 3A4 pathway and it is susceptible to drug-drug interactions with strong inducers or inhibitors of hepatic CYP 3A4 activity.
Outcome and Management
In using kinase inhibitors to the therapy of cancer, routine monitoring of liver tests before and during therapy is warranted. Serum aminotransferase elevations above 5 times the upper limit of normal (if confirmed) or any elevations accompanied by jaundice or symptoms should lead to temporary cessation. Vantetanib should be restarted only if serum enzyme abnormalities resolve or improve and only with careful monitoring. There does not appear to be cross reactivity in risk for hepatic injury between vandetanib and other tyrosine kinase inhibitors.
Drug Class: Antineoplastic Agents, Protein Kinase Inhibitors
PRODUCT INFORMATION
REPRESENTATIVE TRADE NAMES
Vandetanib – Generic, Caprelsa®
DRUG CLASS
Antineoplastic Agents
Product labeling at DailyMed, National Library of Medicine, NIH
CHEMICAL FORMULA AND STRUCTURE
| DRUG | CAS REGISTRY NO. | MOLECULAR FORMULA | STRUCTURE |
|---|---|---|---|
| Vandetanib | 443913-73-3 | C22-H24-Br-F-N4-O2 |
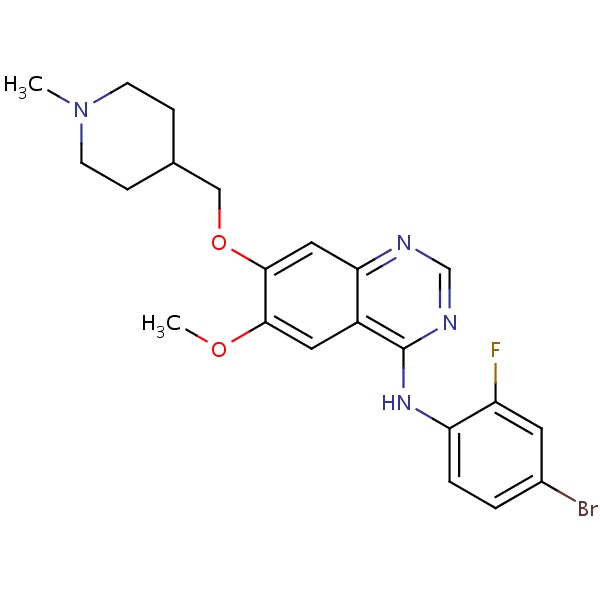 |
ANNOTATED BIBLIOGRAPHY
References updated: 28 June 2018
- Zimmerman HJ. Hepatotoxicity: the adverse effects of drugs and other chemicals on the liver. 2nd ed. Philadelphia: Lippincott, 1999.(Review of hepatotoxicity published in 1999 before the availability of tyrosine kinase receptor inhibitors such as vandetanib).
- DeLeve LD. Erlotinib. Cancer chemotherapy. In, Kaplowitz N, DeLeve LD, eds. Drug-induced liver disease. 3rd ed. Amsterdam: Elsevier, 2013, pp. 556.(Review of hepatotoxicity of cancer chemotherapeutic agents discusses several tyrosine kinase inhibitors including imatinib, gefitinib, erlotinib and crizotinib, but not vandetanib).
- Chabner BA, Barnes J, Neal J, Olson E, Mujagic H, Sequist L, Wilson W, et al. Targeted therapies: tyrosine kinase inhibitors, monoclonal antibodies, and cytokines. In, Brunton LL, Chabner BA, Knollman BC, eds. Goodman & Gilman's the pharmacological basis of therapeutics. 12th ed. New York: McGraw-Hill, 2011, pp. 1731-54.(Textbook of pharmacology and therapeutics).
- Weil A, Martin P, Smith R, Oliver S, Langmuir P, Read J, Molz KH. Pharmacokinetics of vandetanib in subjects with renal or hepatic impairment. Clin Pharmacokinet 2010; 49: 607-18. [PubMed: 20690783](Single dose pharmacokinetics studies in 30 subjects with varying degrees of liver dysfunction showed minimal differences in plasma levels or exposure despite presence of Child Pugh class A, B and C cirrhosis).
- Wells SA Jr, Gosnell JE, Gagel RF, Moley J, Pfister D, Sosa JA, Skinner M, et al. Vandetanib for the treatment of patients with locally advanced or metastatic hereditary medullary thyroid cancer. J Clin Oncol 2010; 28: 767-72. [PMC free article: PMC2834392] [PubMed: 20065189](Among 30 patients with advanced or metastatic hereditary medullary thyroid cancer [with activating RET mutations] treated with vandetanib for an average of 18.8 months, partial responses occurred in 20% of patients and common side effects were hypertension [77%], diarrhea [70%], rash [67%], fatigue [63%] and nausea [63%]; no mention of ALT elevations or hepatotoxicity).
- Leboulleux S, Bastholt L, Krause T, de la Fouchardiere C, Tennvall J, Awada A, Gómez JM, et al. Vandetanib in locally advanced or metastatic differentiated thyroid cancer: a randomised, double-blind, phase 2 trial. Lancet Oncol 2012; 13: 897-905. [PubMed: 22898678](Among 145 patients with advanced or metastatic differentiated thyroid cancer, median progression free survival was 11.1 months in those receiving vandetanib vs 5.9 months with placebo; no mention of ALT elevations or hepatotoxicity, but QTc prolongation occurred in 23%).
- Deshpande HA, Sheth K, Sosa JA, Roman S. Efficacy and tolerability of pharmacotherapy options for the treatment of medullary thyroid cancer. Clin Med Insights Oncol 2012; 6: 355-62. [PMC free article: PMC3489097] [PubMed: 23133319](Review of the rationale for use, mechanism of action, pharmacology, efficacy, safety and cost of vandetanib for medullary thyroid cancer, mentions that ALT elevations were reported in 3-5% of treated patients).
- Wells SA Jr, Robinson BG, Gagel RF, Dralle H, Fagin JA, Santoro M, Baudin E, et al. Vandetanib in patients with locally advanced or metastatic medullary thyroid cancer: a randomized, double-blind phase III trial. J Clin Oncol 2012; 30: 134-41. [PMC free article: PMC3675689] [PubMed: 22025146](Among 331 patients with advanced or metastatic medullary thyroid cancer, median progression free survival was 30.5 months with vandetanib vs 19.3 months with placebo; extensive discussion of adverse events does not mention ALT elevations or hepatotoxicity).
- Vandetanib (Caprelsa) for medullary thyroid cancer. Med Lett Drugs Ther 2012; 54 (1381): 3-4. [PubMed: 22233588](Concise review of the mechanism of action, efficacy, safety and costs of vandetanib for medullary thyroid cancer shortly after its approval in the US, mentions severe adverse events of QTc prolongation, sudden death, skin reactions, photosensitivity and Stevens Johnson syndrome, but not hepatotoxicity or ALT elevations).
- Spraggs CF, Xu CF, Hunt CM. Genetic characterization to improve interpretation and clinical management of hepatotoxicity caused by tyrosine kinase inhibitors. Pharmacogenomics 2013; 14: 541-54. [PubMed: 23556451](Review of genetic associations of serum ALT and bilirubin elevations during therapy with tyrosine kinase inhibitors, focusing on lapatinib and pazopanib).
- Shah RR, Morganroth J, Shah DR. Hepatotoxicity of tyrosine kinase inhibitors: clinical and regulatory perspectives. Drug Saf 2013; 36: 491-503. [PubMed: 23620168](Review of the hepatotoxicity of 18 tyrosine kinase inhibitors approved for use in cancer in the US as of 2013; vandetanib is associated with some degree of ALT elevation in 51% of patients and in elevations above 5 times ULN in 2%, but has not been linked to cases of clinically apparent hepatitis or hepatic failure).
- Ton GN, Banaszynski ME, Kolesar JM. Vandetanib: a novel targeted therapy for the treatment of metastatic or locally advanced medullary thyroid cancer. Am J Health Syst Pharm 2013; 70: 849-55. [PubMed: 23640345](Review of the efficacy and safety of vandetanib as therapy of medullary thyroid cancer does not mention ALT elevations or hepatotoxicity).
- Lacouture ME, Ciccolini K, Kloos RT, Agulnik M. Overview and management of dermatologic events associated with therapies for medullary thyroid cancer. Thyroid 2014; 62: 798-806. [PMC free article: PMC4148058] [PubMed: 24902006](Description of the spectrum of skin toxicities of kinase inhibitors including vandetanib used in treatment of medullary thyroid cancer mentions that inhibition of EGFR signaling causes growth arrest and apoptosis in keratinocytes, with subsequent release of cytokines and recruitment of inflammatory cells).
- Iacovelli R, Palazzo A, Procopio G, Santoni M, Trenta P, De Benedetto A, Mezi S, et al. Incidence and relative risk of hepatic toxicity in patients treated with anti-angiogenic tyrosine kinase inhibitors for malignancy. Br J Clin Pharmacol 2014; 77: 929-38. [PMC free article: PMC4093918] [PubMed: 23981115](Systematic review of liver toxicity reported in controlled trials of anti-VEGFR kinase inhibitors [axitinib, pazopanib, sorafenib, sunitinib, regorafenib and vandetanib] used to treat solid tumors identified 6 articles with 3691 patients, among whom 34% had ALT elevations compared to 24% of controls [above 5 times ULN in 5.2% vs 1.4%], with highest rates for sorafenib and pazopanib).
- Gridelli C, Novello S, Zilembo N, Luciani A, Favaretto AG, De Marinis F, Genestreti G, et al. Phase II randomized study of vandetanib plus gemcitabine or gemcitabine plus placebo as first-line treatment of advanced non-small-cell lung cancer in elderly patients. J Thorac Oncol 2014; 9: 733-7. [PubMed: 24722160](Among 124 patients with advanced non-small cell lung cancer treated with gemcitabine with or without vandetanib, progression free survival was 14 days longer with the combination while adverse event rates were similar in both groups; no mention of ALT elevations or hepatotoxicity).
- Santoro A, Gebbia V, Pressiani T, Testa A, Personeni N, Arrivas Bajardi E, Foa P, et al. A randomized,multicenter, phase II study of vandetanib monotherapy versus vandetanib in combination with gemcitabine versus gemcitabine plus placebo in subjects with advanced biliary tract cancer: the VanGogh study. Ann Oncol 2015; 26: 542-7. [PubMed: 25538178](Among 173 patients with advanced biliary tract cancer treated with gemcitabine or vandetanib or both, progression free survival was smilar in the 3 groups as were adverse event rates; no mention of ALT elevations or hepatotoxicity).
- Zhang N, Liu Y, Jeong H. Drug-drug interaction potentials of tyrosine kinase inhibitors via inhibition of UDP-glucuronosyltransferases. Sci Rep 2015 Dec 8; 5: 17778. [PMC free article: PMC4672351] [PubMed: 26642944](In vitro analysis of effect of tyrosine kinase inhibitors including vandetanib on UDP-glucuronosyltransferases, an interaction that may explain the hyperbilirubinemia that occurs in 5-10% of patients treated with these agents).
- Chougnet CN, Borget I, Leboulleux S, de la Fouchardiere C, Bonichon F, Criniere L, Niccoli P, et al. Vandetanib for the treatment of advanced medullary thyroid cancer outside a clinical trial: results from a French cohort. Thyroid 2015; 25: 386-91. [PubMed: 25627619](Among 60 French patients with medullary thyroid cancer treated with vandetanib in an early access program, partial responses occurred in 20% of subjects but all had at least one adverse event, most commonly skin rash [60%], diarrhea [58%], and fatigue [52%]; no mention of ALT elevations or hepatotoxicity).
- Chalasani N, Bonkovsky HL, Fontana R, Lee W, Stolz A, Talwalkar J, Reddy KR, et al.; United States Drug Induced Liver Injury Network. Features and outcomes of 899 patients with drug-induced liver injury: The DILIN Prospective Study. Gastroenterology 2015; 148: 1340-52.e7. [PMC free article: PMC4446235] [PubMed: 25754159](Among 899 cases of drug induced liver injury enrolled in a US prospective study between 2004 and 2013, 49 were attributed to antineoplastic agents [5.5%], 9 of which were attributed to kinase inhibitors [imatinib=5, lapatinib=2, regorafenib=1], but none to vandetanib).
- Tsang VH, Robinson BG, Learoyd DL. The safety of vandetanib for the treatment of thyroid cancer. Expert Opin Drug Saf 2016; 15: 1107-13. [PubMed: 27301016](Review of the mechanism of action, clinical efficacy and safety of vandetanib as therpay of thyroid cancer, mentions that ALT elevations are common but generally mild and self-limited in course; no mention of clinically apparent liver injury or hepatotoxicity).
- Bunchorntavakul C, Reddy KR. Drug hepatotoxicity: newer agents. Clin Liver Dis 2017; 21: 115-34. [PubMed: 27842767](Review of the hepatotoxicity of recently approved medications including the antineoplastic tyrosine kinase inhibitors such as imatinib, bosutinib, ponatinib, nilotinib, gefitinib, erlotinib, crizotinib, lapatinib, sunitinib, pazopanib, vemurafenib, regorafenib and vandetanib).
- PMCPubMed Central citations
- PubChem SubstanceRelated PubChem Substances
- PubMedLinks to PubMed
- [Efficacy and safety of vandetanib on advanced medullary thyroid carcinoma: single center result from a phase Ⅲ study].[Zhonghua Er Bi Yan Hou Tou Jin...][Efficacy and safety of vandetanib on advanced medullary thyroid carcinoma: single center result from a phase Ⅲ study].Wang SX, Zhang XW, Wang XX, An CM, Zhang YB, Liu W, Zhao YF, He XH, Li ZJ, Niu LJ, et al. Zhonghua Er Bi Yan Hou Tou Jing Wai Ke Za Zhi. 2019 Jun 7; 54(6):439-444.
- Role of vandetanib in the management of medullary thyroid cancer.[Biologics. 2012]Role of vandetanib in the management of medullary thyroid cancer.Brassard M, Rondeau G. Biologics. 2012; 6:59-66. Epub 2012 Mar 8.
- Cabozantinib and vandetanib for unresectable locally advanced or metastatic medullary thyroid cancer: a systematic review and economic model.[Health Technol Assess. 2019]Cabozantinib and vandetanib for unresectable locally advanced or metastatic medullary thyroid cancer: a systematic review and economic model.Tappenden P, Carroll C, Hamilton J, Kaltenthaler E, Wong R, Wadsley J, Moss L, Balasubramanian S. Health Technol Assess. 2019 Feb; 23(8):1-144.
- Review Vandetanib: a novel targeted therapy for the treatment of metastatic or locally advanced medullary thyroid cancer.[Am J Health Syst Pharm. 2013]Review Vandetanib: a novel targeted therapy for the treatment of metastatic or locally advanced medullary thyroid cancer.Ton GN, Banaszynski ME, Kolesar JM. Am J Health Syst Pharm. 2013 May 15; 70(10):849-55.
- Review [Vandetanib, in the management of patients with locally advanced or metastatic medullary thyroid carcinomas].[Bull Cancer. 2014]Review [Vandetanib, in the management of patients with locally advanced or metastatic medullary thyroid carcinomas].Chougnet CN, Schlumberger M, Leboulleux S, Baudin E. Bull Cancer. 2014 Sep; 101(9):891-5.
- Vandetanib - LiverToxVandetanib - LiverTox
Your browsing activity is empty.
Activity recording is turned off.
See more...