OVERVIEW
Introduction
Darunavir is an antiretroviral protease inhibitor that is used in the therapy and prevention of human immunodeficiency virus (HIV) infection and the acquired immunodeficiency syndrome (AIDS). Darunavir can cause transient and usually asymptomatic elevations in serum aminotransferase levels and has been linked to rare instances of clinically apparent, acute liver injury. In HBV or HCV coinfected patients, highly active antiretroviral therapy with darunavir may result of an exacerbation of the underlying chronic hepatitis B or C.
Background
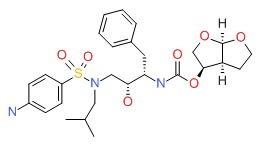
Darunavir (dar ue' na vir) is a proteinomimetic, azapeptide that blocks the catalytic site of the HIV protease preventing cleavage of viral polyprotein precursors into mature, functional proteins that are necessary for viral replication. When given in combination with other antiretroviral agents, darunavir has been shown to lower HIV RNA levels and delay onset of AIDS related complications. Darunavir was approved for use in the United States in 2003 and is indicated for the treatment of HIV, typically in combination with low “booster” doses of ritonavir, a potent CYP 3A4 inhibitor. Darunavir is available under the brand name Prezista in tablets of 75, 150, 400, 600 and 800 mg and as an oral suspension (100 mg/mL). The usual adult dosage is 800 mg with ritonavir (100 mg) once daily. Higher doses and twice daily administration are sometimes recommended for patients with darunavir resistance mutations. A fixed combination of darunavir (800 mg) with the CYP 3A4 inhibitor cobicistat (150 mg) was approved for use in HIV infection in 2016 under the brand name Prezcobix, the recommended dose being one tablet daily. Common side effects of darunavir are nausea, diarrhea, gastrointestinal upset, headache, fatigue, rash and, with long term use, hyperlipidemia and lipodystrophy. Severe adverse events can include hypersensitivity reactions including Stevens Johnson syndrome. The combination of darunavir with a CYP 3A4 inhibitor also predisposes to significant drug-drug interactions.
Hepatotoxicity
Some degree of serum aminotransferase elevations occur in a high proportion of patients taking darunavir containing antiretroviral regimens. Moderate-to-severe elevations in serum aminotransferase levels (above 5 times the upper limit of normal) are found in 3% to 10% of patients overall, and rates are higher in patients with HIV-HCV coinfection. In clinical trials of darunavir elevations in serum ALT above 5 times ULN occurred in 2% to 3% of patients, but no subject developed clinically apparent liver injury with jaundice. The serum enzyme elevations during therapy are usually asymptomatic and self-limited and can resolve even with continuation of the medication. Clinically apparent acute liver injury due to darunavir has been reported since its approval and more widescale use, but none have been well characterized for clinical features. The liver injury generally arises after 1 to 8 weeks of therapy and the pattern of serum enzyme elevations is usually, but not always, hepatocellular. Signs of hypersensitivity (fever, rash, eosinophilia) are rare, as is autoantibody formation. The acute liver injury is usually self-limited and resolves within a few weeks of stopping darunavir. However, fatal instances have been reported, at least to the sponsor and monitoring of liver enzymes during therapy is recommended.
Finally, initiation of darunavir based highly active antiretroviral therapy can lead to exacerbation of an underlying chronic hepatitis B or C in coinfected individuals, typically arising 2 to 12 months after starting therapy and associated with a hepatocellular pattern of serum enzyme elevations and increases in serum levels of hepatitis B virus (HBV) DNA or hepatitis C virus (HCV) RNA. Darunavir therapy has not been clearly linked to lactic acidosis and acute fatty liver that is reported in association with several nucleoside analogue reverse transcriptase inhibitors.
Likelihood score: D (possible, rare cause of clinically apparent liver injury).
Mechanism of Injury
The cause of the clinical hepatotoxicity from darunavir is not clearly known. Darunavir is extensively metabolized by the liver, largely by the cytochrome P450 system (CYP3A4), and toxic intermediates may be the cause of some liver injury. In patients with HIV infection who are coinfected with either HBV or HCV, initiation of potent antiretroviral therapy may be associated with flares of the underlying chronic hepatitis, which may be the result of reconstitution of the immune system, viral interactions or a direct effect of the drug on the hepatitis virus.
Outcome and Management
The severity of liver injury due to darunavir ranges from transient, asymptomatic serum aminotransferase elevations to acute hepatitis that can be severe and even fatal. In typical cases, recovery occurs within 1 to 2 months and neither chronic hepatitis nor vanishing bile duct syndrome have been reported. Rechallenge should be avoided. There does not appear to be cross sensitivity in the hepatic injury to other protease inhibitors or antiretroviral agents. The exacerbation of hepatitis B or C that can occur with darunavir based antiretroviral therapies can be severe and can lead to liver failure or progressive end stage liver disease. Patients with HCV or HBV coinfection should be monitored prospectively for viral and serum aminotransferase levels and appropriate therapy of the hepatitis instituted if possible.
References to darunavir are included with references to all the HIV protease inhibitors in the overview section of protease inhibitors (updated September 2017). Most of the HIV protease inhibitors in clinical use are proteinomimetic drugs and are structurally unrelated.
Drug Class: Antiviral Agents, Antiretroviral Agents
Other Drugs in the Subclass, Protease Inhibitors: Amprenavir, Atazanavir, Fosamprenavir, Indinavir, Lopinavir, Nelfinavir, Ritonavir, Saquinavir, Tipranavir