Summary of Study Characteristics
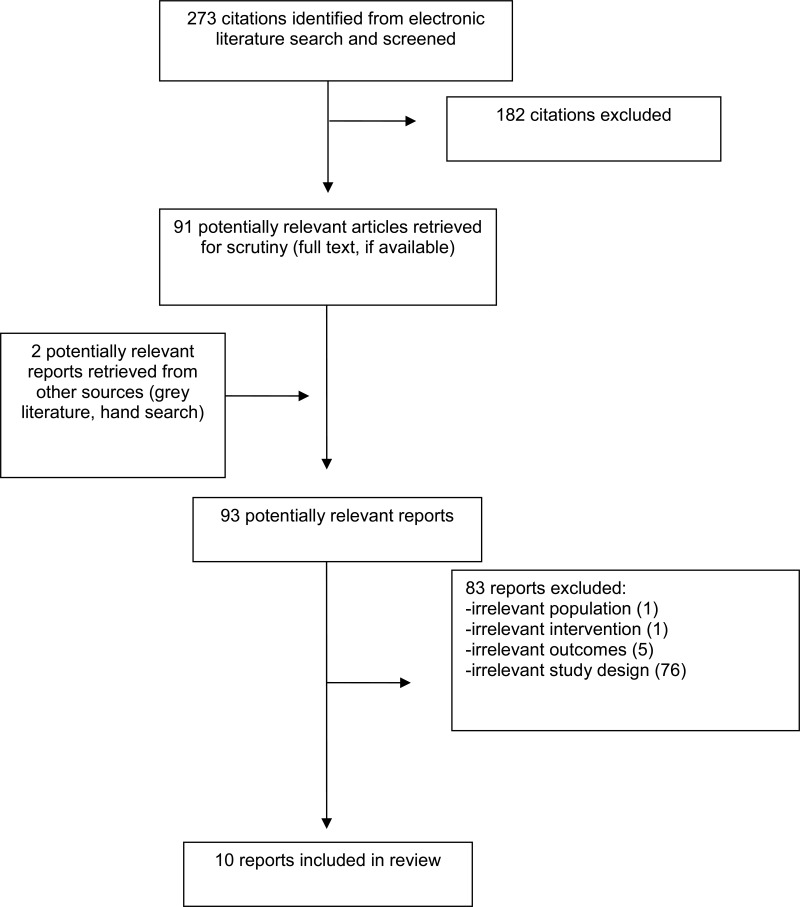
Overall, 10 publications met the inclusion criteria and were included in this report: two systematic reviews, six RCTs, and two non-randomized studies.
Additional details regarding the characteristics of included publications are provided Appendix 2.
Study Design
Two systematic reviews met the inclusion criteria listed in and were included in the current Rapid Response report: a systematic review and meta-analysis examining immediate allergic reactions to GBCAs and a systematic review examining the presence of GBCA depositions in the brain and neurotoxicity.
The systematic review and meta-analysis of immediate allergic reactions to GBCAs was published in 2018 and included nine non-randomized studies. The authors searched PubMed and Google Scholar for published studies until February 2017. The included studies were published from 2011 onwards, with study periods ranging from 2000 to 2016.16
The systematic review of GBCA depositions in the brain was published in 2017 and included 25 publications (19 MRI analyses, three case reports, and three autopsy reports), The authors did not report their search date range; however, the search was completed in July 2016 and the included studies dated back to 2014.17
There was no overlap in the included studies of the two systematic reviews, as outlined in Appendix 5.
In addition, eight clinical studies also met the inclusion criteria outlined in . The first study was a multicenter, double-blind RCT that utilized a crossover design.6 Another five studies were RCTs,4,7,18–20 and the remaining two studies were non-randomized, open-label clinical trials.5,21 Three of the five RCTs were multicenter RCTs, and the remaining two were conducted at single centers.7,20 Furthermore, two RCTs were double-blinded,19,20 two were single-blinded,4,18 and one RCT did not specify any blinding procedure.7 The nonrandomized trials obtained two sets of MRIs from each patient, the first being unenhanced (i.e. with no contrast agent administered), and the second enhanced with contrast agent.5,21
Country of Origin
The first author of the systematic review and meta-analysis of allergic reactions to GBCAs was from the United States of America (USA)16 and the first author of the systematic review of GBCA depositions in the brain was from Poland.17
Of the eight clinical trials, three were conducted in the USA,5,6,20 three were conducted in Japan, 4,7,21 one was conducted in China,18 and one was conducted in Switzerland.19
Patient Population
The systematic review and meta-analysis of allergic reactions included studies where rates of immediate (timeframe not defined) allergic reactions to GBCAs were reported; details of the patient population for the nine included studies were limited to the type of GBCA administered.16 The systematic review of GBCA depositions in the brain included patients who had MRI examinations with GBCAs. Among the 19 studies and autopsy reports included in the review, the authors presented the number of GBCA administrations as well as the contrast agent.17
In the study that utilized a randomized crossover trial design, men and women at least 18 years of age who were referred for contrast-enhanced MRI of the central nervous system (CNS) were recruited from 51 centers worldwide. Patients who were pregnant, breastfeeding, had a history of severe allergic reaction, or had underlying diseases (such as cardiovascular, kidney or liver diseases) were excluded from the study. Additionally, any patient who had been administered any contrast agent within 24 hours of the study MRI or were taking medications that may have interfered with the study were excluded.6
One RCT involved male and female patients at least 20 years of age who were referred for contrast-enhanced MRI based on their current clinical symptoms, or the results of a previous imaging procedure. Included patients had to be clinically stable. The exclusion criteria were patients who were pregnant, breastfeeding, had a history of severe allergic reaction, severe cardiovascular disease or chronic renal failure. Patients who had participated in any gadobutrol studies, had received or were to receive a contrast agent within 24 hours of the first contrast agent administration, and those who had contraindications to the MRI procedures or gadolinium-based contrast agent use were also excluded.4
The RCT conducted in China recruited patients from four centers. The patients were between 18 and 65 years of age, had known or suspected CNS lesions (cranial and/or spinal) and were referred for a contrast-enhanced MRI. Patients who were pregnant, breastfeeding, had hypersensitivity to contrast media, or had severely impaired liver or kidney function (or other underlying diseases) were excluded from the study. Patients were also excluded from the study if they had received or were to receive a contrast agent within 24 hours of the first contrast agent administration or had contraindications to the MRI procedures or the contrast agent used.18
The Japanese RCT included patients between 20 to 85 years of age, weighing 45 to 70 kg and were scheduled for a contrast-enhanced MRI of the brain at Kitasato University Hospital between November 2007 and February 2010. Patients were excluded from the study if their serum-creatinine levels were ≥ 1.6 mg/dL within 3 months prior to the MRI procedure, or if they were unable to comply with the study protocol.7
In one RCT conducted by Semelka et al., the patient population was not well described. The 59 included patients were described as having an age range of 5 to 85 years, with a mean age of 52 years. The patients were comprised of 31 men and 28 women.20
The RCT conducted in Switzerland studied patients who were at least 18 years of age, had suspected or known focal liver lesions, and required a contrast-enhanced liver MRI. Patients were excluded if they had received an investigational drug within 30 days prior to entering the study or were contraindicated for contrast-enhanced MRI.19
The first non-randomized clinical trial, conducted by Gutierrez et al., recruited patients from 22 centers in Argentina, China, Colombia, South Korea and the USA between December 2007 and December 2008. The study examined patients at least 18 years of age, who were referred for a contrast-enhanced MRI of the CNS. Patients were excluded if they were pregnant, breastfeeding, had a history of severe allergic reactions, or had any underlying diseases (including liver or kidney diseases/injuries). Patients who had participated in any clinical studies 30 days prior to enrollment (including any gadobutrol studies), had received a contrast agent within 24 hours of the first contrast agent administration, and those who had contraindications to the MRI procedures or gadolinium-based contrast agent use were also excluded. Additionally, patients who were taking medications that may have interfered with the study were excluded, as well as any patients who were scheduled to receive a contrast agent or any therapeutic procedure 72 hours after their study MRI.5
The second non-randomized clinical trial examined men and women at least 18 years of age with any indication who were referred for a contrast-enhanced MRI of the CNS. Like the non-randomized study performed by Gutierrez et al., patients who were pregnant, breastfeeding, had a history of severe allergic reactions, received a contrast agent 24 hours prior to the study MRI, or participated in any clinical studies 30 days prior to enrollment (including any gadobutrol studies) were excluded. The patients in this study also had to be clinically stable, and patients with severe cardiovascular diseases or hepato-renal diseases were excluded.21
Interventions and Comparators
In the systematic review and meta-analysis of allergic reactions, the GBCAs used in the included studies were: gadodiamide, gadopentetate, gadobutrol, gadoxetate, gadoterate, gadobenate, gadoteridol, and gadofosveset. The GBCAs were grouped as linear or macrocylic, as well as by ionicity for analysis.16
The systematic review of GBCA depositions in the brain included patients who had undergone GBCA-enhanced MRI. As noted in the systematic review, the contrast agents of the included publications were: gadopentetate dimeglumine, linear GBCA, gabobutrol, gadodiamide (Omniscan), gadoteridol, gadodiamide, gadoterate meglumine, gadobenate dimeglumine.17
In the RCT that utilized a crossover study design, patients were randomized 1:1 to receive either gadobutrol followed by gadoteridol, or gadoteridol followed by gadobutrol. The agents were administered on separate days, with a mean of 4.6 days between injections. After patients had crossed over to their respective second contrast agent (Period 2), patients were monitored for at least 72 hours for adverse events.6 Both agents were administered as a single intravenous injection at the standard dose of 0.1 mmol/kg body weight and at a rate of 2 mL/s. All injections were followed by a 20 mL 0.9% saline flush at the same rate.
One of the Japanese RCTs randomized patients 1:1 to either gadobutrol or gadopentetate dimeglumine. The patients received one intravenous standard dose of 0.1 mmol/kg body weight of their assigned contrast agent by bolus administration, using a power injector via a peripheral vein. To ensure that the injection duration was comparable, gadobutrol was administered at a rate of 1.5 to 2 mL/s and gadopentetate dimeglumine was administered at a rate of 2 to 3 mL/s. Administrations were followed by a 10 mL 0.9% saline flush at the same rate as the contrast agent.4
Similarly, the Chinese RCT randomized patients 1:1 to receive either gadobutrol or gadopentetate dimeglumine at a dose of 0.1 mmol/kg body weight. Gadobutrol was administered as a single intravenous bolus injection at a rate of 1.0 mL/s using a power injector and followed by a 20 mL saline flush. Gadopentetate was administered in the same fashion, but at a rate of 2.0 mL/s.18
The second, single-center Japanese RCT compared patients who were randomly assigned to receive gadodiamide or gadopentetate dimeglumine, each at 0.1 mmol/kg. Details on the method of injection were not given.7
The single-center RCT conducted in the USA noted that patients were randomized to receive gadobutrol or gadobenate dimeglumine. Similar to the other RCTs, the contrast agents were administered as a bolus via power injector at a rate of 2 mL/s, followed by a 20 mL saline flush. However, while gadobutrol was administered at 0.1 mmol/kg, a half-dose of gadobenate dimeglumine was used (i.e. 0.05 mmol/kg). The authors stated that this dosage was routinely used at the institution in an effort to reduce the risk of nephrogenic systemic fibrosis and produced the same diagnostic imaging quality as a full dose.20
The RCT conducted in Switzerland randomized patients to receive 0.025 mmol/kg body weight of gadoxetate disodium, or 0.05 mmol/kg body weight of gadobenate dimeglumine. Both contrast agents were administered as single intravenous injections at 2 mL/s, followed by a 20 mL 0.9% saline flush.19
Both non-randomized clinical trials administered first an unenhanced MRI, then a gadobutrol-enhanced MRI to each patient. The study investigators in each study administered 0.1 mmol/kg body weight of gadobutrol as a single intravenous injection at 2 mL/s, followed by a 20 mL 0.9% saline flush.5,21
Outcomes
The systematic review and meta-analysis examined immediate allergic reactions to GBCAs, which were defined using the American College of Radiology Classification system, whereby acute reactions are classified as mild, moderate or severe.16 The systematic review of GBCA depositions in the brain examined the signal intensity within the dentate nucleus and globus pallidus on MR images in patients who had undergone MRI with GBCA, as well as short- and long-term consequences of gadolinium use; however, the authors did not report how these were outcomes measured or extracted.17
The included RCTs examined a variety of outcomes. The crossover trial examined the occurrence of adverse events.6 Whereas, the Japanese RCT monitored the occurrence of adverse events, as well as clinical laboratory parameters, vital signs and physical examinations at specified time points post-administration.4 In addition, Liang et al. conducted a safety analysis as part of the RCT, which consisted of reporting adverse events and their associated intensity, as well as adverse events related to the contrast agent administered.18 The second Japanese RCT examined only safety outcomes, including the effects of contrast agents on renal function, such as serum-creatinine, serum cystatin-C, estimated glomerular filtration rate (eGFR) and creatinine clearance rate (CCr) levels, to examine subgroups with chronic kidney disease (CKD) and the development of contrast-induced nephropathy (CIN).7 The single-center RCT from the USA reported the occurrence and severity of visually apparent adverse events, specifically emesis and hives.20 The final RCT by Zech et al., evaluated adverse events using the patient response to the question “How do you feel?”, where responses were determined by the investigators to be related or unrelated to the contrast agent administered.19
In the non-randomized trials clinical laboratory parameters, vital signs and results of physical examinations were compared at baseline and during the 72-hour follow-up periods of each trial.5,21
Summary of Critical Appraisal
Systematic Reviews
The two systematic reviews were critically appraised using AMSTAR-II.12 The following is a summary highlighting the strengths and limitations of each study; additional details are provided in Appendix 3.
Strengths of the systematic review and meta-analysis included: data extraction completed in duplicate, author assessment of the risk of bias of the included studies using A Cochrane Risk of Bias Assessment Tool for Non-Randomized Studies of Interventions (ACROBATNRSI) and discussion of the impacts of the risk of bias on the results of each study in the review, such as sources of funding. The authors detail the heterogeneity of the included studies in the review and utilized appropriate statistics in their analysis. Finally, the authors reported any potential sources of conflict. The limitations of the systematic review included a poorly defined research question and inclusion criteria, and it was unclear to what extent a protocol was developed prior to the completion of the review. Likewise, the details of the search strategy were limited and were executed only in PubMed and Google Scholar. The authors do not explicitly state whether study selection was completed in duplicate and the included studies were not described in detail.16
Strengths of the systematic review of GBCA depositions in the brain included the following: the research question, inclusion criteria and key search terms were presented in the article; the search strategy was executed in PubMed and Medline databases; the authors hand searched the bibliographies of included studies; and study selection (title/abstract and full text screening) was reported to be conducted in duplicate, with a third reviewer consulted as necessary to resolve disputes. The limitations of the review included: limited details on the process for conducting the literature search, including the extent to which the review methods were established prior to the completion of the review (e.g. a protocol); the selection criteria for study designs; the process for data extraction; and details of the included or excluded studies. Finally, the authors did not complete any risk of bias assessment and did not report sources of funding for the included studies.17
Randomized Studies
The six included RCTs were critically appraised utilizing the CASP checklist for RCTs. The following is a summary that highlights the strengths and limitations from each study. Additional details regarding the strengths and limitations of included publications are provided in Appendix 3.
The strengths of the RCT with a crossover design included the following: patients were randomly assigned to the treatment groups, a double-blind study design was utilized, all patients were properly accounted for at the trial’s conclusion, the study had sufficiently large sample size and power and both groups had similar characteristics at baseline and were treated equally for the duration of the trial. One limitation of the study was the variable precision (i.e. the size of the standard deviations varied by outcome). The study was double-blinded, however, due to the nature of the crossover study design, the initial injection was administered by an unblinded nurse or technologist to ensure the fully blinded administration of the second injection. Although this was a large multicenter study, with many countries represented, patients with underlying conditions were excluded from the study population. Hence, the generalizability of these results may be limited.6
Kuwatsuru et al.4 conducted an RCT with strengths that are comparable to the cross-over RCT6, in that the patients were randomly assigned to treatment groups, all patients were properly accounted for at the trial’s conclusion, both groups had similar characteristics at the beginning of the trial and were treated equally for the duration of the trial. The study had sufficiently large sample size and power, as demonstrated by a power calculation. In addition, the patients were blinded to which treatment they received, however the investigators were not blinded. The limitations of this RCT4 were also similar to the crossover RCT6, including: variable precision estimates (i.e. the size of the standard deviations varied by outcome); all patients were of Asian descent, which may limit the generalizability to more diverse populations; and patients were clinically stable, limiting the generalizability of the results to real-world populations.
The strengths of Liang et al.18 RCT include the random assignment of patients to the treatment groups, all patients were properly accounted for at the trial’s conclusion, and both groups had similar characteristics at the beginning of the trial. Similar to the Kuwatsuru et al.4 RCT, the trial had a single-blind design, where investigators were not blinded to the treatment groups; however since the two contrast agents had different molarity (gadobutrol was 1.0 M and gadopentetate was 0.5 M) and were administered at different rates, the investigators could not be blinded. Limitations of this study include small treatment effects with large standard deviations, and the study included only Chinese patients.18
Naito et al.7 performed a single-center RCT. The strengths of the study include the random assignment of patients to the treatment groups and the proper accounting for all patients at the end of the trial. Additionally, both treatment groups had similar characteristics at the beginning of the trial and were treated equally for the duration of the trial. Limitations included a lack of details on blinding procedures and generalizability due to the study being conducted at a single center in Japan.
Strengths of Semelka et al.20 include the randomization of treatment assignment, blinding of patients and study personnel to treatment, and the similarity of groups at the start of the trial. The main limitation of the study was the lack of quantitative evidence provided, thus the quality of the results could not be evaluated. Additionally, Semelka et al. did not define the patient population well, and a mixed population of children and adults (ages 5 – 85) was included. This limits the generalizability to the population of interest (i.e. adults undergoing MRI). Adverse event outcomes of interest were limited to those that were visually apparent, specifically emesis and hives. Finally, gadobenate dimeglumine was administered at halfdose as per hospital protocol (gadobutrol was administered at full dose), thus the groups were not treated equally in the trial.
The strengths of the multicenter RCT performed by Zech et al.19 include randomization of patients to the treatment groups, and the double-blinded study design (though the paper does not explicitly state that the investigators were blinded). The treatment groups were not similar at the start of the trial, as more patients assigned to receive gadoxetate disodium had signs of diffuse liver disease or liver cancer. Additionally, the treatment groups received different concentrations of contrast agents (0.025 mmol/kg of gadoxetate disodium, and 0.05 mmol/kg of gadobenate dimeglumine), which may have compromised blinding and resulted in unequal treatment of the groups. Adverse events were addressed by the study investigators as an open question: “How do you feel?”, thus measurement of the safety outcome was subjective. Finally, the study population was comprised of 95% Caucasians, limiting the generalizability to more heterogeneous populations.
Non-Randomized Studies
The two included non-randomized clinical trials were critically appraised utilizing the Cochrane ROBINS-I tool.14 The following summary highlights the strengths and limitations from each study, with additional details provided in Appendix 3.
Overall, Gutierrez et al.5 and Tanaka et al.21 were similar in study design and analysis, and both were found to be comparable to a well-performed randomized trial: no bias due to confounding was expected, all eligible patients were included, the follow-up and start of intervention coincided for all patients, the intervention was well defined, and assessors were blinded and thus the outcome measures were not influenced by knowledge of the intervention. In Gutierrez et al.5, while it was reported in some cases that the intervention deviated from usual practice, these patients were excluded from analysis and thus the outcome was not affected. Tanaka et al.21 did not provide any information regarding deviations from the intended intervention.
Summary of Findings
The summary of findings below are presented according to the research questions posed by this Rapid Response report. Appendix 4 presents a table of the main study findings and authors’ conclusions.
Safety of Macrocyclic GBCAs
Gutierrez et al.6 conducted an RCT utilizing a crossover design to determine the safety profile of gadobutrol in comparison to gadoteridol, which are both macrocyclic gadoliniumbased contrast agents. The main study findings with regards to safety were that gadobutrol and gadoteridol have similar safety profiles, and a similar number of patients in the trial experienced treatment-emergent adverse events in each group (approximately 10% of patients in each group). However, less than 1% of patients experienced a serious treatment-emergent adverse event, none of which were related to gadobutrol or gadoteridol as assessed by the study investigators.6
Gutierrez et al.5 also performed a non-randomized, open-label clinical trial to determine the safety of gadobutrol. Approximately 5% of patients experienced an adverse event, and only one patient experienced a serious adverse event, which was deemed to be unrelated to gadobutrol. Gadobutrol also did not cause any clinically relevant changes to vital signs, laboratory or hematological parameters in the study population. The authors concluded that gadobutrol has a very good safety profile.5
The second non-randomized study design by Tanaka et al. also examined the safety of gadobutrol using an open-label clinical trial study design. Less than 10% of patients experienced at least one treatment-emergent adverse event, and 2.7% experienced an adverse event that was related to gadobutrol. No severe adverse events were reported with the use of gadobutrol. The study authors concluded that gadobutrol is a well-tolerated contrast agent.21
Safety of Linear GBCAs
In a single-blind RCT conducted at Kitasano University Hospital in Japan, Naito et al. 7 examined the renal safety of gadodiamide and gadopentetate dimeglumine. No patients developed contrast-induced nephropathy in either group. Kidney function parameters such as serum-creatinine, eGFR and CCr did not change significantly after receiving either gadolinium-based contrast agent, but serum cystatin-C levels were significantly higher after exposure to gadodiamide. Subgroups of patients with stage 1, 2 or 3 CKD were also examined. It was found that serum cystatin-C levels in patients with stage 1 CKD, and serum creatinine levels in patients with stage 2 CKD significantly increased after exposure to gadodiamide. The authors concluded that gadopentetate dimeglumine has no nephrotoxic effects, and gadodiamide has slight (but clinically insignificant) nephrotoxic effects. Since this study was conducted at only one center, a follow-up study on a larger scale is needed to confirm these findings.7
Zech et al.19 compared the safety of gadoxetate disodium and gadobenate dimeglumine, two linear contrast agents, in a multicenter, double-blind RCT. Adverse events were reported for each contrast agent, with approximately 6% of patients in both groups experiencing adverse events. No serious adverse events or deaths were reported. The majority of the adverse events (which were considered not serious in nature) were determined to be either “possibly” or “probably” related to the contrast agent administration, by the study investigators. However, the authors found that both agents have a similar safety profile, and this evidence was consistent with other studies.19
Comparative Risks and Safety of Macrocyclic and Linear GBCAs
The systematic review and meta-analysis of immediate allergic reactions to GBCAs found that the rate of overall and severe allergic-like reactions was 9.2 and 0.52 per 10000 administrations, respectively. The authors reported that the nonionic linear GBCA gadodiamide had the lowest overall rate of immediate adverse reactions compared to linear ionic GBCAs and nonionic macrocylic GBCAs. Nonionic linear GBCA was reported to have the lowest rate of moderate and severe adverse reactions compared to linear ionic GBCAs. The authors also reported that linear agents without protein binding had a lower reaction rate per 10000 injections when compared to macrocyclics without protein binding. In a model controlling for both ionicity and protein binding, the authors reported that nonionic linear GBCA had a lower relative risk for all reactions (0.12, 95% confidence interval [CI]: 0.05 to 0.31; P < .0001) as well as moderate and severe reactions (0.19, 95% CI: 0.05 to 0.66; P = .009) when compared with macrocyclic GBCAs. Finally, the authors reported that all GBCAs with protein binding, which included the linear GBCAs gadoxetate, gadofosveset, and gadobenate, were associated with a greater risk of reactions compared to gadopentetate dimeflumine, an ionic linear agent without protein binding. Based on these findings, the authors conclude that protein binding, macrocyclic structure, and ionicity were associated with a higher rate of allergic-like adverse events in patients injected with GBCAs. This meta-analysis was based on the findings of nine studies, and results may be limited by the retrospective analysis of data, selection bias and data accuracy.16
In the systematic review examining the presence of GBCA depositions in the brain and symptoms of gadolinium neurotoxicity looked at 25 publications (including 19 MRI analyses, 3 case reports and 3 autopsies) the authors conclude that signal intensity on unenhanced T1-weighted MR images (an indicator of brain accumulation) was correlated positively with exposure to GBCAs, and was found to be greater after serial administrations of linear nonionic versus cyclic contrast agents. However, limited data on the populations of the included studies was included in the systematic review and only a narrative description of study findings was provided.17
An RCT by Kuwatsuru et al.4 compared the safety of gadobutrol (a macrocyclic agent) to gadopentetate dimeglumine (a linear agent). In this trial, no significant changes were noted in vital signs, physical examinations or clinical laboratory parameters in either group, 24 hours after administration. Both agents were well-tolerated, with less than 10% of patients in both groups experiencing treatment-emergent adverse events. All adverse events reported in this study were of mild severity, and no serious adverse events or deaths were reported. In conclusion, the study found that both the macrocyclic and linear agent had good safety and tolerability.4
Liang et al.18 also compared the safety of gadobutrol to gadopentetate dimeglumine. The investigators found similar results to Kuwatsuru et al. regarding the safety profiles of both agents. Less than 5% of patients reported adverse events, and all adverse events were of mild intensity, according to the study investigators. One mild adverse event was deemed to be related to gadobutrol, and all other adverse events were unrelated to the study agents. Like Kuwatsuru et al., no significant changes were noted in vital signs, physical examinations or clinical laboratory parameters in either group.18
Finally, Semelka et al.20 compared gadobutrol to gadobenate dimeglumine, a linear contrast agent. The occurrence of mild adverse events was examined for both agents, particularly those that were visually apparent (emesis and hives). No patients included in the study experienced any adverse events, regardless of severity. The authors state that this study was a small-scale, pilot study designed to test the feasibility of addressing the safety of gadolinium-based contrast agents in a randomized fashion. Given the significant limitations of the study design, the results should be considered with caution, but are not dissimilar to other studies comparing macrocyclic and linear contrast agents.20