NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
LiverTox: Clinical and Research Information on Drug-Induced Liver Injury [Internet]. Bethesda (MD): National Institute of Diabetes and Digestive and Kidney Diseases; 2012-.

LiverTox: Clinical and Research Information on Drug-Induced Liver Injury [Internet].
Show detailsOVERVIEW
Introduction
Vitamin B refers to several water soluble vitamins often found together in foods, all of which are necessary for normal growth and metabolism, but none of which are synthesized in adequate amounts by humans. The common forms of vitamin B include vitamin B1 (thiamine), B2 (riboflavin), B3 (niacin), B6 (pyridoxine) and B12 (cyanocobalamin). Except for niacin (when given in high doses), there is no evidence that the other B vitamins, in physiologic or even super-physiologic high doses cause liver injury or jaundice. The major forms of vitamin B and selected other water soluble vitamins (biotin, pantothenic acid, choline) are discussed briefly in this record.
Vitamin B1, Thiamine
Thiamine (or thiamin) (thye' a min) is a water soluble B vitamin found in whole grains, legumes, yeast, beef and pork. Thiamine was the first B vitamin to be discovered and was given the designation vitamin B1. Thiamine is required in amino acid and carbohydrate metabolism and is active in energy generation reactions. Thiamine deficiency is rare, but can occur in malnourished patients due to chronic alcoholism or cancer chemotherapy with poor dietary intake. More recently, symptomatic thiamine deficiency has been reported in women with hyperemesis gravidarum, patients after gastric bypass surgery and in malnourished patients with intestinal obstruction or malabsorption syndromes. Populations and cultures that rely heavily upon rice based diets are at increased risk of thiamine deficiency. Classic diet related thiamine deficiency causes the symptom complex known as beriberi (“weak, weak”), marked by variable degrees of weight loss, nausea and vomiting, diarrhea, irritability, apathy, muscle weakness and painful peripheral neuropathy. Cardiac dysfunction with right sided heart failure and peripheral edema can also occur and is called “wet” beriberi. Thiamine deficiency can also present with prominent central nervous system symptoms (Wernicke-Korsakoff syndrome), particularly in malnourished patients with chronic alcoholism or on cancer chemotherapy. Wernicke encephalopathy is characterized by mental deterioration, nystagmus, ophthalmoplegia and ataxia; Korsakoff’s syndrome is marked by memory loss, confabulation and psychosis. Acute thiamine deficiency can also cause lactic acidosis. Thiamine is highly water soluble and body stores are not great, for which reason deficiencies can develop rapidly (within weeks to months). The recommended dietary allowance of thiamine is 1.2 mg in adult men and 1.1 mg in adult women, amounts that are provided in the average American diet. Thiamine is available generically in many over-the-counter forms and is included in virtually all multivitamin preparations (typically in concentrations of 0.3 to 1.5 mg). Parenteral thiamine is available (100 mg/mL) and used in parenteral nutrition and to treat suspect thiamine deficiencies, often given routinely to hospitalized patients admitted with complications of chronic alcoholism. Oral forms of thiamine have not been associated with adverse events, ALT elevations or liver injury even when given in high doses. Parenteral administration of thiamine can be associated with immediate hypersensitivity reactions including anaphylaxis, but these are rare (<1:1000). Thus, neither oral nor parenteral high dose thiamine administration has been linked to serum enzyme elevations or to instances of clinically apparent liver injury.
Likelihood score: E (unlikely cause of liver injury).
Vitamin B2, Riboflavin
Riboflavin (rye' boe flay vin) is a water soluble B vitamin found in milk and dairy products, whole grains, legumes, lean meat and fish. Riboflavin is important in fat, carbohydrate and protein metabolism and is a central component in flavin adenine dinucleotide (FAD), a component of many enzymes that require electron transfer. Riboflavin deficiency is rare, but can occur with severe malnutrition and chronic alcoholism and usually presents with nonspecific symptoms including weakness, sore throat, mucositis, cheilosis, glossitis, dermatitis and anemia. Several foods are fortified with riboflavin including bread, cereals and milk. The recommended dietary allowance is 1.3 mg for adult men and 1.1 mg for women, which are well within the amounts found in a typical American diet. Riboflavin is available over-the-counter in multiple forms and is included in most multivitamin preparations in typical concentrations of 0.3 to 1.7 mg. Riboflavin is yellow in color, has natural fluorescence and is inactivated by light. Oral forms of riboflavin have not been associated with adverse events, ALT elevations or hepatotoxicity even when given in high doses. One reason why high doses of riboflavin are well tolerated is that oral doses above 30 mg are not absorbed, and what riboflavin is absorbed is rapidly excreted and body stores are generally limited.
Likelihood score: E (unlikely cause of clinically apparent liver injury).
Vitamin B3, Niacin
Niacin (nye' a sin) is a water-soluble B vitamin found in many foodstuffs, particularly fresh vegetables, milk, meat and eggs. Cereal grains and bread are often fortified with niacin. Chemically niacin is known as nicotinic acid and its amide as nicotinamide, both of which are precursors of two important co-enzymes, nicotinamide adenine dinucleotide (NAD) and its phosphate (NADP), which are important in oxidative and reductive reactions and in DNA repair. Niacin deficiency is the cause of pellagra which is now found largely among malnourished alcoholics, but was previously epidemic in populations dependent upon corn based diets. Symptoms of pellagra (“sour skin”) include dermatitis, diarrhea, depression, seizures and dementia. The recommended daily allowance of niacin for adults is 16 mg in men and 14 mg in women. Unlike other B vitamins, niacin has been linked to instances of clinically apparent liver injury, but only when given as niacin and in very high doses. Doses of niacin and nicotinamide used in multivitamins and as vitamin supplements (typically ~20 mg) and the higher doses used to treat pellagra (100-200 mg of nicotinamide three times daily) have not been linked to ALT elevations or to clinically apparent liver injury. Niacin (nicotinic acid) in high doses causes a decrease in serum cholesterol and is used to treat dyslipidemia, using concentrations in the range of 1.5 to 6.0 grams daily (100 to 400 times the RDA). Niacin at these dose levels and particularly the long acting formulations have been linked to a distinctive and severe form of liver injury typically presenting after several months of therapy with marked elevations in serum aminotransferase levels and with early features of hepatic failure. The latency to onset can be quite long (6 months to several years), but there is often a history of recent increase in dose or change in niacin formulation (to a sustained release form). Recovery upon withdrawal is rapid. Further discussion and examples of liver injury due to high dose niacin are provided in the section on niacin which can be reached using the link below.
Likelihood score: A[HD] (well known cause of clinically apparent liver injury, but only when given in high doses).
Vitamin B6, Pyridoxine
Pyridoxine (pir" i dox' een) is a water soluble B vitamin found in many foodstuffs, but in highest concentrations in meat, legumes and nuts. Pyridoxine actually represents a family of related compounds including pyridoxine, pyridoxal, pyridoxamine and their phosphates, which are the active coenzyme forms of vitamin B6. Pyridoxine acts as a cofactor in many enzyme systems, particularly in amino acid metabolism and heme synthesis. The recommended dietary allowance for pyridoxine is 1.3 to 2.0 mg for adults, a level that is well within that provided in typical American diets. Pyridoxine deficiency is rare, but can occur with severe malnutrition and chronic alcoholism. Symptoms of deficiency include weakness, fatigue, dermatitis, cheilosis and anemia. Certain medications including isoniazid, L-dopa, penicillamine and cycloserine interact with vitamin B6 and can cause deficiency. For that reason, these drugs are often given with pyridoxine supplementation (10 to 25 mg daily). Pyridoxine is available over-the-counter in multiple forms and concentrations and is included in virtually all multivitamin preparations, typically in concentrations of 2 to 3 mg. High doses of pyridoxine (50 to 500 mg daily) have been recommended to treat carpal tunnel syndrome, schizophrenia, autism and diabetes, but the efficacy in these conditions is not proven. Oral forms of pyridoxine (below 100 mg daily) have not been associated with adverse events, ALT elevations or hepatotoxicity. Prolonged use of high doses has been linked to sensory neuropathy and to occasional symptoms of nausea, gastrointestinal upset and dermatitis, but not to liver injury.
In contrast, pyridoxal-5’-phosphate which is used to treat genetic disorders of pyridoxal phosphate metabolism has been linked to serum enzyme elevations when given in high doses which can result in chronic hepatitis, cirrhosis and even hepatocellular carcinoma. These abnormalities of pyridoxine metabolism typically present in infancy with refractory seizures than respond to pyridoxine or pyridoxal phosphate. These abnormalities do not recur when patients are switched to pyridoxine (which is not always effective), but do recur when pyridoxal phosphate is restarted. Pyridoxal phosphate is not approved for use in the United States but can be obtained under special circumstances.
Likelihood score: E (unlikely cause of liver injury).
Vitamin B12, Cobalamin
Cyanocobalamin (sye" an oh koe bal' a min) is a water soluble B vitamin found in dairy products and meat. The cobalamins are complex organometallic compounds with a central cobalt atom within a porphyrin-like corrin ring. Cobalamins act as essential cofactors for several enzymes including methionine synthase and methylmalonyl-coenyzme A-mutase. The activities of these enzymes are important in RNA, protein and lipid metabolism and in hemoglobin synthesis. Cobalamin cannot be synthesized by humans and its presence in meat and eggs is due to its synthesis by microorganisms in the intestines of animals. Vitamin B12 absorption from the diet requires a cofactor (intrinsic factor) produced by parietal cells of the stomach. The major cause of cobalamin deficiency in humans is lack of intrinsic factor due to gastric atrophy caused by autoimmune destruction of parietal cells. Classic vitamin B12 deficiency causes profound anemia and symptoms of anorexia, irritability, apathy, weakness and a distinctive neurologic syndrome with paresthesias in the hands and feet, unsteady gait, moodiness, confusion and memory loss. The recommended daily dietary allowance of vitamin B12 is 2.4 µg in adults which is well within the concentrations found in the average American diet. Normal serum levels range from 200 to 900 pg/mL (150 to 660 picomoL). Vitamin B12 is available in multiple over-the-counter oral forms and it is included in most multivitamin preparations in typical concentrations of 1 to 6 µg. Parenteral formulations are available by prescription and treatment of vitamin B12 deficiency usually requires parenteral administration, typically in doses of 1000 µg intramuscularly once monthly. Neither oral nor parenteral forms of vitamin B12 have been linked to significant side effects or toxicity. The parenteral forms can cause local injection reactions and hypersensitivity and should be given intramuscularly or by deep subcutaneous injection and not intravenously. Vitamin B12 therapy has not been linked to ALT elevations or to clinically apparent acute liver injury.
Likelihood score: E (unlikely cause of liver injury).
Biotin
Biotin (bye' oh tin) is a water soluble vitamin (also known as vitamin B7, formerly vitamin H) and is found in liver, soy, beans and egg yolks. Egg whites, however, contain the protein avidin that binds to biotin and reduces its availability. Biotin acts as a carrier of carbon dioxide and plays a role in carboxylase enzymes involved in gluconeogenesis and fatty acid metabolism. The recommended daily dietary allowance for biotin has not been formally established, but the amounts needed are small and biotin is found in many foods and is produced by intestinal bacteria. An adequate intake for biotin has been estimated as 30 µg daily. Thus, most diets provide adequate amounts of biotin and its deficiency is rare. Biotin deficiency has occurred in humans on parenteral nutrition. Symptoms include hair loss, seborrheic dermatitis, depression, hallucinations and paresthesias. Biotin is available generically in many over-the-counter forms in doses of 5 to 10 mg and is included in most multivitamin preparations, usually in concentrations of 30 to 300 µg. Biotin is typically added to parenteral nutrition and the doses for deficiencies is in the range of 10 mg daily. Biotin supplements have no known adverse events and have not been linked to ALT elevations or hepatotoxicity.
Likelihood score: E (unlikely cause of liver injury).
Pantothenic Acid
Pantothenic acid (pan" toe then' ik as’ id) is a water soluble vitamin (also known as vitamin B5) that is found in many foods including vegetables, eggs, liver and yeast. Pantothenic acid is a component of coenzyme A and is involved in fatty acid and cholesterol metabolism and synthesis of steroid hormones. Pantothenic acid deficiency has been produced experimentally and causes gastrointestinal disturbance, muscle cramps, paresthesias, ataxia, depression and hypoglycemia. It may be the cause of burning feet syndrome, experienced by prisoners of war. Pantothenic acid deficiency occurs largely as a component of mixed, severe malnutrition with combined vitamin deficiencies. The recommended dietary allowance of pantothenic acid has not been formally established, but the dietary reference adequate intake is 5 mg daily in adults. Pantothenic acid is available generically in many over-the-counter forms and is included in most multivitamin preparations, typically in concentrations ranging from 1 to 10 mg. Pantothenic acid supplementation has not been associated with adverse events, ALT elevations or liver injury even when given in high doses.
Likelihood score: E (unlikely cause of liver injury).
Choline
Choline (koe' leen) is a precursor of acetylcholine, phospholipids and betaine and is necessary for the structural integrity of cell membranes and cholinergic neurotransmission. Choline is not considered a vitamin because it is synthesized in the mammalian liver. However, the amounts derived from de novo synthesis are not thought to be adequate for normal nutrition. Choline is widely distributed in many foodstuffs and particularly liver, milk, eggs and peanuts. The recommended adequate intake was been estimated to be 550 mg daily in men and 425 mg in women, levels which are regularly met by typical American diets. Choline deficiency can be created in experimental animals and causes fatty liver, which is often used as an experimental model for alcoholic and non-alcoholic fatty liver disease. Whether choline deficiency is an important cause of fatty liver disease in humans is not known, but severe protein-calorie malnutrition is often accompanied by marked fatty liver and choline supplementation of total parenteral nutrition decreases fat accumulation in the liver. High levels of choline intake (above 3.5 grams daily) can cause hypotension, diarrhea, salivation, sweating and a fishy body odor. However, there have been no reports of liver injury or ALT elevations associated with high oral supplement of choline.
Likelihood score: E (unlikely cause of clinically apparent liver injury).
Drug Class: Vitamins
Other Drugs in the Class: Vitamin A, Vitamin C, Vitamin D, Vitamin E, Vitamin K, Folate, Niacin
PRODUCT INFORMATION
REPRESENTATIVE TRADE NAMES
Vitamin B1, Thiamine – Generic, Combination Products
Vitamin B2, Riboflavin – Generic, Combination Products
Vitamin B6, Pyridoxine – Generic, Combination Products
Vitamin B12, Cyanocobalamin – Generic, Combination Products
DRUG CLASS
Vitamins
Product labeling at DailyMed, National Library of Medicine, NIH
CHEMICAL FORMULAS AND STRUCTURES
| DRUG | CAS REGISTRY NO | MOLECULAR FORMULA | STRUCTURE |
|---|---|---|---|
| Biotin | 58-85-5 | C10-H16-N2-O3-S |
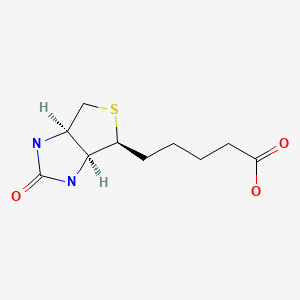
|
| Choline | 62-49-7 | C5-H14-N-O |
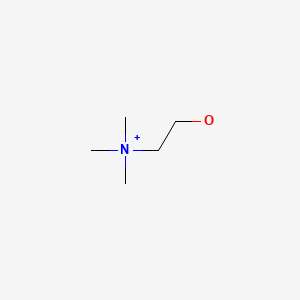
|
| Cyanocobalamin | 68-19-9 | C63-H88-Co-N14-O14-P |
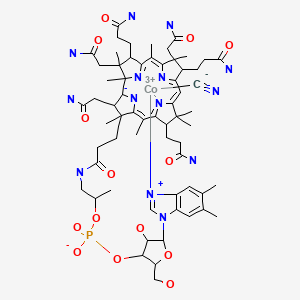
|
| Nicotinamide | 98-92-0 | C6-H6-N2-O |

|
| Pantothenic Acid | 79-83-4 | C9-H17-N-O5 |
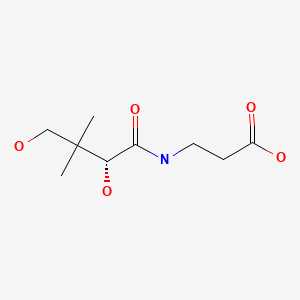
|
| Pyridoxine HCl | 58-56-0 | C8-H11-N-O3.Cl-H |
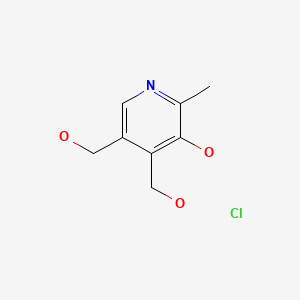
|
| Riboflavin | 83-88-5 | C17-H20-N4-O6 |

|
| Thiamine HCl | 67-03-8 | C12-H17-N4-O-S.Cl-H.Cl |
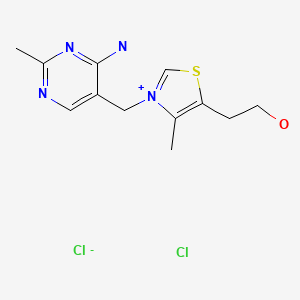
|
ANNOTATED BIBLIOGRAPHY
References updated: 27 May 2021
- Zimmerman HJ. Hepatotoxicity: the adverse effects of drugs and other chemicals on the liver. 2nd ed. Philadelphia: Lippincott, 1999.(Expert review of hepatotoxicity published in 1999, does not discuss vitamin B or water soluble vitamins other than niacin).
- Seeff L, Stickel F, Navarro VJ. Hepatotoxicity of herbals and dietary supplements. In, Kaplowitz N, DeLeve LD, eds. Drug-induced liver disease. 3rd ed. Amsterdam: Elsevier, 2013: pp, 631-57.(Review of hepatotoxicity of dietary supplements; does not discuss vitamins and minerals).
- Kaushansky K, Kipps TJ. Hematopoietic agents: growth factors, minerals and vitamins. In, Brunton LL, Hilal-Dandan R, Knollman BC, eds. Goodman & Gilman’s the pharmacological basis of therapeutics. 13th ed. New York: McGraw-Hill, 2018, pp. 751-68.(Textbook of pharmacology and therapeutics).
- Shils ME, Olson JA, Shike M, Ross AC. Modern nutrition in health and disease. 9th ed. Baltimore: Williams & Wilkins, 1998.(Textbook of nutrition with separate chapters on each of the B vitamins).
- Food and Nutrition Board, Institute of Medicine. DRI dietary reference intakes: for thiamin, riboflavin, niacin, vitamin B6, folate, vitamin B12, pantothenic acid, biotin and choline. Washington DC: National Academy Press, 1998. [PubMed: 23193625](Reports from the Food and Nutrition Board of the Institute of Medicine on reference values for vitamin intake, replacing the previously published Recommended Dietary Allowances).
- Office of Dietary Supplements. https://ods
.od.nih.gov /factsheets/list-all/ (Fact sheets on dietary supplements including B vitamins maintained and regularly updated by the Office of Dietary Supplements, National Institutes of Health). - Schaumburg H, Kaplan J, Windebank A, Vick N, Rasmus S, Pleasure D, Brown MJ. Sensory neuropathy from pyridoxine abuse. A new megavitamin syndrome. N Engl J Med. 1983;309:445–8. [PubMed: 6308447](27 year old woman developed difficulty walking and peripheral neuropathy 2 years after starting increasing doses of pyridoxine [to 5 g daily], resolving slowly and incompletely upon stopping; no mention of liver test results or hepatotoxicity).
- Stephen JM, Grant R, Yeh CS. Anaphylaxis from administration of intravenous thiamine. Am J Emerg Med. 1992;10:61–3. [PubMed: 1736919](32 year old man developed nausea, diffuse skin erythema, shortness of breath and wheezing within minutes of receiving intravenous thiamine [100 mg], responding to corticosteroids, epinephrine and antihistamines).
- Wrenn KD, Slovis CM. Is intravenous thiamine safe? Am J Emerg Med. 1992;10:165. [PubMed: 1586415](Letter in response to Stephen [1992] mentioning the safety of intravenous thiamine, the authors estimating that among 10,000 injections given for alcoholism and malnutrition, they had not seen any significant allergic reactions or other side effects).
- Johri S, Shetty S, Soni A, Kumar S. Anaphylaxis from intravenous thiamine--long forgotten? Am J Emerg Med. 2000;18:642–3. [PubMed: 10999594](51 year old woman with confusion and alcoholism developed shock requiring intubation after receiving intravenous thiamine [100 mg] with recurrence on reexposure two days later).
- Bendich A, Cohen M. Vitamin B6 safety issues. Ann N Y Acad Sci. 1990;585:321–30. [PubMed: 2192616](Review of the safety of pyridoxine in high doses including reports of neuropathy, which is typically reversible upon stopping and associated with use of more than 100 mg daily; no mention of ALT elevations or hepatotoxicity).
- Gdynia HJ, Müller T, Sperfeld AD, Kühnlein P, Otto M, Kassubek J, Ludolph AC. Severe sensorimotor neuropathy after intake of highest dosages of vitamin B6. Neuromuscul Disord. 2008;18:156–8. [PubMed: 18060778](75 year old man developed gait disturbance and sensory neuropathy two years after starting high doses of pyridoxine [9.6 g daily] along with 100 other supplements with marked, but not complete recovery upon stopping).
- Bender DA. Non-nutritional uses of vitamin B6. Br J Nutr. 1999;81:7–20. [PubMed: 10341670](Review of the non-nutritional uses and toxicity of pyridoxine mentions neuropathy, which arises usually with doses in excess of 200 mg daily; no mention of ALT elevations or hepatotoxicity).
- Reuben A, Koch DG, Lee WM., Acute Liver Failure Study Group. Drug-induced acute liver failure: results of a U.S. multicenter, prospective study. Hepatology. 2010;52:2065–76. [PMC free article: PMC3992250] [PubMed: 20949552](Among 1198 patients with acute liver failure enrolled in a US prospective study between 1998 and 2007, 133 were attributed to drug induced liver injury, but none were attributed to water soluble vitamins including niacin).
- Sriram K, Manzanares W, Joseph K. Thiamine in nutrition therapy. Nutr Clin Pract. 2012;27:41–50. [PubMed: 22223666](Review of thiamine in nutrition, history of its discovery and complications of its deficiency).
- Steinberg A, Gorman E, Tannenbaum J. Thiamine deficiency in stem cell transplant patients: a case series with an accompanying review of the literature. Clin Lymphoma Myeloma Leuk. 2014;14 Suppl:S111–3. [PubMed: 25486948](49 year old woman with acute leukemia underwent hematopoietic cell transplantation and developed diarrhea, weight loss, headaches and encephalopathy, responding to intravenous thiamine).
- Stroh C, Meyer F, Manger T. Beriberi, a severe complication after metabolic surgery - review of the literature. Obes Facts. 2014;7:246–52. [PMC free article: PMC5644786] [PubMed: 25095897](Review of 255 published cases of thiamine deficiency after bariatric surgery).
- Chalasani N, Bonkovsky HL, Fontana R, Lee W, Stolz A, Talwalkar J, Reddy KR, et al. United States Drug Induced Liver Injury Network. Features and outcomes of 899 patients with drug-induced liver injury: The DILIN Prospective Study. Gastroenterology. 2015;148:1340–52. [PMC free article: PMC4446235] [PubMed: 25754159](Among 899 cases of drug induced liver injury enrolled in a US prospective study between 2004 and 2013, 7 were attributed to niacin, but none were attributed to any other vitamin).
- Isenberg-Grzeda E, Alici Y, Hatzoglou V, Nelson C, Breitbart W. Nonalcoholic thiamine-related encephalopathy (Wernicke-Korsakoff Syndrome) among inpatients with cancer: a series of 18 cases. Psychosomatics. 2016;57:71–81. [PMC free article: PMC4979979] [PubMed: 26791514](Over an 18 month period, 18 hospitalized patients receiving cancer chemotherapy were diagnosed with Wernicke-Korsakoff Syndrome, many with nausea, vomiting, weakness and lactic acidosis).
- Yoshida I, Sakaguchi Y, Nakano M, Yamashita F, Hitoshi T. Pyridoxal phosphate-induced liver injury in a patient with homocystinuria. J Inherit Metab Dis. 1985;8:91. [PubMed: 3939539](7 year old boy with homocystinuria developed malaise and liver test abnormalities 2 months after starting high doses [500 to 1000 mg daily] of pyridoxal phosphate [ALT 228 Karmen units, Alk P 57.9 KA units, bilirubin not provided], which returned to normal within a month of stopping and did not recur with pyridoxine but did with restarting pyridoxal phosphate).
- Sudarsanam A, Singh H, Wilcken B, Stormon M, Arbuckle S, Schmitt B, Clayton P, et al. Cirrhosis associated with pyridoxal 5'-phosphate treatment of pyridoxamine 5'-phosphate oxidase deficiency. JIMD Rep. 2014;17:67–70. [PMC free article: PMC4241198] [PubMed: 25256445](8 year old boy with pyridoxamine 5’ phosphate oxidase deficiency required high doses of pyridoxamine 5’ phosphate to control seizures [~100 mg/kg/day] and was found to have abnormal liver tests [ALT 169 U/L, GGT 131 U/L, prothrombin time 19 seconds, bilirubin not given] and cirrhosis on liver biopsy, liver tests improving with lowering of the dose).
- Mills PB, Camuzeaux SS, Footitt EJ, Mills KA, Gissen P, Fisher L, Das KB, et al. Epilepsy due to PNPO mutations: genotype, environment and treatment affect presentation and outcome. Brain. 2014;137(Pt 5):1350–60. [PMC free article: PMC3999720] [PubMed: 24645144](Description of 15 children with pyridoxine-5’-phosphate oxidase deficiency, two of whom developed liver function abnormalities when treated with pyridoxal-5-phosphate which improved but did not resolve when the dose was reduced; details not provided).
- Wilson MP, Plecko B, Mills PB, Clayton PT. Disorders affecting vitamin B6 metabolism. J Inherit Metab Dis. 2019;42:629–46. [PubMed: 30671974](Review of genetic disorders associated with impairment of pyridoxal-5-phosphate metabolism which typically presents in childhood with severe seizures and is responsive to therapy with pyridoxal-5-phosphate, which at high doses has been linked to serum aminotransferase elevations that can lead to cirrhosis and hepatocellular carcinoma).
- Sinha S, Kataria A, Kolla BP, Thusius N, Loukianova LL. Wernicke encephalopathy-clinical pearls. Mayo Clin Proc. 2019;94:1065–72. [PubMed: 31171116](Clinical review of the clinical features of Wernicke encephalopathy which is associated with alcoholism but also cancer chemotherapy, malabsorption syndromes, intestinal obstruction, hyperemesis gravidarum, and gastric bypass surgery, and is treated with high doses of thiamine given parenterally which is safe even in doses of 600 mg daily).
- Calderon-Ospina CA, Nava-Mesa MO, Paez-Hurtado AM. Update on safety profiles of vitamins B1, B6, and B12: a narrative review. Ther Clin Risk Manag. 2020;16:1275–88. [PMC free article: PMC7764703] [PubMed: 33376337](Review of the potential adverse reactions to use of high doses of thiamine [largely just rare mild-to-moderate infusion or hypersensitivity reactions], pyridoxine [neurotoxicity associated with prolonged use of high doses, usually reversible] and vitamin B12 [hip fractures and lung cancer, but relatedness is probably confounded by other factors including smoking]).
- Cree BAC, Cutter G, Wolinsky JS, Freedman MS, Comi G, Giovannoni G, Hartung HP, et al. SPI2 investigative teams. Safety and efficacy of MD1003 (high-dose biotin) in patients with progressive multiple sclerosis (SPI2): a randomised, double-blind, placebo-controlled, phase 3 trial. Lancet Neurol. 2020;19:988–97. [PubMed: 33222767](Among 642 patients with progressive multiple sclerosis treated with oral biotin [100 mg] or placebo three times daily for 12 months, improvements in disability and walk time were similar in the two groups as were overall [84% vs 85%] and serious adverse event rates [26% vs 26%], and “serum chemistries… did not differ between groups”, but biotin did interfere with results of assays using biotinylated antibodies).
- McLaughlin K, Joyal K, Lee S, Corrado M, Marquis K, Anger K, Szumita P. Safety of intravenous push thiamine administration at a tertiary academic medical center. J Am Pharm Assoc. 2020;60(4):598–601. [PubMed: 31932197](Among 8606 administrations of intravenous thiamine [100 to 500 mg] in 2595 patients given over a 2 year period, there were no instances of anaphylaxis and only rare [n=26] mild local infusion reactions).
- da Silva JSV, Seres DS, Sabino K, Adams SC, Berdahl GJ, Citty SW, Cober MP, et al. Parenteral Nutrition Safety and Clinical Practice Committees, American Society for Parenteral and Enteral Nutrition. ASPEN consensus recommendations for refeeding syndrome. Nutr Clin Pract. 2020;35:178–95. [PubMed: 32115791](Description of clinical features and pathogenesis of refeeding syndrome and appropriate approach to its prevention, focusing upon use and monitoring of serum phosphate, potassium and magnesium and including use of thiamine; no mention of liver injury or hepatitis).
- Coughlin CR 2nd, Tseng LA, Abdenur JE, Ashmore C, Boemer F, Bok LA, Boyer M, et al. Consensus guidelines for the diagnosis and management of pyridoxine-dependent epilepsy due to α-aminoadipic semialdehyde dehydrogenase deficiency. J Inherit Metab Dis. 2021;44:178–92. [PubMed: 33200442](Guidelines for management of children with pyridoxine-responsible epilepsy with ALDH7A1 deficiency recommends treatment with pharmacologic doses of pyridoxine [30 mg/kg/day] and possibly a lysine restricted diet, with monitoring for peripheral neuropathy; no mention of hepatotoxicity).
- PMCPubMed Central citations
- PubChem SubstanceRelated PubChem Substances
- PubMedLinks to PubMed
- Review Hydrosoluble vitamins.[Handb Clin Neurol. 2014]Review Hydrosoluble vitamins.Chawla J, Kvarnberg D. Handb Clin Neurol. 2014; 120:891-914.
- Water-soluble vitamins in cancer patients on parenteral nutrition: a prospective study.[JPEN J Parenter Enteral Nutr. ...]Water-soluble vitamins in cancer patients on parenteral nutrition: a prospective study.Inculet RI, Norton JA, Nichoalds GE, Maher MM, White DE, Brennan MF. JPEN J Parenter Enteral Nutr. 1987 May-Jun; 11(3):243-9.
- Water soluble vitamins in normal human skin.[J Invest Dermatol. 1953]Water soluble vitamins in normal human skin.LEE TH, LERNER AB, HALBERG RJ. J Invest Dermatol. 1953 Jan; 20(1):19-26.
- NUTRITIONAL STUDIES INVOLVING VITAMIN B6 OF LACTIC ACID BACTERIA. I. THE EFFECTS OF VITAMIN B6 AND ALANINE ON THE GROWTH OF LACTIC ACID BACTERIA IN ALANINE-FREE SYNTHETIC MEDIA CONTAINING ESSENTIAL VITAMINS.[J Vitaminol (Kyoto). 1964]NUTRITIONAL STUDIES INVOLVING VITAMIN B6 OF LACTIC ACID BACTERIA. I. THE EFFECTS OF VITAMIN B6 AND ALANINE ON THE GROWTH OF LACTIC ACID BACTERIA IN ALANINE-FREE SYNTHETIC MEDIA CONTAINING ESSENTIAL VITAMINS.KAKIUCHI Y. J Vitaminol (Kyoto). 1964 Dec 10; 10:264-74.
- Review B-vitamins and HIV/AIDS.[Nutrition and HIV: Epidemiolog...]Review B-vitamins and HIV/AIDS.Layden AJ, Finkelstein JL. Nutrition and HIV: Epidemiological Evidence to Public Health. 2018 May 15
- Vitamin B - LiverToxVitamin B - LiverTox
Your browsing activity is empty.
Activity recording is turned off.
See more...