NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
Comparative Effectiveness Review Summary Guides for Consumers [Internet]. Rockville (MD): Agency for Healthcare Research and Quality (US); 2005-.
This publication is provided for historical reference only and the information may be out of date.
Is This Information Right for Me?
This information is right for you if
- Your health care professional* said you or your loved one has fecal incontinence (FI). People with FI have trouble holding their stool until they can get to the bathroom. Stool sometimes leaks by accident. FI is also sometimes called “accidental bowel leakage.”
- You want to know what treatments are available for FI and what researchers have found about how well the treatments work.
- You or your loved one are age 18 or older. The information in this summary is from research on adults.
What will this summary tell me?
This summary will answer these questions:
- What is FI?
- What are treatment options for FI?
- What have researchers found about how well FI treatments work?
- What are possible side effects or complications of the treatments?
- What should I discuss with my health care professional?
Note: This summary only discusses research on treatments for FI. It does not cover products that people with FI use, such as pads, disposable underwear, and skin care products.
What is the source of this information?
Researchers funded by the Agency for Healthcare Research and Quality, a Federal Government research agency, reviewed studies on treatments for fecal incontinence published between 1980 and June 2015. The report included 63 studies comparing one treatment to another and 53 studies on only surgery for FI. The report was reviewed by health care professionals, researchers, experts, and the public. You can read the report at www.effectivehealthcare.ahrq.gov/fecal-incontinence.
Understanding Your Condition
What is fecal incontinence?
Fecal incontinence (FI) is a condition in which you have trouble holding your stool until you can get to the bathroom. Stool sometimes leaks by accident. The stool may be solid or liquid. FI is also sometimes called “accidental bowel leakage.”
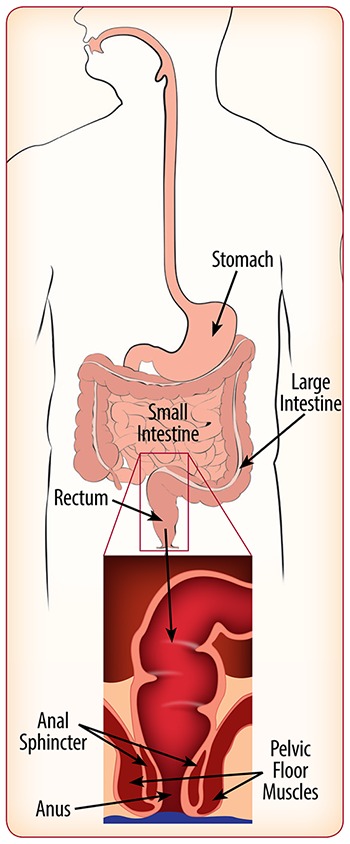
Stool is the waste that passes out of your body during a bowel movement. Stool is made of undigested food and mucus. The mucus is a thick liquid that coats your digestive tract.
Any food that cannot be digested moves into your large intestine as waste. The last part of the large intestine is called the rectum. Waste stays in the rectum until it leaves your body through the anus during a bowel movement.
Muscles and nerves in the rectum and anus keep stool in the rectum until you are ready for a bowel movement. A ring of muscles called the anal sphincter (pronounced SFINK-ter) acts like a rubber band around the anus to keep it closed tightly. The pelvic floor muscles help support the bladder, rectum, and other organs. They also help control bowel movements.
What causes FI?
FI can be caused by many things, including:
- Damage to the sphincter muscles or to the nerves that control the rectum and sphincter muscles
- »
This can happen from childbirth, surgery involving the rectum or anus, or straining often to pass stool.
- »
A spinal cord or brain injury can also damage the nerves that control the rectum and sphincter muscles.
- Loss of stretch or stiffening of the rectum
- »
This can happen from surgery involving the rectum or anus, radiation treatment for cancer, or inflammatory bowel diseases (disorders that cause irritation to the lining of the lower digestive system).
- Swollen blood vessels in and around the lower rectum and anus (called hemorrhoids)
- A condition in which the rectum drops down through the anus (called rectal prolapse)
- Diarrhea
- »
Loose stools are more difficult to hold in than solid stools.
How common is FI?
- About 1 out of every 12 people in the United States has FI. That is equal to almost 18 million people.
- FI is more common in older adults and in women.

What problems can FI cause?
Many people feel embarrassed and upset about their FI. They may avoid social situations because they are afraid of leaking stool. FI can severely limit a person's ability to enjoy work or activities. Untreated FI can lead to skin rashes, infections, and other problems.
Understanding Your Options
How is FI treated?
Many treatments have been used to help people with FI:
- Dietary fiber supplements
- Antidiarrhea medicines
- Bowel training
- Pelvic floor exercises (sometimes done with biofeedback)
- Anal sphincter bulking shots
- Surgery
Dietary Fiber Supplements
Dietary fiber supplements, such as psyllium, can help make your stool less loose. These supplements come as pills or powders.
Antidiarrhea Medicines
If your FI is caused by diarrhea, a medicine can help stop the diarrhea. Examples of antidiarrhea medicines include diphenoxylate (Lomotil®) or loperamide (Imodium®).
Bowel Training
Bowel training means trying to have a bowel movement at certain times of the day. You may try when you wake up each morning or after a meal. It may take several weeks or months to develop a regular pattern.
Pelvic Floor Muscle Training and Biofeedback
For pelvic floor muscle training (PFMT), you squeeze and release the muscles you use to stop a bowel movement. PFMT is sometimes done with biofeedback. Biofeedback helps you become more aware of how your muscles work. It uses sensors placed in the anus and rectum to make you feel like you need to have a bowel movement. The sensors then track when you squeeze your pelvic floor and anal sphincter muscles. This helps your health care professional see if you are squeezing your muscles the right way.
Anal Sphincter Bulking Shots
Anal sphincter bulking shots may help build up the tissue around the anus. The shots are given into the walls of the anus. They help to narrow the opening of the anus to help decrease stool leakage.
Surgery
Surgery may help FI that is caused by damaged nerves or muscles. Surgery is usually suggested only if other treatments do not work. There are several types of surgery for FI.
Sacral Nerve Stimulation
A small device is placed under the skin of your lower back. The device uses electrical pulses to stimulate the nerves that control the muscles in your rectum and anus. The area on your lower back will be numbed so you do not feel pain when the device is placed under the skin. The procedure is usually done in an outpatient center. The device runs on a battery that lasts about 5 years. When the battery runs out, you will need another procedure to replace the device.
Anal Sphincter Repair
If you have a tear in your anal sphincter, your doctor may recommend this type of surgery. A tear can be caused by childbirth or injury. The surgeon reconnects the ends of the muscles to fix the tear. This surgery is also called sphincteroplasty.
Anal Sphincter Replacement
The surgeon places a small cuff around the anus. The cuff connects to a small pump placed under the skin. When the cuff fills with air, it acts like the sphincter muscles to close the anus. To have a bowel movement, you squeeze the pump to let the air out of the cuff so the anus can open.
What have researchers found about treatments for FI?
| Treatment | What Researchers Found |
|---|---|
| The dietary fiber supplement psyllium |
|
| Antidiarrhea medicines |
|
| Bowel training |
|
| Pelvic floor muscle training (PFMT) with biofeedback * |
|
| Anal sphincter bulking shots |
|
| Surgery for FI (sacral nerve stimulation, anal sphincter repair, and anal sphincter replacement) |
|
- *
There is not enough research to know how well PFMT works by itself (without biofeedback).
What are the possible side effects or complications of FI treatments?
All treatments for FI have possible side effects and complications (see the chart on the next page). Just because side effects and complications are possible does not mean you will have them.
Researchers found that:
- People who had surgery for FI had side effects and complications more often than people who used nonsurgery treatments.
- Side effects of nonsurgery treatments were usually mild.
- Complications of surgery were more severe.
- Complications happened most often with anal sphincter replacement surgery.
| Treatment | Possible Side Effects or Complications |
|---|---|
| Nonsurgery treatments | |
| The dietary fiber supplement psyllium |
|
| Antidiarrhea medicines diphenoxylate (Lomotil®) and loperamide (Imodium®) |
|
| Bowel training |
|
| Pelvic floor muscle training with biofeedback |
|
| Anal sphincter bulking shots |
|
| Surgery | |
| Sacral nerve stimulation |
|
| Anal sphincter repair |
|
| Anal sphincter replacement |
|
- *
You may need one or more additional surgeries to fix the problem or to replace or remove the device.
- †
Sepsis is a serious illness that happens when your immune system over-responds to an infection. It causes inflammation in your body. This could lead to blood clots and leaky blood vessels, very low blood pressure, and damage to your internal organs. You may need surgery to help get rid of the infection.
Note: Complications from anal sphincter repair and anal sphincter replacement often require another surgery. In severe cases, some complications may cause you to need a colostomy (pronounced cah-LOSS-tuh-mee). For a colostomy, the surgeon brings the end of your rectum through a small opening in the wall of your belly. As waste is made, it travels through your large intestine and rectum. Then waste travels through the opening in your belly and collects in a pouch outside of your body.
Making a Decision
What should I think about when deciding about treatment?
You may want to talk with your health care professional about
- Issues that concern you, such as needing to run to find a bathroom, needing to go to the bathroom often, being prepared for social situations, and controlling your FI
- The trade-offs between possible benefits and side effects or complications for each treatment
- The cost of the treatments and how much of the cost your insurance covers
Ask your health care professional
- Which treatment do you think may be best for me?
- Might changes in my diet help?
- If I have surgery, how long would my recovery be?
- How long will I need to continue treatment?
- How long will it take to know if the treatment is working? If the treatment does not help, when should I see you to try something different?
- How long will the treatment work? Might it stop working?
- What are the possible benefits and risks of the treatment?
- How will I know if I am having a side effect or complication, and when should I call you?
- How common are side effects or complications for each treatment? How severe might they be?
Source
The information in this summary comes from the report Treatments for Fecal Incontinence, March 2016. The report was produced by the Minnesota Evidence-based Practice Center through funding by the Agency for Healthcare Research and Quality (AHRQ).
For a copy of the report or for more information about AHRQ, go to www.effectivehealthcare.ahrq.gov/fecal-incontinence.
Additional information came from the MedlinePlus® Web site, a service of the National Library of Medicine and the National Institutes of Health. This site is available at www.medlineplus.gov.
This summary was prepared by the John M. Eisenberg Center for Clinical Decisions and Communications Science at Baylor College of Medicine, Houston, TX. People with fecal incontinence reviewed this summary.
Footnotes
- *
Your health care professional may include your primary care physician, gastroenterologist (a doctor who specializes in the digestive system), proctologist (a doctor who specializes in diseases of the colon, rectum, and anus), gynecologist (a doctor who specializes in the female reproductive system), urogynecologist (a doctor who specializes in disorders of the pelvic floor), surgeon, nurse practitioner, or physician assistant.
- Review Prevention of urinary and fecal incontinence in adults.[Evid Rep Technol Assess (Full ...]Review Prevention of urinary and fecal incontinence in adults.Shamliyan T, Wyman J, Bliss DZ, Kane RL, Wilt TJ. Evid Rep Technol Assess (Full Rep). 2007 Dec; (161):1-379.
- Fecal Incontinence and Quality of Life in Adults With Rectal Cancer After Lower Anterior Resection.[J Wound Ostomy Continence Nurs...]Fecal Incontinence and Quality of Life in Adults With Rectal Cancer After Lower Anterior Resection.Lin YH, Chen HP, Liu KW. J Wound Ostomy Continence Nurs. 2015 Jul-Aug; 42(4):395-400.
- Review Noninvasive Treatments for Low Back Pain: A Summary of the Research for Adults.[Comparative Effectiveness Revi...]Review Noninvasive Treatments for Low Back Pain: A Summary of the Research for Adults.John M. Eisenberg Center for Clinical Decisions and Communications Science. Comparative Effectiveness Review Summary Guides for Consumers. 2005
- Review Role of diet in fecal incontinence: a systematic review of the literature.[Int Urogynecol J. 2016]Review Role of diet in fecal incontinence: a systematic review of the literature.Colavita K, Andy UU. Int Urogynecol J. 2016 Dec; 27(12):1805-1810. Epub 2016 Feb 16.
- The prevalence of fecal incontinence and associated risk factors in older adults participating in the SABE study.[Neurourol Urodyn. 2016]The prevalence of fecal incontinence and associated risk factors in older adults participating in the SABE study.Tamanini JT, de Jesus FA, Castro RA, Ferreira Sartori MG, Castello Girão MJ, Dos Santos JL, de Oliveira Duarte YA, Lebrão ML. Neurourol Urodyn. 2016 Nov; 35(8):959-964. Epub 2015 Aug 21.
- Treatments for Fecal Incontinence - Comparative Effectiveness Review Summary Gui...Treatments for Fecal Incontinence - Comparative Effectiveness Review Summary Guides for Consumers
Your browsing activity is empty.
Activity recording is turned off.
See more...