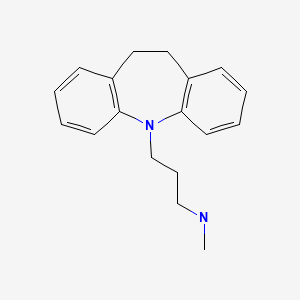
CASRN: 50-47-5
Drug Levels and Effects
Summary of Use during Lactation
Milk levels of desipramine and its metabolite are low and have not been detected in the serum of breastfed infants. Immediate side effects have not been reported and a limited amount of follow-up has found no adverse effects on infant growth and development. Desipramine use during breastfeeding would usually not be expected to cause any adverse effects in breastfed infants, especially if the infant is older than 2 months. A safety scoring system finds desipramine use to be possible during breastfeeding.[1]
Drug Levels
Desipramine is metabolized to 2-hydroxydesipramine which has antidepressant activity equal to that of desipramine.[2]
Maternal Levels. A mother who was taking desipramine 300 mg daily had average milk desipramine plus 2-hydroxydesipramine milk levels of 338 mcg/L at 9 hours after the dose 10 to 11 weeks postpartum.[3]
Infant Levels. Two infants whose mothers were taking desipramine during pregnancy and lactation with a maternal dosage of 200 mg daily. One infant was tested at 2.3 and 14.9 weeks of age while breastfeeding 7 to 9 times daily and the other was tested at 5.4 weeks of age while breastfeeding 10 to 12 weeks of age. Neither had detectable (<25 mcg/L) serum desipramine.[4]
Two other infants had mothers who began desipramine postpartum. One infant whose mother took desipramine 150 mg daily was tested at 12.3 weeks of age while breastfeeding 4 to 6 times daily. The other whose mother took desipramine 37 mg daily was tested at 33 weeks of age while breastfeeding 0 to 3 times daily. Both had undetectable (<10 mcg/L) serum desipramine levels.[4]
Effects in Breastfed Infants
One infant whose mother took desipramine 100 mg daily for 8 weeks starting at 16 weeks postpartum was followed up at 36 months of age. No adverse effects on growth and development were found.[5]
Effects on Lactation and Breastmilk
Desipramine has caused increased serum prolactin levels in some patients.[6] The clinical relevance of these findings in nursing mothers is not known. The prolactin level in a mother with established lactation may not affect her ability to breastfeed.
An observational study looked at outcomes of 2859 women who took an antidepressant during the 2 years prior to pregnancy. Compared to women who did not take an antidepressant during pregnancy, mothers who took an antidepressant during all 3 trimesters of pregnancy were 37% less likely to be breastfeeding upon hospital discharge. Mothers who took an antidepressant only during the third trimester were 75% less likely to be breastfeeding at discharge. Those who took an antidepressant only during the first and second trimesters did not have a reduced likelihood of breastfeeding at discharge.[7] The antidepressants used by the mothers were not specified.
A retrospective cohort study of hospital electronic medical records from 2001 to 2008 compared women who had been dispensed an antidepressant during late gestation (n = 575) to those who had a psychiatric illness but did not receive an antidepressant (n = 1552) and mothers who did not have a psychiatric diagnosis (n = 30,535). Women who received an antidepressant were 37% less likely to be breastfeeding at discharge than women without a psychiatric diagnosis, but no less likely to be breastfeeding than untreated mothers with a psychiatric diagnosis.[8] None of the mothers were taking desipramine.
In a study of 80,882 Norwegian mother-infant pairs from 1999 to 2008, new postpartum antidepressant use was reported by 392 women and 201 reported that they continued antidepressants from pregnancy. Compared with the unexposed comparison group, late pregnancy antidepressant use was associated with a 7% reduced likelihood of breastfeeding initiation, but with no effect on breastfeeding duration or exclusivity. Compared with the unexposed comparison group, new or restarted antidepressant use was associated with a 63% reduced likelihood of predominant, and a 51% reduced likelihood of any breastfeeding at 6 months, as well as a 2.6-fold increased risk of abrupt breastfeeding discontinuation. Specific antidepressants were not mentioned.[9]
Alternate Drugs to Consider
References
- 1.
- Uguz F. A new safety scoring system for the use of psychotropic drugs during lactation. Am J Ther. 2021;28:e118–e126. [PubMed: 30601177]
- 2.
- Weissman AM, Levy BT, Hartz AJ, et al. Pooled analysis of antidepressant levels in lactating mothers, breast milk, and nursing infants. Am J Psychiatry. 2004;161:1066–78. [PubMed: 15169695]
- 3.
- Stancer HC, Reed KL. Desipramine and 2-hydroxydesipramine in human breast milk and the nursing infant's serum. Am J Psychiatry. 1986;143:1597–1600. [PubMed: 3789215]
- 4.
- Birnbaum CS, Cohen LS, Bailey JW, et al. Serum concentrations of antidepressants and benzodiazepines in nursing infants: A case series. Pediatrics. 1999;104:e11. [PubMed: 10390297]
- 5.
- Misri S, Sivertz K. Tricyclic drugs in pregnancy and lactation: A preliminary report. Int J Psychiatry Med. 1991;21:157–71. [PubMed: 1894455]
- 6.
- Madhusoodanan S, Parida S, Jimenez C. Hyperprolactinemia associated with psychotropics--a review. Hum Psychopharmacol. 2010;25:281–97. [PubMed: 20521318]
- 7.
- Venkatesh KK, Castro VM, Perlis RH, et al. Impact of antidepressant treatment during pregnancy on obstetric outcomes among women previously treated for depression: An observational cohort study. J Perinatol. 2017;37:1003–9. [PMC free article: PMC10034861] [PubMed: 28682318]
- 8.
- Leggett C, Costi L, Morrison JL, et al. Antidepressant use in late gestation and breastfeeding rates at discharge from hospital. J Hum Lact. 2017;33:701–9. [PubMed: 28984528]
- 9.
- Grzeskowiak LE, Saha MR, Nordeng H, et al. Perinatal antidepressant use and breastfeeding outcomes: Findings from the Norwegian Mother, Father and Child Cohort Study. Acta Obstet Gynecol Scand. 2022;101:344–54. [PMC free article: PMC9564556] [PubMed: 35170756]
Substance Identification
Substance Name
Desipramine
CAS Registry Number
50-47-5
Drug Class
Breast Feeding
Lactation
Milk, Human
Antidepressive Agents
Antidepressive Agents, Tricyclic
Disclaimer: Information presented in this database is not meant as a substitute for professional judgment. You should consult your healthcare provider for breastfeeding advice related to your particular situation. The U.S. government does not warrant or assume any liability or responsibility for the accuracy or completeness of the information on this Site.
Publication Details
Publication History
Last Revision: April 18, 2022.
Copyright
Attribution Statement: LactMed is a registered trademark of the U.S. Department of Health and Human Services.
Publisher
National Institute of Child Health and Human Development, Bethesda (MD)
NLM Citation
Drugs and Lactation Database (LactMed®) [Internet]. Bethesda (MD): National Institute of Child Health and Human Development; 2006-. Desipramine. [Updated 2022 Apr 18].