NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
Comparative Effectiveness Review Summary Guides for Consumers [Internet]. Rockville (MD): Agency for Healthcare Research and Quality (US); 2005-.
This publication is provided for historical reference only and the information may be out of date.
Is this information right for me?
Yes, this information is right for you if
- Your doctor* said all tests show you have localized prostate cancer (the cancer has not spread outside the prostate gland).
This information may not be helpful to you if
- Your prostate cancer has spread to other parts of your body.
What will this summary tell me?
This summary will tell you about
- What localized prostate cancer is
- Common treatment options for localized prostate cancer (watchful waiting, active surveillance, surgery to remove the prostate gland, radiation therapy, and hormone treatment)
- What researchers found about how the treatments compare
- Possible side effects of the treatments
- Things to talk about with your doctor
This summary does not cover
- How to prevent prostate cancer
- Less common treatments for localized prostate cancer, such as high-intensity focused ultrasound (high-energy sound waves), cryotherapy (freezing treatment), proton-beam radiation therapy (radiation with a beam of protons instead of x-rays), and stereotactic body radiation therapy (high-energy focused radiation)
- Herbal products or vitamins and minerals
- Treatments (such as chemotherapy) for cancer that has spread outside the prostate gland
What is the source of the information?
Researchers funded by the Agency for Healthcare Research and Quality, a Federal Government research agency, reviewed studies on treatments for localized prostate cancer published between January 1, 2007, and March 7, 2014. The report included 52 studies and was reviewed by health care professionals, researchers, experts, and the public. You can read the report at www.effectivehealthcare.ahrq.gov/prostate-cancer.
Understanding Your Condition
What is localized prostate cancer?
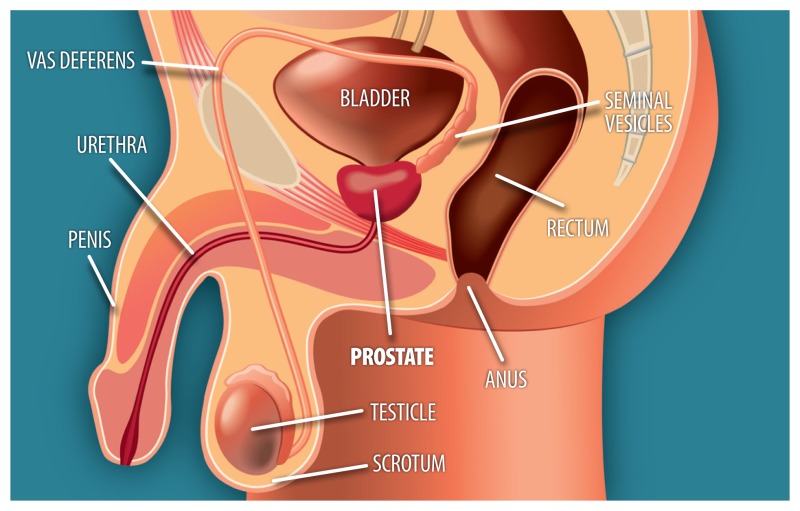
Localized prostate cancer is cancer that is only inside your prostate gland and has not spread to other parts of your body. The prostate is a gland in men about the size of a walnut. It makes and stores the liquid that carries sperm.
The prostate is near the bladder and rectum (the last part of the bowel before the anus). It is just below the bladder and surrounds the upper part of the urethra (the tube that drains urine from the bladder).
Most men with localized prostate cancer have few or no symptoms. Possible symptoms can include:
- Problems when you urinate (such as pain or burning, difficulty starting or stopping, or a weak flow)
- Pain in your lower back
- Pain when you ejaculate
- Blood in your urine
Note: It is important to note that most men with these symptoms do not have prostate cancer. As men get older, their prostate gland may grow larger over time. This, and other health conditions, can cause these symptoms in men who do not have prostate cancer.
How common is prostate cancer?
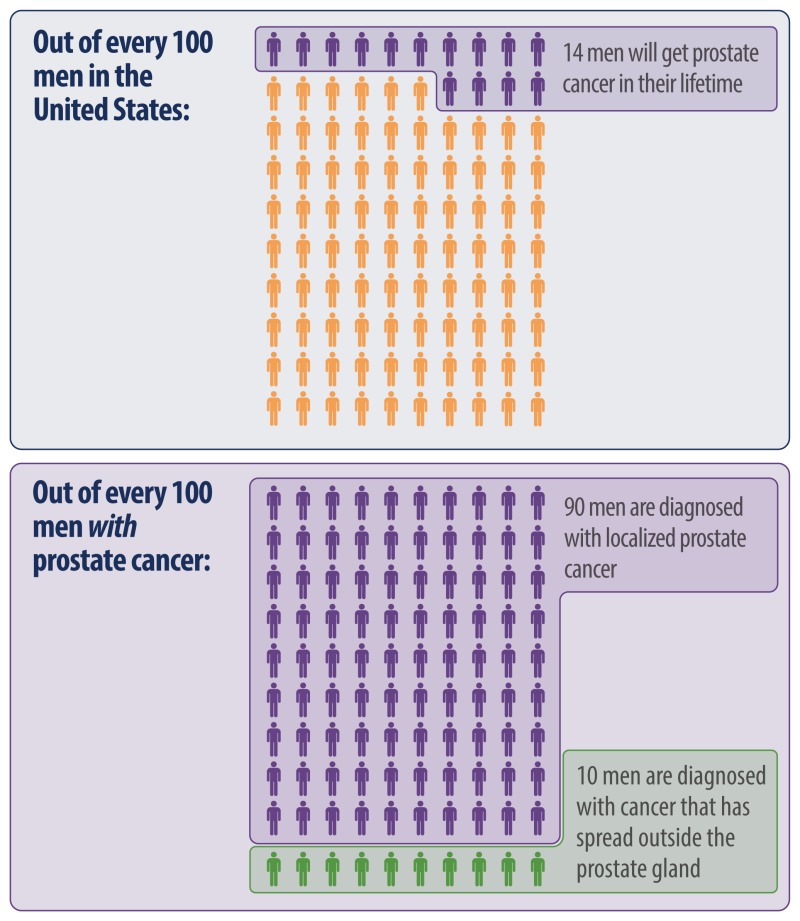
Prostate cancer is the most common cancer in men other than skin cancer.
Who is at risk for prostate cancer?
- Men aged 50 years or older have a higher risk of prostate cancer.
- Prostate cancer is more common in African Americans.
- The risk of prostate cancer is higher for men with a history of prostate cancer in their family.
What tests check for prostate cancer?
Common tests to check for prostate cancer include:
- Digital rectal exam: Your doctor inserts a finger into your rectum and touches your prostate gland. The doctor feels the shape of the prostate gland and checks for any hard spots.
- PSA blood test: This blood test tells how much PSA (a protein made by the prostate gland) is in your blood. Many men with prostate cancer have PSA levels that are higher than normal or that have gotten higher over time.
- –
A high PSA level does not always mean a man has prostate cancer. As men get older, their prostate gland may grow larger over time. This growth, and other health conditions, can cause a high PSA level in men who do not have prostate cancer.
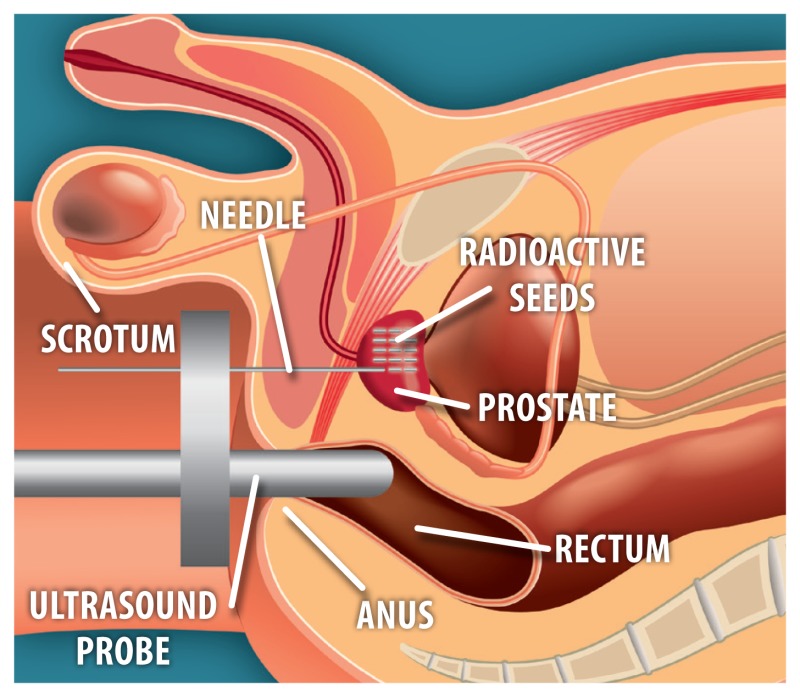
If the test results are not normal, your doctor may recommend more tests, such as a biopsy. During a biopsy, the doctor uses a needle to take out a tiny piece or pieces of the prostate gland. An ultrasound probe may be used to guide the needle. Another doctor called a pathologist (puh-THOL-o-jist) looks at the tissue under a microscope to check for cancer cells.
What if my biopsy shows cancer?
If the biopsy shows prostate cancer, your doctor will determine how likely your cancer is to grow quickly and spread. Sometimes, prostate cancer grows slowly over many years. But other times, it grows quickly.
Your doctor can use your PSA level, Gleason score, and tumor score (T-score) to determine your risk level. The following pages give more information about Gleason score, T-score, and prostate cancer risk levels.
Gleason Score
The Gleason score is a common scale used to determine how fast your prostate cancer is likely to grow. Gleason scores can range from 2 to 10, but most often range from 6 to 10. The higher the Gleason score, the more likely your cancer is to grow and spread.
Tumor Score (T-score)
The T-score tells how far your prostate cancer has grown.
- T1: The cancer is too small to be felt during a digital rectal exam or seen in an imaging test (such as an ultrasound). The cancer is found from a biopsy done after a man has a high PSA level or has surgery for problems urinating. The cancer is only in the prostate gland.
- T2: The cancer can be felt during a digital rectal exam and may be seen in an imaging test. The cancer is still only in the prostate gland.
- –
T2a: The cancer is in one-fourth of the prostate gland (half of the left or right side).
- –
T2b: The cancer is in more than one-fourth of the prostate gland (more than half of one side), but has not grown into the other side of the prostate gland.
- –
T2c: The cancer has grown into both sides of the prostate gland.
- T3: The cancer has grown outside the prostate gland (T3a). The cancer may have spread to the seminal vesicles (T3b), the pair of glands attached to the prostate gland that help make semen.
- T4: The cancer has grown outside the prostate gland into nearby tissues, such as the rectum or bladder. Prostate cancer also commonly spreads to the lymph nodes (also called lymph glands) and bone.
Note: In men with localized prostate cancer, all tests show the cancer is only inside the prostate gland and has not spread to other parts of the body.
Risk Level
Your doctor may use your PSA level, Gleason score, and T-score to determine the risk that your prostate cancer could grow and spread with no treatment or come back after treatment.
Your risk level can help you and your doctor decide what treatment may be best for you. Talk with your doctor about whether your cancer is low, medium, or high risk and what that means for your treatment options.
| Risk Level* | PSA Level | Gleason Score | T-Score |
|---|---|---|---|
| Low risk † | 10 or less | 6 or less | T1–T2a |
| Medium risk †† | 10 to 20 | 7 | T2b–T2c |
| High risk †† | Greater than 20 | 8 or higher | T3a |
- *
From the 2015 clinical practice guideline published by the National Comprehensive Cancer Network.
- †
To be low risk, you must meet the PSA level, Gleason score, and T-score values listed (all three).
- ††
To be medium or high risk, you must meet at least two of the values listed for PSA level, Gleason score, and T-score.
Understanding Your Options
How is localized prostate cancer treated?
There are many treatments for localized prostate cancer. The type of treatment your doctor suggests depends on many things. These may include your risk level, your age, and any other health problems. It is important to take time to learn about your cancer, your options for treatment, and possible side effects. Most men diagnosed with localized prostate cancer do not die from the disease.
Treatments for localized prostate cancer include:
- Watchful waiting
- Active surveillance
- Surgery to remove the prostate gland
- Radiation therapy
- Hormone therapy
Watchful Waiting
With watchful waiting, your doctor will watch you over time to see what happens with your cancer. If new symptoms start or old symptoms get worse, your doctor will help you manage them. Your doctor will not do any tests to see if your cancer is growing.
Active Surveillance
With active surveillance, your doctor will closely monitor you at regular checkups. During checkups, your doctor may do a digital rectal exam, a PSA blood test, a biopsy, or other tests to see if the cancer is growing. If tests show your cancer is starting to grow, your doctor will talk with you about other treatment options.
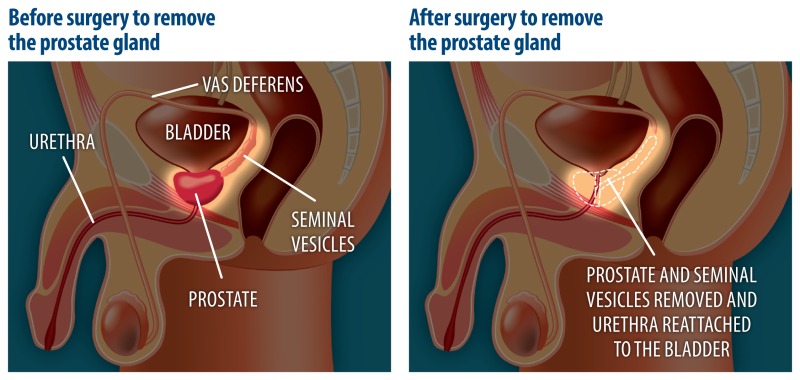
Surgery To Remove the Prostate Gland
In this type of surgery, the surgeon removes the prostate gland and seminal vesicles (the pair of glands attached to the prostate gland that help make semen). The prostate gland surrounds the upper part of the urethra (the tube that carries urine from the bladder). So, that part of the urethra must be removed as well. The remaining urethra is reattached to the bladder. The surgeon may also remove lymph nodes or other tissues around the prostate gland to check if the cancer has spread.
Radiation Therapy
For this type of therapy, your doctor uses radiation to kill the prostate cancer cells.
Radiation can be given in two ways:
- External-beam radiation: This type of radiation treatment uses a machine to aim high-energy radiation beams at the cancer cells in your prostate gland. You lie on a table under the machine. The goal is to aim the beams only at the cancer cells and not to hurt the healthy tissues around the cancer. There are many different ways to give external-beam radiation. For example, the beams can be sent from different angles or at different strengths. Radiation treatment is given a few minutes a day, 5 days a week, for 8 to 9 weeks.
- Brachytherapy: This type of radiation is also called “radiation seeding.” You will be given medicine so you do not feel pain. The doctor then uses an ultrasound probe to guide the needles that place small radioactive seeds (about the size of a grain of rice) into your prostate gland. The seeds slowly release radiation over time. Once the seeds stop releasing radiation, they stay in the prostate gland and do not need to be removed. This type of radiation is done in one visit, usually as an outpatient procedure.
Hormone Therapy
Prostate cancer cells need the male hormone testosterone to grow. Hormone therapy lowers the amount of testosterone in the body or blocks the effects of testosterone. This helps to slow or stop the cancer from growing. Hormone therapy comes as shots or pills.
- Hormone medicines that lower the amount of testosterone in the body include leuprolide (Lupron®, Viadur®, Eligard®) and goserelin (Zoladex®).
- Hormone medicines that block the effects of testosterone include flutamide (Eulexin®) and bicalutamide (Casodex®).
Hormone therapy is sometimes used together with radiation. It is also sometimes given before surgery to remove the prostate gland.
What have researchers found about how these treatments compare with each other?
Deciding which treatment may be best for you depends on many things, including your cancer risk level, what researchers have found about the treatments, and what is important to you regarding possible benefits and side effects of the treatments.
Researchers found that for some men:
- The risk of the cancer spreading to other parts of the body is much lower with surgery to remove the prostate gland than with watchful waiting.
- Surgery to remove the prostate gland appears to increase the chance of surviving the cancer more than external-beam radiation therapy.
- A combination of 3D-CRT (a type of external-beam radiation therapy) and hormone therapy appears to increase the chance of surviving the cancer more than 3D-CRT alone.
Note: In the time since this research was done, advances have been made in treatments for localized prostate cancer. Improved treatments and new treatments may now work better to treat localized prostate cancer.
Research is only one source that helps guide doctors when they treat localized prostate cancer. Doctors also rely on their experience and on guidelines for treatment based on evidence and recommendations by experts.
When thinking about what treatment may be best for you, your doctor will consider several things, including:
- Your age
- Your cancer risk level
- Your medical history
- Other health problems you may have
- How long you are expected to live
- Your preferences
Your doctor will also discuss possible side effects to help you decide about treatment. Talk with your doctor about your options and the trade-offs between possible benefits and side effects. Usually you have time to think about your options before making a decision.
Note: In recent years (after much of the current research was done), more cases of localized prostate cancer are being found at very early stages using the PSA blood test. More research is needed to know which men whose prostate cancer is in a very early stage may benefit more from active surveillance than from other treatments. If your prostate cancer is in a very early stage, talk with your doctor about which treatment may be best for you.
What are possible side effects of treatments for localized prostate cancer?
All treatments can cause side effects. The most common side effects are urinary bowel, and sexual problems. Some problems happen soon after treatment, but others develop over time. Some side effects may get better, but some may last a long time or may never go away. Talk with your doctor if you have any side effects. There may be ways to help manage them.
| POSSIBLE SIDE EFFECTS | OTHER INFORMATION | |
|---|---|---|
| Active Surveillance |
|
|
| Surgery To Remove the Prostate Gland |
| |
Radiation Therapy
|
| |
| Hormone Therapy |
|
|
- *
Not always being able to control your urine or leaking urine. The leaking of urine could be very minor dripping, or it could be more severe.
- **
This is becoming less common with newer surgery techniques.
- †
Men who may wish to father a child in the future can talk with their doctor about “banking” their sperm before surgery to remove the prostate gland or radiation therapy.
- ††
Part of your intestine, other organs, or belly fat may poke through an opening at the place where the surgery was done or through a weak spot in the muscles of your abdomen. You may need surgery to fix the hernia.
- §
Such as diarrhea, blood in the stool, leaking stool from the rectum, and rectal pain.
- §§
Such as needing to urinate more often, a burning feeling when urinating, and blood in the urine.
Making a Decision
What should I think about when deciding on treatment?
There are several things to think about when deciding which treatment is right for you. You may want to talk with your doctors about:
- How likely your cancer is to grow, spread, or cause other problems in your lifetime
- Which type of treatment might be best for you
- The trade-offs between possible benefits and possible side effects of the treatments
- Discussing treatment options with your partner or other family members
- How often you will need to see your doctor for treatment
Ask your doctors
- How long may I live with my cancer?
- How likely is my cancer to grow and spread?
- Is watchful waiting or active surveillance an option for me?
- If I use active surveillance, how often should I come in for checkups? What will we do if the cancer starts to grow or spread?
- Which treatment do you think might be best for me based on my age, risk level, and other health issues?
- What is the chance that the treatment might help me to live longer?
- What will my quality of life be with the treatment?
- What side effects of treatment should I watch for and how will they be managed?
- How might treatment affect my sex life?
- If I have surgery to remove my prostate gland, how long might it take to recover?
- Are there local support groups I can join?
Sources
The information in this summary comes from the report Therapies for Clinically Localized Prostate Cancer: Update of a 2008 Systematic Review, December 2014. The report was produced by the ECRI Institute–Penn Medicine Evidence-based Practice Center through funding by the Agency for Healthcare Research and Quality (AHRQ).
For a copy of the report or for more information about AHRQ, go to www.effectivehealthcare.ahrq.gov/prostate-cancer.
Additional information came from the MedlinePlus® Web site, a service of the National Library of Medicine and the National Institutes of Health. This site is available at www.nlm.nih.gov/medlineplus.
This summary was prepared by the John M. Eisenberg Center for Clinical Decisions and Communications Science at Baylor College of Medicine, Houston, TX. Men with localized prostate cancer reviewed this summary.
Footnotes
- *
In this summary, the term doctor refers to your health care professional, including your primary care physician, urologist, oncologist, nurse practitioner, or physician assistant.
- Review Treating Prostate Cancer: A Guide for Men With Localized Prostate Cancer .[Comparative Effectiveness Revi...]Review Treating Prostate Cancer: A Guide for Men With Localized Prostate Cancer .Eisenberg Center at Oregon Health & Science University. Comparative Effectiveness Review Summary Guides for Consumers. 2005
- Review Management of localised prostate cancer: watchful waiting, surgery or radiation therapy, depending on the natural course, which is often relatively slow.[Prescrire Int. 2012]Review Management of localised prostate cancer: watchful waiting, surgery or radiation therapy, depending on the natural course, which is often relatively slow.. Prescrire Int. 2012 Oct; 21(131):242-8.
- Review Treatments for Localized Prostate Cancer: Systematic Review to Update the 2002 U.S. Preventive Services Task Force Recommendation[ 2011]Review Treatments for Localized Prostate Cancer: Systematic Review to Update the 2002 U.S. Preventive Services Task Force RecommendationChou R, Dana T, Bougatsos C, Fu R, Blazina I, Gleitsmann K, Rugge JB. 2011 Oct
- The Prostate cancer Intervention Versus Observation Trial:VA/NCI/AHRQ Cooperative Studies Program #407 (PIVOT): design and baseline results of a randomized controlled trial comparing radical prostatectomy to watchful waiting for men with clinically localized prostate cancer.[Contemp Clin Trials. 2009]The Prostate cancer Intervention Versus Observation Trial:VA/NCI/AHRQ Cooperative Studies Program #407 (PIVOT): design and baseline results of a randomized controlled trial comparing radical prostatectomy to watchful waiting for men with clinically localized prostate cancer.Wilt TJ, Brawer MK, Barry MJ, Jones KM, Kwon Y, Gingrich JR, Aronson WJ, Nsouli I, Iyer P, Cartagena R, et al. Contemp Clin Trials. 2009 Jan; 30(1):81-7. Epub 2008 Aug 23.
- Review Maximizing resources in the local treatment of prostate cancer: A summary of cost-effectiveness studies.[Urol Oncol. 2017]Review Maximizing resources in the local treatment of prostate cancer: A summary of cost-effectiveness studies.Muralidhar V, Nguyen PL. Urol Oncol. 2017 Feb; 35(2):76-85. Epub 2016 Jul 27.
- Treating Localized Prostate Cancer - Comparative Effectiveness Review Summary Gu...Treating Localized Prostate Cancer - Comparative Effectiveness Review Summary Guides for Consumers
Your browsing activity is empty.
Activity recording is turned off.
See more...