OVERVIEW
Introduction
Atazanavir is an antiretroviral protease inhibitor that is used in the therapy and prevention of human immunodeficiency virus (HIV-1) infection and the acquired immunodeficiency syndrome (AIDS). Atazanavir can cause transient and usually asymptomatic elevations in serum aminotransferase levels, mild elevations in indirect bilirubin concentration and, rarely, clinically apparent, acute liver injury. In HBV or HCV coinfected patients, highly active antiretroviral therapy with atazanavir may result of an exacerbation of the underlying chronic hepatitis B or C.
Background
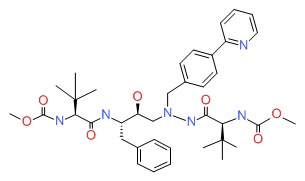
Atazanavir (a" ta zan' a vir) is proteinomimetic, azapeptide that binds to the active, catalytic site of the HIV-1 protease preventing cleavage and processing of viral polyprotein precursors into mature, functional proteins that are necessary for viral replication. Atazanavir, in combination with other antiretroviral agents, has been shown to be effective in lowering HIV RNA levels and improving CD4+ lymphocyte counts in patients with HIV infection and AIDS. Atazanavir was approved for use in the United States in 2003 for the treatment of HIV infection and is typically given in combination with low “booster” doses of ritonavir or with the pharmacologic enhancer cobicistat, which improve its pharmacokinetics by inhibiting its metabolism by CYP 3A4. Atazanavir is available under the brand name Reyataz in capsules of 150, 200 and 300 mg. The recommended adult dosage is 400 mg once daily or 300 mg if given with ritonavir (100 mg) once daily. A fixed combination of atazanavir with the cobicistat (300 mg/150 mg) is also available under the brand name Evotaz. The recommended dose of the combination formulation is one tablet daily. The most common side effects of atazanavir are nausea, diarrhea, gastrointestinal upset, headache, fatigue, rash, hypersensitivity reactions, hyperbilirubinemia and, with long term use, hyperlipidemia and lipodystrophy.
Hepatotoxicity
Atazanavir can cause several forms of liver injury including transient serum enzyme elevations, indirect hyperbilirubinemia, idiosyncratic acute liver injury and exacerbation of underlying chronic viral hepatitis.
Some degree of serum aminotransferase elevations occurs in a high proportion of patients taking atazanavir containing antiretroviral regimens. Moderate-to severe elevations in serum aminotransferase levels (>5 times the upper limit of normal) are found in 3% to 10% of patients, although rates may be higher in patients with HIV-HCV coinfection. These elevations are usually asymptomatic and self-limited and can resolve even with continuation of the medication.
Atazanavir therapy (similar to indinavir) also causes increases in unconjugated (indirect) and total serum bilirubin that can manifest as jaundice in up to 10% of patients. These elevations are due to the inhibition of UDP glucuronyl transferase, the hepatic enzyme responsible for conjugation of bilirubin that is deficient in Gilbert syndrome. The hyperbilirubinemia is usually mild, the increases averaging 0.3-0.5 mg/dL, but can be more marked in patients with Gilbert syndrome with increases of 1.5 mg/dL or more and clinical jaundice. The jaundice, however, is not indicative of hepatic injury.
Clinically apparent acute liver injury due to atazanavir is rare and the clinical pattern of liver injury, latency and recovery have not been well defined. The liver injury is idiosyncratic and rare and probably similar to the injury that is caused by other HIV protease inhibitors. The liver injury typically arises 1 to 8 weeks after starting the protease inhibitor and has variable patterns of liver enzyme elevation, from hepatocellular to cholestatic. Signs of hypersensitivity (fever, rash, eosinophilia) are rare, as is autoantibody formation. The acute liver injury is usually self-limited and resolves within a few weeks of stopping the antiretroviral agent (Case 1).
In addition, initiation of atazanavir based antiretroviral therapy can lead to exacerbation of an underlying chronic hepatitis B or C in coinfected individuals, typically arising 2 to 12 months after starting therapy, and associated with a hepatocellular pattern of serum enzyme elevations and increases in serum levels of hepatitis B virus (HBV) DNA or hepatitis C virus (HCV) RNA. Atazanavir therapy has not been clearly linked to lactic acidosis and acute fatty liver that is reported in association with several nucleoside analogue reverse transcriptase inhibitors.
Likelihood score: D (possible, rare cause of clinically apparent liver injury).
Mechanism of Injury
The cause of the clinical hepatotoxicity from atazanavir is only partially known. The indirect hyperbilirubinemia associated with its use is caused by inhibition of hepatic conjugation of bilirubin, similar to what occurs in Gilbert syndrome and is not indicative of liver injury. Atazanavir is extensively metabolized by the liver, largely by the cytochrome P450 system (CYP 3A4) and toxic intermediates may be the cause of the idiosyncratic forms of liver injury. In patients with HIV infection who are coinfected with either HBV or HCV, initiation of potent antiretroviral therapy may be associated with flares of the underlying chronic hepatitis as the result of reconstitution of the immune system, viral interactions or a direct effect of the drug on the hepatitis virus.
Outcome and Management
The severity of liver injury from atazanavir ranges from asymptomatic unconjugated hyperbilirubinemia to moderate serum aminotransferase elevations to acute hepatitis. In typical cases, recovery occurs within 1 to 2 months and neither chronic hepatitis nor vanishing bile duct syndrome have been reported due to atazanavir. Rechallenge may lead to recurrence and should be avoided. There does not appear to be cross sensitivity in the hepatic injury to other protease inhibitors or antiretroviral agents. The exacerbation of hepatitis B or C that can occur with atazanavir based antiretroviral therapies can be severe and lead to liver failure or progressive, end stage liver disease. Patients with HCV or HBV coinfection should be monitored prospectively for viral and serum aminotransferase levels and appropriate therapy instituted if possible.
References to atazanavir are included with references to all the HIV protease inhibitors in the overview section of Protease Inhibitors (updated September 2017). Most of the HIV protease inhibitors in clinical use are proteinomimetic drugs and are structurally unrelated.
Drug Class: Antiviral Agents, Antiretroviral Agents
Other Drugs in the Subclass, Protease Inhibitors: Amprenavir, Darunavir, Fosamprenavir, Indinavir, Lopinavir, Nelfinavir, Ritonavir, Saquinavir, Tipranavir
CASE REPORT
Case 1. Serum aminotransferase elevations and jaundice arising during atazanavir therapy.
[Modified from: Eholié SP, Lacombe K, Serfaty L, Wendum D, Girard PM. Acute hepatic cytolysis in an HIV-infected patient taking atazanavir. AIDS 2004; 18: 1610-1. PubMed Citation]
A 56 year old woman with HIV infection and long history of antiretroviral therapy developed elevations in serum aminotransferase levels 8 weeks after switching from lopinavir/ritonavir to atazanavir in combination with tenofovir and didanosine. In the previous five years, she had been treated with various antiretroviral regimens which had included stavudine, didanosine, efavirenz, abacavir, nelfinavir, lopinavir and ritonavir, and had complications of lipodystrophy and dyslipidemia. Tests for hepatitis A, B and C were negative as were autoantibodies. She did not drink alcohol and was taking no other medications. Because of improvements in her dyslipidemia after switching to atazanavir, the medication was continued and she was monitored. Thirty weeks after starting atazanavir, serum ALT levels had risen to more than ten-fold elevated and she was jaundiced (Table). Ultrasonography showed fatty liver without evidence of obstruction and liver biopsy showed steatosis and an acute hepatitis-like picture. Antiretroviral treatment was discontinued and serum aminotransferase levels fell to near normal levels within the next 2 months. She tolerated reintroduction of antiretroviral therapy with tenofovir, didanosine and nelfinavir without recurrence of ALT elevations.
Key Points
View in own window
| Medication: | Atazanavir |
|---|
| Pattern: | Hepatocellular (R=8.3) |
|---|
| Severity: | 3+ (jaundice, hospitalization) |
|---|
| Latency: | 8 weeks to onset of ALT elevations, 30 weeks to jaundice |
|---|
| Recovery: | Yes |
|---|
| Other medications: | Tenofovir, didanosine |
|---|
Laboratory Values
View in own window
| Time After Starting | Time After Stopping | ALT* (U/L) | Alk P (U/L) | Bilirubin (mg/dL) | Other |
|---|
| Pre | | 27 | Normal | Normal | |
| Pre | | 25 | | | |
| Atazanavir started and lopinavir stopped because of dyslipidemia |
| 7 weeks | | 105 | | | |
| 4 months | | 90 | | | |
| 7 months | | 265 | | | |
| 7.5 months | 0 | 405 | 158 | 4.6 | Therapy stopped |
| 8 months | 1 week | 290 | | | |
| 9 months | 6 weeks | 240 | | | |
| 8 weeks | 110 | | | Tenofovir restarted |
| 10 months | 3 months | 48 | | | |
| 11 months | 4 months | 30 | | | |
|
Normal Values
|
<40
|
<130
|
<1.2
| |
*Values estimated from Figure 1.