Clinical Description
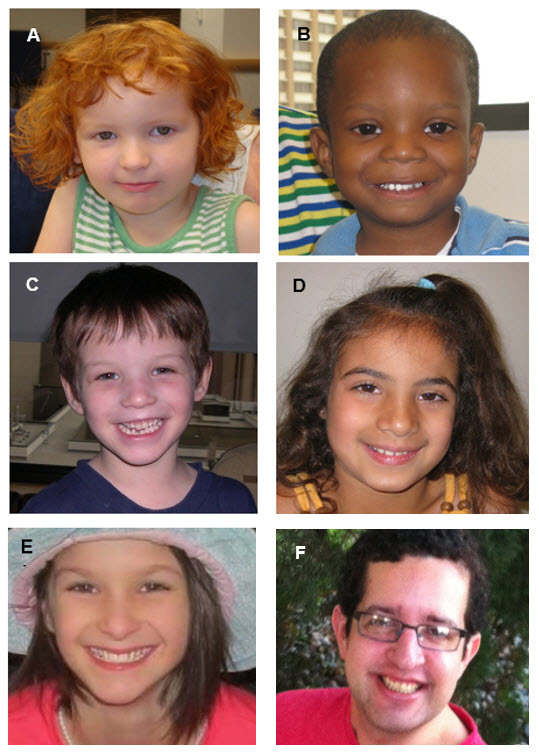
Potocki-Lupski syndrome (PTLS) is characterized by developmental delay, intellectual disability, behavioral disturbances, organ system involvement, and mildly dysmorphic facial features [Potocki et al 2007, Treadwell-Deering et al 2010]. See .
PTLS can manifest in infancy with hypotonia, oropharyngeal dysphagia leading to failure to thrive, congenital heart disease, and hypoglycemia associated with growth hormone deficiency. In contrast, individuals who are more mildly affected may manifest cognitive and behavioral abnormalities only, and not be diagnosed until later in childhood [Potocki et al 2007, Treadwell-Deering et al 2010, Neira-Fresneda & Potocki 2015].
Neurodevelopmental
Mild-to-moderate infantile hypotonia with oropharyngeal dysphagia is common and contributes to poor feeding and mild-to-moderate gross motor delays [Potocki et al 2007, Soler-Alfonso et al 2011]. Poor feeding or poor weight gain can be an initial presentation. Infants and children have significantly lower weight for age, weight for length, and BMI for age than the reference population [Soler-Alfonso et al 2011].
Although gross motor delay is observed in the vast majority, most will achieve independent walking by age two years. Rarely, independent ambulation can be delayed until age four years.
Cognitive impairment is one of the most common characteristics of PTLS [Potocki et al 2007]. The vast majority of individuals tested have moderate intellectual disability [Treadwell-Deering et al 2010].
Speech delay is universal. Standardized testing has revealed expressive and receptive language impairment which can include articulation difficulties and disordered intonation and prosody [Treadwell-Deering et al 2010]. Some individuals may exhibit verbal apraxia.
While there are no formal studies of articulation and language abilities in teens and adults with PTLS, verbal abilities appear to improve both with age and speech therapy. Little data regarding findings in adults are available; however, adults with a confirmed molecular genetic diagnosis who have been clinically evaluated have cognitive challenges.
Sleep-disordered breathing. Although sleep disturbances are not often clinically recognized and significant airway obstruction is not found on examination, abnormalities frequently evident on sleep studies include sleep-disordered breathing such as mild central and/or obstructive sleep apnea [Potocki et al 2007, Neira-Fresneda & Potocki 2015]. Children with sleep apnea may present with snoring or hyperactivity. In addition, periodic limb movement disorder is commonly observed.
Behavioral difficulties identified by objective measures and by parental reports include attention problems, withdrawal, and high levels of hyperactivity and anxiety. Reported deficits in executive functioning include initiating and shifting activities and working memory.
Autism spectrum disorder (ASD) and/or autistic features (decreased eye contact, motor mannerisms or posturing, sensory hypersensitivity or preoccupation, repetitive behaviors, difficulty with transitions, lack of appropriate functional or symbolic play, and lack of joint attention) are seen in affected individuals [Potocki et al 2007, Treadwell-Deering et al 2010, Neira-Fresneda & Potocki 2015]. Using validated scoring systems (ADI-R and ADOS-G), Treadwell-Deering et al [2010] found that approximately 60% of a small cohort of children with PTLS met criteria for ASD.
Growth Hormone Deficiency
Five of seven individuals in the original description of PTLS had short stature; one of the five had documented growth hormone deficiency [Potocki et al 2000]. In a second study, one of ten individuals had short stature (but not growth hormone deficiency) [Potocki et al 2007]. Subsequently, additional individuals with PTLS and growth hormone deficiency have been identified, including some with hypoglycemia in infancy and short stature in early childhood [Author, personal observation].
Other
Musculoskeletal features of PTLS that can mimic those seen in connective tissue disorders include severe bilateral clubfeet [Dhanaraj et al 2015], joint hypermobility, kyphoscoliosis, pes planus, and long fingers and toes [Martin et al 2008].
Renal anomalies include hypoplastic, multicystic dysplastic kidneys, and hydronephrosis [Goh et al 2012].
EEG abnormalities observed during sleep include slow occipital dominant rhythm and generalized and/or focal epileptiform abnormalities. Clinical or electroencephalographic seizures have not been reported [Potocki et al 2007, Neira-Fresneda & Potocki 2015].
Other findings include the following [Potocki et al 2007, Neira-Fresneda & Potocki 2015]:
Hyperopia (common, but not significant enough to require corrective lenses in childhood)
Mild high-frequency sensorineural hearing loss
Dental malocclusion and dental crowding