CASRN: 303-53-7
Drug Levels and Effects
Summary of Use during Lactation
Amounts of cyclobenzaprine in milk appear to be very small and two infants apparently tolerated the drug in milk well. If cyclobenzaprine is required by the mother, it is not a reason to discontinue breastfeeding. Monitor the infant for (drowsiness, adequate weight gain, and developmental milestones), especially in neonates and preterm infants and when using combinations of sedating drugs.
Drug Levels
Maternal Levels. Two mothers were taking chronic cyclobenzaprine therapy. One mother was taking 5 mg once daily for temporomandibular joint pain and the other mother was taking 10 mg twice daily for fibromyalgia pain. Each collected milk at 0, 1, 2, 4, 6, 8 and 12 hours after a dose. After the 5 mg dose, the peak milk level was 6.6 mcg/L and the average level was 2.2 mcg/L. After the 10 mg dose, the peak milk level was 24.5 mcg/L and the average level was 10.3 mcg/L. These amounts resulted in the respective infant dosages of 0.3 mcg/kg and 0.7 mcg/kg daily. In both cases, the weight-adjusted dosage was 0.5% of the maternal dosage.[1]
Infant Levels. Relevant published information was not found as of the revision date.
Effects in Breastfed Infants
Two mothers were taking chronic cyclobenzaprine therapy. One mother was taking 5 mg once daily for temporomandibular joint pain and the other mother was taking 10 mg twice daily for fibromyalgia pain. The latter mother was also taking unspecified antidepressants, levothyroxine, zolpidem, alprazolam and famotidine. Both mothers were breastfeeding their infants (extent not stated). Neither infant had any noticeable adverse reaction such as sedation.[1]
A search was performed of the shared database of all U.S. poison control centers for the time period of 2001 to 2017 for calls regarding medications and breastfeeding. Of 2319 calls in which an infant was exposed to a substance via breastmilk, 1 of 7 classified as resulting in a major adverse effect involved cyclobenzaprine. A 16-day-old infant was exposed to cyclobenzaprine, acetaminophen and oxycodone in breastmilk. The infant was admitted to the hospital in a noncritical care unit for bradycardia, hypotension, and respiratory arrest. The dosages and extent of breastfeeding were not reported and the infant survived.[2]
Effects on Lactation and Breastmilk
Relevant published information was not found as of the revision date.
Alternate Drugs to Consider
References
- 1.
- Burra B, Datta P, Rewers-Felkins K, et al. Transfer of cyclobenzaprine into human milk and subsequent infant exposure. J Hum Lact. 2019;35:559–62. [PubMed: 31017819]
- 2.
- Beauchamp GA, Hendrickson RG, Horowitz BZ, et al. Exposures through breast milk: An analysis of exposure and information calls to U.S. poison centers, 2001-2017. Breastfeed Med. 2019;14:508–12. [PubMed: 31211594]
Substance Identification
Substance Name
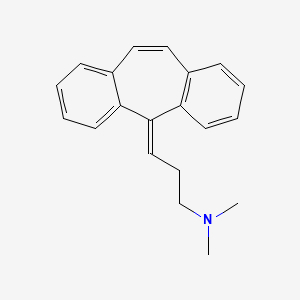
Cyclobenzaprine
CAS Registry Number
303-53-7
Drug Class
Breast Feeding
Lactation
Muscle Relaxants, Central
Disclaimer: Information presented in this database is not meant as a substitute for professional judgment. You should consult your healthcare provider for breastfeeding advice related to your particular situation. The U.S. government does not warrant or assume any liability or responsibility for the accuracy or completeness of the information on this Site.
Publication Details
Publication History
Last Revision: March 17, 2021.
Copyright
Attribution Statement: LactMed is a registered trademark of the U.S. Department of Health and Human Services.
Publisher
National Institute of Child Health and Human Development, Bethesda (MD)
NLM Citation
Drugs and Lactation Database (LactMed®) [Internet]. Bethesda (MD): National Institute of Child Health and Human Development; 2006-. Cyclobenzaprine. [Updated 2021 Mar 17].