NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
Comparative Effectiveness Review Summary Guides for Consumers [Internet]. Rockville (MD): Agency for Healthcare Research and Quality (US); 2005-.
This publication is provided for historical reference only and the information may be out of date.
Is This Guide Right for Me?
This guide is for patients who have been
- Diagnosed with head and neck cancer.
- Need radiation therapy to treat that cancer.
This guide is to help you decide which type of radiation therapy you should choose to treat your head and neck cancer.
What does the guide cover?
Radiation can either be delivered from a machine outside of your body (called “external-beam radiation therapy”) or can be placed inside your body (called “brachytherapy”).
This guide only covers external-beam radiation therapy.
This guide explains differences among four types of radiation therapy and possible side effects.
This guide does not cover other forms of treatment for your head and neck cancer that you may be getting or have received, such as chemotherapy or surgery. This guide does not cover treatments for brain cancer or thyroid cancer.
If you are not sure if this guide is right for you, ask your doctor, nurse, or other health care professional.
Where does the information come from?
The information in this guide comes from a review of many different studies on radiation therapy for head and neck cancer. It is not based on a single study but on many studies looked at together by a team of researchers, doctors, and other experts.
Understanding Your Disease
What is cancer of the head and neck?
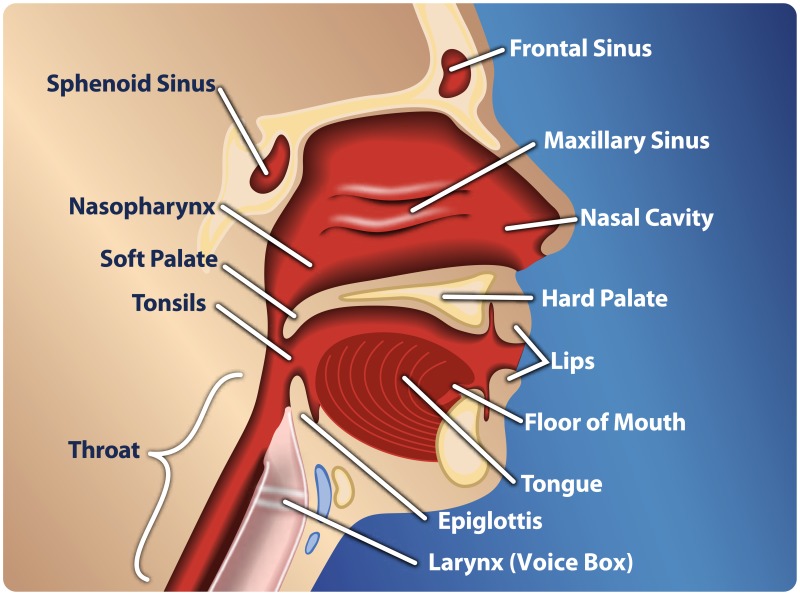
Most types of head and neck cancer start in the cells lining the open cavities of the head and neck, such as the sinuses, nasal cavity, mouth, or throat. Other kinds of head and neck cancer can occur in the salivary glands. These glands produce the fluid, called “saliva” or spit, that keeps your mouth and throat moist. Cancer of the brain and thyroid is not classified as head and neck cancer.
According to the National Cancer Institute, head and neck cancer accounts for nearly 3 to 5 percent of all cancer in the United States. These types of cancer are more common in men and in people older than age 50. Around 47,560 men and women in this country develop head and neck cancer every year. Tobacco and alcohol use are common risk factors for this cancer.
How is head and neck cancer treated?
There are several ways that doctors can treat head and neck cancer, including:
- Surgery, where a part or all of the tumor or cancer cells are removed.
- Chemotherapy, where certain drugs are used to kill cancer cells.
- Radiation therapy, where waves of energy are sent to kill cancer cells in and around the tumor.
Often, these treatments are used together. This guide is only about radiation therapy.
Understanding Radiation Therapy
What is radiation therapy?
How radiation treats your cancer
High-energy radiation is delivered to cancer cells or a tumor.
Radiation therapy works in two ways:
- Radiation can stop or slow the growth of the cancer.
- Radiation can shrink tumors, reduce some symptoms, and relieve pain.
Radiation therapy does not kill cancer cells right away. You may need several days or weeks of treatment with radiation before cancer cells start to die. Cancer cells will keep dying for weeks or months after radiation therapy is finished.
Radiation therapy starts with a plan
Your doctors will make a detailed radiation plan for your treatment. The plan includes:
- Where to aim the radiation beams.
- How much radiation you should get.
The goal of the plan is to provide the right amount of radiation to stop your tumor from growing or shrink it. The doctors want to protect you from any harm caused by the radiation, especially to the healthy cells around the tumor.
Different systems to deliver radiation
Doctors use different systems and tools to make the radiation therapy plan and deliver your radiation therapy. The approach your doctor may use to target the tumor, aim the radiation beams, and change the strength of the beams while they are being given has changed over time. Using different beam strengths may help protect you from the side effects of radiation.
What are the side effects of radiation therapy?
Everyone is different
Radiation therapy can cause damage to normal, healthy cells near and around your cancer. The damage may cause side effects. These side effects can be very different for different people. Your side effects may depend on the:
- Dose and type of radiation used.
- Site of your cancer.
- Stage of your cancer.
- Your age.
Types of side effects
Side effects can appear around 2 weeks after the first radiation treatment or much later and can include:
- Mouth sores (feels like little cuts or ulcers in your mouth).
- Dry mouth (also called “xerostomia” [pronounced zero-STOH-mee-ah]).
- Pain or difficulty with swallowing.
- Changes in taste or smell.
- Changes in the sound of your voice.
- Jaw stiffness and jaw bone decay.
- Changes in your skin.
- Feeling tired.
What impact can these side effects have?
Radiation therapy does not hurt when it is given. Some of the side effects can hurt or affect your quality of life however, even when the radiation helps to stop or slow down your cancer. Some side effects last only a few days. Other side effects can last weeks, months, or longer.
Some side effects, like dry mouth (xerostomia), may not ever get better. Your saliva, or spit, is used for many things. Saliva is needed as you eat to help you swallow your food. Saliva also helps to protect you from tooth decay, as well as tongue and gum disease, by keeping bacteria from settling on your teeth, tongue, and gums. Saliva even plays a role in speaking.
Understanding Your Choices
What are the differences between radiation systems?
There are four external-beam radiation systems that doctors can use to treat your cancer. The first three of these have been used successfully to treat head and neck cancer for a number of years.
- The oldest system is called Two-Dimensional Radiation Therapy or 2DRT. This system targets the tumor using a two-dimensional image, much like a picture or photograph. The beams can only be aimed at a few angles and do not change strength while they are being given. 2DRT is not used as often as the newer systems.
- A newer sytem is called Three-Dimensional Conformal Radiation Therapy or 3DCRT. This system uses three-dimensional images that let doctors better target the tumor. The images are made with a computed tomography (CT) or magnetic resonance imaging (MRI) machine. The beams can be aimed at more angles than 2DRT to limit the amount of radiation to the normal areas around the tumor.
- A more recent system is called Intensity-Modulated Radiation Therapyor IMRT. This system is similar to 3DCRT, but the doctor can adjust the amount of radiation you get from each beam. This is done to try to reduce injury to the healthy areas around the tumor.
- Another system uses a different kind of energy beam to treat your tumor. This system is called Proton-Beam Radiation Therapy or PBRT. There is very little information about how well this form of radiation therapy works, and it is not widely used.
Which type of radiation therapy is most effective for my cancer?
- Doctors do not know if one type of radiation therapy is more effective than others in stopping or slowing down the growth of your head and neck cancer.
- Doctors do not know if any one type of radiation therapy will control your cancer better or help you live longer.
Which type may have fewer side effects?
- There is some evidence that IMRT causes less damage to the glands that make your saliva (the fluid or spit in your mouth) when compared to 2DRT or 3DCRT. Early results from a recent study suggest that when patients were examined 1 year after treatment, those who were treated with IMRT experienced dry mouth (xerostomia) less often than those who were treated with 2DRT or 3DCRT.
- While doctors think that IMRT may help avoid damage to other normal organs in the head and neck—such as your eyes, brain, and other glands—they do not know this for sure.
- The skill and experience of your doctors in using each type of radiation therapy may be important. The current studies were conducted in centers associated with universities and medical schools. Doctors do not know if the results are different in other types of medical centers.
- Doctors do not know how the side effects of PBRT compare to the other three types of radiation therapy.
Making a decision
What questions should I ask my doctor?
- What side effects of radiation therapy am I most likely to have, when might they occur, and how long might they last?
- Which forms of radiation therapy are available to me?
- How much experience do the doctors and medical staff here have with each form of radiation therapy?
- How do you make sure that the tumor and the tissues around it get the right amount of radiation?
Other questions for your doctor:
_____________________________________________________________________________
_____________________________________________________________________________
_____________________________________________________________________________
_____________________________________________________________________________
_____________________________________________________________________________
_____________________________________________________________________________
_____________________________________________________________________________
Write the answers here:
_____________________________________________________________________________
_____________________________________________________________________________
_____________________________________________________________________________
_____________________________________________________________________________
_____________________________________________________________________________
_____________________________________________________________________________
_____________________________________________________________________________
Sources
The information in this guide comes from the report Comparative Effectiveness and Safety of Radiation Therapy Treatments for Head and Neck Cancer. It was produced by the Blue Cross and Blue Shield Association Technology Evaluation Center Evidence-based Practice Center through funding by the Agency for Healthcare Research and Quality (AHRQ). For a copy of the report or for more information about AHRQ and the Effective Health Care Program, go to www.effectivehealthcare.ahrq.gov. Additional information was provided by the National Cancer Institute (www.cancer.gov).
- Review Radiation Therapy for Head and Neck Cancer: A Summary for Adults and Their Caregivers.[Comparative Effectiveness Revi...]Review Radiation Therapy for Head and Neck Cancer: A Summary for Adults and Their Caregivers.John M. Eisenberg Center for Clinical Decisions and Communications Science. Comparative Effectiveness Review Summary Guides for Consumers. 2005
- Review Treating Prostate Cancer: A Guide for Men With Localized Prostate Cancer .[Comparative Effectiveness Revi...]Review Treating Prostate Cancer: A Guide for Men With Localized Prostate Cancer .Eisenberg Center at Oregon Health & Science University. Comparative Effectiveness Review Summary Guides for Consumers. 2005
- Review A systematic overview of radiation therapy effects in head and neck cancer.[Acta Oncol. 2003]Review A systematic overview of radiation therapy effects in head and neck cancer.Zackrisson B, Mercke C, Strander H, Wennerberg J, Cavallin-Ståhl E. Acta Oncol. 2003; 42(5-6):443-61.
- A prospective survey of radiotherapy in Sweden.[Acta Oncol. 1996]A prospective survey of radiotherapy in Sweden.. Acta Oncol. 1996; 35 Suppl 6:47-56.
- Pilot study of intraoperative high dose rate brachytherapy for head and neck cancer.[Radiother Oncol. 1996]Pilot study of intraoperative high dose rate brachytherapy for head and neck cancer.Nag S, Schuller D, Pak V, Young D, Grecula J, Bauer C, Samsami N. Radiother Oncol. 1996 Nov; 41(2):125-30.
- Understanding Radiotherapy for Head and Neck Cancer - Comparative Effectiveness ...Understanding Radiotherapy for Head and Neck Cancer - Comparative Effectiveness Review Summary Guides for Consumers
Your browsing activity is empty.
Activity recording is turned off.
See more...