CASRN: 599-79-1
Drug Levels and Effects
Summary of Use during Lactation
Sulfasalazine and its active metabolite mesalamine are poorly excreted into breastmilk. However, rather high levels of the mesalamine metabolite N-acetyl-5-ASA appear in breastmilk and its effects on breastfed infants are unknown. Another sulfasalazine metabolite, sulfapyridine, also appears in milk and infant serum and might cause hemolysis, especially in newborn infants and in those with glucose-6-phosphate dehydrogenase (G6PD) deficiency. The time of greatest risk for hemolysis in fullterm newborns without G6PD deficiency might be as short as 8 days after birth.[1] Bloody diarrhea has occurred in an infant whose mother was taking sulfasalazine and a few cases of diarrhea have been reported in infants exposed to mesalamine in breastmilk, although the rate is not high. Most experts and professional guidelines consider mesalamine derivatives to be safe during breastfeeding.[2-9] If the mother requires sulfasalazine, it is not a reason to discontinue breastfeeding, but carefully observe breastfed infants for diarrhea. Other mesalamine derivatives that do not contain a sulfonamide are preferred.
Drug Levels
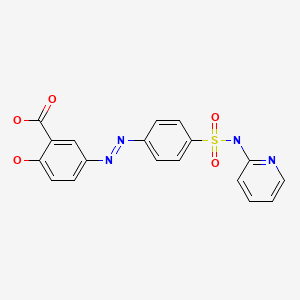
Sulfasalazine is a chemical combination of sulfapyridine and mesalamine (5-aminosalicylic acid; 5-ASA) which is considered to be the active component. Sulfapyridine is metabolized to acetylated and glucuronidated metabolites. Mesalamine is metabolized to N-acetyl-5-ASA, which is inactive in treating inflammatory bowel disease, but its possible effects on the breastfed infant are unknown.
Maternal Levels. Three women who were taking 500 mg of sulfasalazine 4 times daily had breastmilk samples analyzed 1 week postpartum. The times of the samples in relation to the doses were not stated. Sulfasalazine milk levels averaged 2.7 mg/L, total sulfapyridine (including all metabolites) averaged 10.3 mg/L and free sulfapyridine (not including metabolites) was 6.5 mg/L. Mesalamine and its metabolites were not measured.[10]
Twelve patients with inflammatory bowel disease were started on sulfasalazine 3 weeks postpartum and had breastmilk levels taken 2 to 3 weeks later. Of 31 samples in the 12 women, only 5 samples had detectable (>1 mg/L) sulfasalazine levels, ranging from 1.5 to 2.5 mg/L with dosages of 1 or 2 grams of sulfasalazine daily. Eight of the patients had 16 untimed milk levels measured while taking dosages of 1 to 3 grams daily. Milk sulfapyridine levels ranged from 1 to 38 mg/L, with some correlation to dosage. Almost no sulfapyridine metabolites were found in milk.[11]
A woman began taking sulfasalazine 500 mg 4 times daily at 4.5 months postpartum for ulcerative colitis. She provided milk samples on 8 days over the next 2 months. A total of 44 samples were obtained, including 10 on the first day of medication. Other samples were obtained midway between nursing bouts which occurred about every 4 hours. Sulfasalazine was not found in any of the milk samples. Sulfapyridine appeared in milk 4 hours after the first dose in a concentration of 4.8 mg/L. Over the next 2 weeks, sulfapyridine levels fluctuated in the range of 3.9 to 6.6 mg/L and acetylsulfapyridine levels were in the range of 0.4 to 2 mg/L. Total sulfapyridine plus metabolites were in the range of 3.2 to 13 mg/L with most values between 5 and 8 mg/L. Mesalamine was not detected in breastmilk.[12]
Three women who were taking sulfasalazine 3 grams daily for ulcerative colitis each had a single milk level measured 3 to 4 days postpartum. Sampling time in relation to the dose was not reported. Sulfasalazine levels ranged from <0.5 mg/L to 1.2 mg/L; sulfapyridine levels ranged from 9 to 16.9 mg/L; acetylsulfapyridine levels ranged from 1.1 to 6.7 mg/L. Mesalamine levels were uniformly 0.02 mg/L and N-acetyl-5ASA levels ranged from 1.2 to 3.4 mg/L.[13]
Eight women were taking sulfasalazine during pregnancy and postpartum in an average dosage of 2.6 grams daily. Milk samples were taken 2 hours after breastfeeding, but times in relation to a dose were not stated. Sulfasalazine was undetectable (<0.5 to 1 mg/L) in all but one milk sample in which it was 4.1 mg/L. Sulfapyridine levels in 7 of the samples ranged from 12 to 60 mg/L.[14]
Infant Levels. The breastfed infant of a mother taking sulfasalazine 500 mg 4 times daily had levels of sulfapyridine plus metabolites measured in urine 3 times during 2.5 months of therapy, beginning at 4.5 months postpartum. Total sulfapyridine plus metabolites ranged from 3 to 4.1 mg/L, with most of the drug appearing as metabolites. No mesalamine was detected in the infant's urine.[12]
A 3-month-old breastfed infant whose mother was taking sulfasalazine 3 grams daily had a sulfapyridine blood level of 5.3 mg/L. The infant's mother was a slow acetylator, but the infant's acetylator status was not determined.[15]
Eight breastfed infants whose mothers were taking sulfasalazine in an average dosage of 2.6 grams daily had serum levels measured once between 2 and 24 weeks of age. Sulfasalazine serum levels were undetectable (<0.5 to 1 mg/L) in 6 infants. In the other 2 infants, sulfasalazine serum levels were 1 and 1.7 mg/L. Sulfapyridine was detectable in 5 infants' serum in levels ranging from 1 to 4.8 mg/L.[14]
Effects in Breastfed Infants
One group of investigators stated that they had 10 years of experience using sulfasalazine during the puerperium with no obvious adverse effects in breastfed infants.[10]
The breastfed infant of a mother taking sulfasalazine 500 mg 4 times daily beginning at 4.5 months postpartum experienced no adverse effects during 2.5 months of nursing.[12]
A 2-month-old breastfed infant whose mother was taking sulfasalazine 3 grams daily had an episode of bloody diarrhea. The bloody diarrhea recurred 2 weeks later and persisted until 3 months of age. The infant had up to 6 bowel movements daily and the stools had a loose consistency and were mixed with fresh blood. A colonoscopy revealed a mild inflammatory process and numerous punctate erosions in the mucosa. The infant had a sulfapyridine blood level of 5.3 mg/L, which may have been enhanced because the infant's mother was a slow acetylator. The bloody diarrhea stopped 48 to 72 hours after the mother stopped taking sulfasalazine. A repeat colonoscopy at 4.5 months of age was normal and no further bloody diarrhea occurred up to 14 months of follow-up. The authors felt that the reaction was likely caused by an allergic reaction to sulfapyridine.[15] The reaction was probably caused by sulfasalazine or one of its metabolites in breastmilk. Both sulfapyridine and mesalamine have been reported to cause diarrhea in breastfed infants.[16,17]
Eight infants whose mothers were taking sulfasalazine in average dosage of 2.6 grams daily were breastfed. Sulfapyridine was detectable in 5 infant's serum in levels ranging from 1 to 4.8 mg/L. The authors pointed out that these levels were far below those required to displace bilirubin from serum albumin binding sites.[14]
A case-control study compared the infants of mothers taking mesalamine (n = 117; average dose, 2065 mg daily), olsalazine (n = 2) or sulfasalazine (n = 2) to infants of matched control mothers (n = 121) who were exposed to no treatment known to be harmful to a breastfed infant. Infants were exposed to mesalamine through milk for a mean of 5.3 months (range: 3 days-24 months). Infants were breastfed for an average of about 7.4 months and were followed up at an average age of about 22 months. No difference in the frequency or characteristics of maternally reported adverse events were found between exposed and control infants.[18,19]
A woman with Crohn's disease used sulfasalazine 4 grams daily during pregnancy and postpartum. During breastfeeding (extent not stated) she also received infliximab 5 mg/kg every 8 weeks and prednisone 60 mg daily in a tapering schedule. At 6 months of age, the infant was asymptomatic with regular weight gain.[20]
In a cohort study, over a 10-year period 15 nursing mothers with rheumatoid arthritis took sulfasalazine during partial or exclusive breastfeeding. No mention was made of adverse effects in their infants.[21]
Effects on Lactation and Breastmilk
Relevant published information was not found as of the revision date.
Alternate Drugs to Consider
(Rheumatoid Arthritis) Auranofin, Etanercept, Gold Sodium Thiomalate, Hydroxychloroquine, Infliximab, Methotrexate, Penicillamine, Sulfasalazine; (Inflammatory Bowel Disease) Adalimumab, Azathioprine, Budesonide, Certolizumab Pegol, Infliximab, Mesalamine, Prednisone, Sulfasalazine
References
- 1.
- Zao J, Koren G, Bozzo P. Using nitrofurantoin while breastfeeding a newborn. Can Fam Physician 2014;60:539-40. [PMC free article: PMC4055319] [PubMed: 24925943]
- 2.
- Mahadevan U, Matro R. Care of the pregnant patient with inflammatory bowel disease. Obstet Gynecol 2015;126:401-12. [PubMed: 26241432]
- 3.
- van der Woude CJ, Kolacek S, Dotan I, et al. European evidenced-based consensus on reproduction in inflammatory bowel disease. J Crohns Colitis 2010;4:493-510. [PubMed: 21122553]
- 4.
- Flint J, Panchal S, Hurrell A, et al. BSR and BHPR guideline on prescribing drugs in pregnancy and breastfeeding-Part I: Standard and biologic disease modifying anti-rheumatic drugs and corticosteroids. Rheumatology (Oxford) 2016;55:1693-7. [PubMed: 26750124]
- 5.
- Götestam Skorpen C, Hoeltzenbein M, Tincani A, et al. The EULAR points to consider for use of antirheumatic drugs before pregnancy, and during pregnancy and lactation. Ann Rheum Dis 2016;75:795-810. [PubMed: 26888948]
- 6.
- Sammaritano LR, Bermas BL, Chakravarty EE, et al. 2020 American College of Rheumatology Guideline for the Management of Reproductive Health in Rheumatic and Musculoskeletal Diseases. Arthritis Rheumatol 2020;72:529-56. [PubMed: 32090480]
- 7.
- Nguyen GC, Seow CH, Maxwell C, et al. The Toronto Consensus Statements for the Management of IBD in Pregnancy. Gastroenterology 2016;150:734-57.e1. [PubMed: 26688268]
- 8.
- Russell MD, Dey M, Flint J, et al. British Society for Rheumatology guideline on prescribing drugs in pregnancy and breastfeeding: Immunomodulatory anti-rheumatic drugs and corticosteroids. Rheumatology (Oxford) 2023;62:e48-e88. [PMC free article: PMC10070073] [PubMed: 36318966]
- 9.
- Torres J, Chaparro M, Julsgaard M, et al. European Crohn's and Colitis Guidelines on Sexuality, Fertility, Pregnancy, and Lactation. J Crohns Colitis 2023;17:1-27. [PubMed: 36005814]
- 10.
- Azad Khan, AK, Truelove SC. Placental and mammary transfer of sulphasalazine. Br Med J 1979;2:1553. [PMC free article: PMC1597396] [PubMed: 43760]
- 11.
- Järnerot G, Into-Malmberg MB. Sulphasalazine treatment during breast feeding. Scand J Gastroenterol 1979;14:869-71. [PubMed: 44005]
- 12.
- Berlin CM, Jr, Yaffe SJ. Disposition of salicylazosulfapyridine (Azulfidine) and metabolites in human breast milk. Dev Pharmacol Ther 1980;1:31-9. [PubMed: 6108198]
- 13.
- Ambrosius Christensen L, Rasmussen SN, Hansen SH, et al. Salazosulfapyridine and metabolites in fetal and maternal body fluids with special reference to 5-aminosalicylic acid. Acta Obstet Gynecol Scand 1987;66:433-5. [PubMed: 2892343]
- 14.
- Esbjörner E, Järnerot G, Wranne L. Sulphasalazine and sulphapyridine serum levels in children to mothers treated with sulphasalazine during pregnancy and lactation. Acta Paediatr Scand 1987;76:137-42. [PubMed: 2882643]
- 15.
- Branski D, Kerem E, Gross-Kieselstein E, et al. Bloody diarrhea--a possible complication of sulfasalazine transferred through human breast milk. J Pediatr Gastroenterol Nutr 1986;5:316-7. [PubMed: 2870147]
- 16.
- Nelis GF. Diarrhoea due to 5-aminosalicylic acid in breast milk. Lancet 1989;333:383. [PubMed: 2563532]
- 17.
- Föllmer W. Uber die anwendung sulfonamiden im wochenbett. Klin Wochenschr 1941;20:912-3.
- 18.
- Moretti ME, Spiczynski Y, Hashemi G, et al. Prospective follow-up of infants exposed to 5-aminosalicylic acid containing drugs through maternal milk. J Clin Pharmacol 1998;38:867. doi:10.1177/009127009803800901 [CrossRef]
- 19.
- Moretti ME. Prospective follow-up of infants exposed to 5-aminosalicylic acid containing drugs through maternal milk. Theses Canada 1998. https:
//library-archives .canada.ca/eng/services /services-libraries /theses/Pages/item .aspx?idNumber=51446896 - 20.
- Correia LM, Bonilha DQ, Ramos JD, et al. Inflammatory bowel disease and pregnancy: Report of two cases treated with infliximab and a review of the literature. Eur J Gastroenterol Hepatol 2010;22:1260-4. [PubMed: 20671559]
- 21.
- Ikram N, Eudy A, Clowse MEB. Breastfeeding in women with rheumatic diseases. Lupus Sci Med 2021;8:e000491. [PMC free article: PMC8039217] [PubMed: 33832977]
Substance Identification
Substance Name
Sulfasalazine
CAS Registry Number
599-79-1
Drug Class
Breast Feeding
Lactation
Milk, Human
Gastrointestinal Agents
Anti-Inflammatory Agents, Non-Steroidal
Antirheumatic Agents
Sulfonamides
Antibacterial Agents
Anti-Infective Agents
Disclaimer: Information presented in this database is not meant as a substitute for professional judgment. You should consult your healthcare provider for breastfeeding advice related to your particular situation. The U.S. government does not warrant or assume any liability or responsibility for the accuracy or completeness of the information on this Site.
Publication Details
Publication History
Last Revision: February 15, 2024.
Copyright
Attribution Statement: LactMed is a registered trademark of the U.S. Department of Health and Human Services.
Publisher
National Institute of Child Health and Human Development, Bethesda (MD)
NLM Citation
Drugs and Lactation Database (LactMed®) [Internet]. Bethesda (MD): National Institute of Child Health and Human Development; 2006-. Sulfasalazine. [Updated 2024 Feb 15].