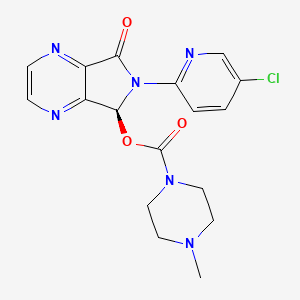
CASRN: 138729-47-2
Drug Levels and Effects
Summary of Use during Lactation
No data are available on the use of eszopiclone during breastfeeding. Data from the racemate, zopiclone, indicate that occasional use while breastfeeding an older infant should pose little risk to the infant. A safety scoring system finds zopiclone possible to use during breastfeeding,[1] but the infant should be monitored for sedation, poor feeding and poor weight gain.[2] An alternate hypnotic may be preferred, especially while nursing a newborn or preterm infant.
Drug Levels
Eszopiclone is the S-isomer of zopiclone which is a racemic mixture containing 50% S- and 50% R-eszopiclone. In the United States, the recommended dose of eszopiclone is 2 mg compared with the dose of 7.5 mg of zopiclone used in Europe.
Maternal Levels. Three nursing women (time postpartum not stated) received a single oral dose of zopiclone 7.5 mg. Peak milk levels of about 55 mcg/L occurred about 2 hours after the dose. The half-life in milk was similar to that in plasma which was 5.3 hours in healthy adults.[3,4]
Twelve nursing mothers who were 2 to 6 days postpartum were given a single oral dose of 7.5 mg of zopiclone. The peak milk level averaged 34 mcg/L (range 24 to 57 mcg/L) and it occurred 2.4 hours (range 1 to 6 hours) after the dose. The mean half-life in milk was 5.3 hours (range 3.5 to 8.6 hours). The authors estimated that an exclusively breastfed infant would receive an average of 15 mcg/kg or 1.2 to 1.4% of the maternal weight-adjusted dosage of zopiclone.[2]
A woman took zopiclone 3.75 mg 4 times daily during pregnancy and postpartum for tension headaches. At 2 weeks postpartum, 2 hours after the second dose of the day, milk zopiclone levels ranged from 2.4 to 47.3 mcg/L and daily zopiclone excretion in the milk was estimated to be 3 mcg for a production of 335 mL. The weight-adjusted maternal dosage was estimated to be 3.2%.[5]
Infant Levels. Relevant published information was not found as of the revision date.
Effects in Breastfed Infants
In 12 mothers who were 2 to 6 days postpartum and took 7.5 mg of zopiclone, infant breastfeeding was interrupted for 8 to 10 hours before resuming. No unusual effect were noted in the infants.[2]
Thirty-week preterm twins were born to a mother who took zopiclone 3.75 mg 4 times daily for tension headache during pregnancy. They developed withdrawal symptoms during the first week of life. Beginning at 2 weeks of age, they were about two-thirds breastfed by their mother who continued the drug at the same dose. The infants had no clinical abnormalities and were discharged from the hospital 6 weeks after birth.[5]
Effects on Lactation and Breastmilk
Relevant published information was not found as of the revision date.
References
- 1.
- Uguz F. A new safety scoring system for the use of psychotropic drugs during lactation. Am J Ther 2021;28:e118-e26. [PubMed: 30601177]
- 2.
- Matheson I, Sande HA, Gaillot J. The excretion of zopiclone into breast milk. Br J Clin Pharmacol 1990;30:267-71. [PMC free article: PMC1368227] [PubMed: 2206788]
- 3.
- Gaillot J, Heusse D, Hougton GW, et al. Pharmacokinetics and metabolism of zopiclone. Int Pharmacopsychiatry 1982;17 (Suppl 2):76-91. [PubMed: 7188377]
- 4.
- Gaillot J, Heusse D, Hougton GW, et al. Pharmacokinetics and metabolism of zopiclone. Pharmacology 1983;27 (Suppl 2):76-91. [PubMed: 6669634]
- 5.
- Mathieu O, Masson F, Thompson MA, et al. Case report: In utero exposure and safe breastfeeding in two premature twins of a chronically treated mother with high doses of zopiclone. Fundam Clin Pharmacol 2010;24 (Suppl. S1):424. doi:10.1111/j.1472-8206.2010.00819.x [CrossRef]
Substance Identification
Substance Name
Eszopiclone
CAS Registry Number
138729-47-2
Drug Class
Breast Feeding
Lactation
Milk, Human
Hypnotics and Sedatives
Disclaimer: Information presented in this database is not meant as a substitute for professional judgment. You should consult your healthcare provider for breastfeeding advice related to your particular situation. The U.S. government does not warrant or assume any liability or responsibility for the accuracy or completeness of the information on this Site.
Publication Details
Publication History
Last Revision: October 15, 2024.
Copyright
Attribution Statement: LactMed is a registered trademark of the U.S. Department of Health and Human Services.
Publisher
National Institute of Child Health and Human Development, Bethesda (MD)
NLM Citation
Drugs and Lactation Database (LactMed®) [Internet]. Bethesda (MD): National Institute of Child Health and Human Development; 2006-. Eszopiclone. [Updated 2024 Oct 15].