NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
LiverTox: Clinical and Research Information on Drug-Induced Liver Injury [Internet]. Bethesda (MD): National Institute of Diabetes and Digestive and Kidney Diseases; 2012-.

LiverTox: Clinical and Research Information on Drug-Induced Liver Injury [Internet].
Show detailsOVERVIEW
Introduction
Isoflurane is a commonly used inhalational anesthetic and has an excellent safety record. Isoflurane has been linked to rare instances of severe acute liver injury resembling halothane induced liver injury in small case series and individual case reports.
Background
Isoflurane (eye" soe flur' ane) is a widely used major anesthetic agent with rapid onset of action and rapid dispersal. Isoflurane is a halogenated anesthetic, similar in structure and activity to halothane, desflurane, enflurane and sevofurane. Isoflurane is typically given in inhaled concentrations of 0.5% to 3% in oxygen. Because of its pungent odor and somewhat slow onset of action, isoflurane is typically used to maintain anesthesia after induction with other agents such as nitrous oxide, fentanyl and propofol. Isoflurane became available for use in the United States in 1979. Isoflurane must be administered in a controlled situation by a properly trained anesthesiologist or nurse anesthetist.
Hepatotoxicity
Prospective, serial blood testing often demonstrates minor transient elevations in serum aminotransferase levels in the 1 to 2 weeks after major surgery and halogenated anesthetic agents. Appearance of ALT levels above 10 times the upper limit of normal, however, is distinctly unusual and points to significant hepatotoxicity. Clinically apparent, severe hepatic injury from isoflurane is very rare, only isolated case reports and small case series having been published. The injury is marked by acute elevations in serum aminotransferase levels (5- to 50-fold) and appearance of jaundice within 2 to 21 days of surgery. There are usually minimal increases in alkaline phosphatase and gammaglutamyl transpeptidase levels. Jaundice is usually preceded by a day or two of fever and may be accompanied by rash and eosinophilia. The acute liver injury may be self-limited and resolve within 4 to 8 weeks, but can be severe and associated with acute liver failure. A strong risk factor is previous exposure to any of the halogenated anesthetics and particularly a history of halothane hepatitis or unexplained fever and rash after anesthesia with one of these agents. The differential diagnosis of acute liver injury after surgery and anesthesia is sometimes difficult, and a clinical picture similar to isoflurane hepatitis can be caused by shock or ischemia, other idiosyncratic forms of drug induced liver injury and acute viral or herpes hepatitis.
Likelihood score: B (highly likely cause of clinically apparent liver injury).
Mechanism of Injury
The mechanism of isoflurane hepatotoxicity is suspected to be similar to that of halothane and associated with creation of reactive intermediates. Isoflurane is metabolized to some extent by the microsomal drug metabolizing enzyme CYP 2E1 to a trifluoroacetylated reactive intermediate (TFA) that is capable of binding to multiple intracytoplasmic proteins forming potentially immunogenic adducts. The TFA adducts induce antibodies that can be detected in patients with isoflurane, desflurane as well as halothane hepatotoxicity and are also found in a proportion of health care workers exposed to the volatile anesthetics.
Outcome and Management
Severity ranges from mild and transient aminotransferase elevations without symptoms or other evidence of liver injury, to a self limited symptomatic acute hepatitis-like reaction to severe, acute hepatic failure. The severity and prognosis may relate in part of patient age, being more severe in the elderly and both milder and less common in children. Obesity may also be both a predisposing factor and predictor of outcome. Chronic liver injury from isoflurane exposure has not been described. Patients with isoflurane induced hepatitis should be cautioned against future exposure to fluorinated hydrocarbon anesthetics such as halothane, enflurane, desflurane or sevoflurane.
Drug Class: Halogenated Anesthetics
Other drugs in the Class: Desflurane, Enflurane, Halothane, Sevoflurane
CASE REPORT
Case 1. Isoflurane hepatotoxicity in a patient with previous history of halothane-induced hepatitis.
[Modified from: Hasan F. Isoflurane hepatotoxicity in a patient with a previous history of halothane-induced hepatitis. Hepatogastroenterology 1998; 45: 518-22. PubMed Citation]
A 35 year old woman with diabetes and a previous history of elevated ALT levels after halothane exposure underwent arthroscopy under general anesthesia with isoflurane. Her perioperative and postoperative liver profile was normal. Two weeks later, she presented with jaundice. Of interest, she had a history of halothane induced liver injury 1 and 7 years previously, both episodes associated with jaundice and marked serum aminotransferase elevations. On physical examination she was jaundiced and had mild hepatomegaly. Laboratory examination revealed total bilirubin 27.2 mg/dL, ALT 1950 U/L, alkaline phosphatase 226 U/L, albumin 3.5 g/dL, total protein 7.5 g/dL, and prothrombin time 16 sec (normal 11 sec). Complete blood counts were normal. Abdominal ultrasound showed hepatomegaly with increased echogenicity throughout the liver. The gallbladder, common bile duct, spleen and portal veins were normal. Tests for acute hepatitis A, B and C were negative as were autoantibodies. Liver biopsy showed severe, predominantly centrozonal necrosis and cell loss with diffuse inflammatory infiltrates. The patient was treated with supportive measures and the liver function tests improved spontaneously. She was discharged after 16 days of hospitalization and recovered after 12 weeks. Subsequently, she underwent abscess drainage under propofol anesthesia without incident.
Key Points
| Medication: | Isoflurane |
| Pattern: | Hepatocellular (R=25.5) |
| Severity: | 3+ (jaundice, hospitalization) |
| Latency: | 1 to 2 weeks |
| Recovery: | 3 months |
| Other medications: | Indomethacin, insulin |
Laboratory Values
* Converted from micromoles to mg/dL.
Comment
Severe isoflurane hepatotoxicity is rare. Most commonly the injury presents with fever and jaundice 3 to 14 days after surgery. Many affected patients have a history of previous halothane or isoflurane exposure. Female gender, as in this patient, is a risk factor. The latency period of halothane anesthetic induced liver dysfunction decreases with the frequency of exposure. Rash occurs in 10% of patients. This is a diagnosis of exclusion, and the most common causes of jaundice postoperatively that require exclusion are sepsis, biliary disease, parenteral nutrition related jaundice and shock or ischemia. Recovery is expected after 3 to 4 months. Rechallenge should be avoided, using total intravenous anesthetic technique whenever possible, which this patient later underwent without difficulty.
PRODUCT INFORMATION
REPRESENTATIVE TRADE NAMES
Isoflurane – Generic, Forane®
DRUG CLASS
Anesthetics, Halogenated
Product labeling at DailyMed, National Library of Medicine, NIH
CHEMICAL FORMULA AND STRUCTURE
| DRUG | CAS REGISTRY NO | MOLECULAR FORMULA | STRUCTURE |
|---|---|---|---|
| Isoflurane | 26675-46-7 | C3-H2-Cl-F5-O |
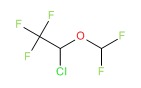 |
ANNOTATED BIBLIOGRAPHY
References updated: 01 January 2018
- Zimmerman HJ. Anesthetic agents. In, Zimmerman, HJ. Hepatotoxicity: the adverse effects of drugs and other chemicals on the liver. 2nd ed. Philadelphia: Lippincott, 1999: pp. 457-82.(Expert review of hepatotoxicity of anesthetic agents published in 1999; mentions that the newer halogenated anesthetics appear to be safer than halothane, but that hints of liver injury from desflurane and sevoflurane have appeared).
- Kenna JG. Mechanism, pathology, and clinical presentation of hepatoxicity of anesthetic agents. In, Kaplowitz N, DeLeve LD, eds. Drug-induced liver disease. 3rd ed. Amsterdam: Elsevier, 2013: pp 403-22.(Review of liver injury from anesthetic agents published in 2013; mentions that a few cases of postoperative liver injury have occurred in patients exposed to isoflurane).
- Patel PM, Patel HH, Roth DM. General anesthetics and therapeutic gases. In, Brunton LL, Chabner KA, Knollman KC, eds. Goodman & Gilman's the pharmacological basis of therapeutics. 12th ed. New York: McGraw-Hill, 2011, pp. 527-64.(Textbook of pharmacology and therapeutics; isoflurane is a commonly used inhalation anesthetic; 99% is excreted unchanged by the lungs and only 0.2% is metabolized by CYP 2E1).
- McLaughlin DF, Eger EI 2nd. Repeated isoflurane anesthesia in a patient with hepatic dysfunction. Anesth Analg 1984; 63: 775-8. [PubMed: 6465564](65 year old woman was found to have liver test abnormalities 11 days after surgery and isoflurane anesthesia [bilirubin 0.4 mg/dL, ALT 229 U/L, Alk P 900 U/L] which was initially attributed isoflurane, but later shown to be due to biliary obstruction).
- Lambert DH. Isoflurane and hepatic dysfunction. Anesth Analg 1985; 64: 458-60. [PubMed: 2858992](Letter in response to McLaughlin et al [1984] questioning their interpretation).
- Fisher NA, Iwata RT, Eger EI 2nd, Smuckler EA. Hepatic necrosis associated with herpes virus after isoflurane anesthesia. Anesth Analg 1985; 64: 1131-3. [PubMed: 2996384](62 year old man developed fever 4 days after surgery and isoflurane anesthesia followed by diarrhea on day 9 with progressive illness leading to death by day 14 accompanied by mild liver test abnormalities [bilirubin 0.8 rising to 1.2 mg/dL, ALT 21 rising to 207 U/L], with evidence of herpes viruses found in liver on autopsy).
- Grégoire S, Smiley RK. Acute hepatitis in a patient with mild factor IX deficiency after anesthesia with isoflurane. CMAJ 1986; 135: 645-6. [PMC free article: PMC1491315] [PubMed: 3756695](33 year old man developed fatigue, fever and jaundice 6 to 8 days after surgery and isoflurane anesthesia [bilirubin ~4 mg/dL, ALT 2500 U/L, Alk P 190 U/L] with recovery in two months; also received Factor IX IV, raising possibility of short incubation period “non-A, non-B hepatitis”).
- Webster JA. Acute hepatitis after isoflurane anesthesia. CMAJ 1986; 135: 1343-4. [PMC free article: PMC1491683] [PubMed: 3779567](Letter in response to Grégoire [1986] contesting conclusions).
- Carrigan TW, Straughen WJ. A report of hepatic necrosis and death following isoflurane anesthesia. Anesthesiology 1987; 67: 581-3. [PubMed: 3662087](44 year old woman developed acute liver injury starting 2 days after surgery and isoflurane anesthesia [bilirubin 9.6 mg/dL, AST >2000 U/L, LDH >4000 U/L], progressing to death by day 4; no rash, fever or eosinophilia and liver injury possibly due to ischemia).
- Stoelting RK, Blitt CD, Cohen PJ, Merin RG. Hepatic dysfunction after isoflurane anesthesia. Anesth Analg 1987; 66: 147-53. [PubMed: 3813057](Review of 45 FDA cases of suspected isoflurane hepatotoxicity by 4 expert anesthesiologists, only 36% of cases were considered as “might be” related).
- Brunt EM, White H, Marsh JW, Holtmann B, Peters MG. Fulminant hepatic failure after repeated exposure to isoflurane anesthesia: a case report. Hepatology 1991; 13: 1017-21. [PubMed: 2050317](26 year old obese woman with history of multiple surgeries and exposures to halogenated anesthetics developed nausea 11 days after isoflurane anesthesia [bilirubin 22 mg/dL, ALT 948 U/L, Alk P 270 U/L], ultimately requiring liver transplant).
- Zimmerman HJ. Even isoflurane. Hepatology 1991; 13: 1251. [PubMed: 2050339](Editorial in response to Brunt [1991] providing overview of anesthetic induced liver injury and suggesting that isoflurane be added to the list of agents causing it).
- Gunza JT, Pashayan AG. Postoperative elevation of serum transaminases following isoflurane anesthesia. J Clin Anesth 1992; 4: 336-41. [PubMed: 1419017](42 year old woman developed asymptomatic and immediate ALT elevation [774 U/L on day 1] without jaundice after isoflurane anesthesia, with fall to normal in 2 weeks, a pattern more typical of ischemic injury).
- Kharasch ED, Thummel KE. Identification of cytochrome P450 2E1 as the predominant enzyme catalyzing human liver microsomal defluorination of sevoflurane, isoflurane, and methoxyflurane. Anesthesiology 1993; 79: 795-807. [PubMed: 8214760](Human microsomes were used to assess metabolism of sevoflurane: CYP 2E1 was the major if not sole enzyme catalyzing defluorination of sevoflurane and others).
- Scheider DM, Klygis LM, Tsang TK, Caughron MC. Hepatic dysfunction after repeated isoflurane administration. J Clin Gastroenterol 1993; 17: 168-70. [PubMed: 8409323](45 year old woman developed ALT elevations starting 3 days after isoflurane anesthesia [peak bilirubin 2.5 mg/dL, ALT 320 U/L, Alk P 900 U/L], with recurrence on reexposure to isoflurane [bilirubin 0.5 mg/dL, ALT 90 U/L, Alk P 400 U/L], resolving rapidly).
- Slayter KL, Sketris IS, Gulanikar A. Halothane hepatitis in a renal transplant patient previously exposed to isoflurane. Ann Pharmacother 1993; 27: 101. [PubMed: 8431608](37 year old man with 2 previous exposures to isoflurane developed serum enzyme elevations starting 7 days after halothane anesthesia [peak bilirubin 1.3 mg/dL, ALT 926 U/L, Alk P 472 U/L], resolving within 2 months).
- Gunaratnam NT, Benson J, Gandolfi AJ, Chen M. Suspected isoflurane hepatitis in an obese patient with a history of halothane hepatitis. Anesthesiology 1995; 83: 1361-4. [PubMed: 8533932](47 year old severely obese man with a history of halothane hepatitis developed fever 1 day and jaundice 10 days after surgery under isoflurane anesthesia [bilirubin 1.4 rising to 5.5 mg/dL, ALT 1576 U/L, 4% eosinophils], resolving within 40 days; also had anti-TFA-protein antibodies during the acute episode).
- Gelven PL, Cina SJ, Lee JD, Nichols CA. Massive hepatic necrosis and death following repeated isoflurane exposure: case report and review of the literature. Am J Forensic Med Pathol 1996; 17: 61-4. [PubMed: 8838473](30 year old woman had outpatient surgery under isoflurane anesthesia and died unexpectedly 2 days later, autopsy showed fat, inflammation and massive necrosis; role for isoflurane difficult to assess).
- Sinha A, Clatch RJ, Stuck G, Blumenthal SA, Patel SA. Isoflurane hepatotoxicity: a case report and review of the literature. Am J Gastroenterol 1996; 91: 2406-9. [PubMed: 8931426](67 year old man developed marked ALT elevations [>1000 U/L] starting 12 days after isoflurane anesthesia without symptoms, fever or jaundice and with rapid recovery; also had late appearance of anti-TFA antibodies).
- Weitz J, Kienle P, Böhrer H, Hofmann W, Theilmann L, Otto G. Fatal hepatic necrosis after isoflurane anaesthesia. Anaesthesia 1997; 52: 892-5. [PubMed: 9349074](36 year old woman developed nausea, abdominal pain and fever 2 days after surgery using isoflurane anesthesia [bilirubin 4.8 mg/dL, ALT 1000 U/L, INR 2.1], ultimately undergoing liver transplantation but dying by day 12; anti-TFA negative, massive centrolobular necrosis in explant suggestive of ischemia).
- Hasan F. Isoflurane hepatotoxicity in a patient with a previous history of halothane-induced hepatitis. Hepatogastroenterology 1998; 45: 518-22. [PubMed: 9638441](35 year old woman developed hepatitis 2 weeks after isoflurane anesthesia, having had 2 previous episodes of jaundice after halothane [peak bilirubin 27.4 mg/dL, ALT 1950 U/L, Alk P 226 U/L], resolving within 12 weeks. Case 1).
- Meldrum DJ, Griffiths R, Kenna JG. Gallstones and isoflurane hepatitis. Anaesthesia 1998; 53: 905-9. [PubMed: 9849287](65 year old woman developed abnormal enzymes 3 days after surgery and isoflurane anesthesia with cholestatic pattern [peak bilirubin 0.6 mg/dL, ALT 250 U/L, Alk P 609 U/L], gallstones and dilated bile ducts found, but patient also had anti-TFA-adducts; only possibly due to isoflurane).
- Nishiyama T, Yokoyama T, Hanaoka K. Liver function after sevoflurane or isoflurane anaesthesia in neurosurgical patients. Can J Anaesth 1998; 45: 753-6. [PubMed: 9793665](Prospective analysis of ALT, AST, Alk P and bilirubin 1,2,3,7 and 14 days after sevo- or isoflurane [n=45 each] showed minimal increases in ALT and AST peaking at 7 days; elevated in ~15%, no patient was symptomatic or jaundiced).
- Turner GB, O'Rourke D, Scott GO, Beringer TR. Fatal hepatotoxicity after re-exposure to isoflurane: a case report and review of the literature. Eur J Gastroenterol Hepatol 2000; 12: 955-9. [PubMed: 10958225](76 year old woman developed fever on day 1 and jaundice day 6 after isoflurane anesthesia, but she also had sepsis, atrial fibrillation, amiodarone and ciprofloxacin exposures; subsequently had acute liver failure and died on day 7; no anti-TFA and bland centrizonal necrosis with cholestasis and fat on autopsy).
- Martin JL, Keegan MT, Vasdev GM, Nyberg SL, Bourdi M, Pohl LR, Plevak DJ. Fatal hepatitis associated with isoflurane exposure and CYP2A6 autoantibodies. Anesthesiology 2001; 95: 551-3. [PubMed: 11506133](55 year old woman developed severe hepatitis starting 4 days after isoflurane anesthesia [bilirubin 8.0 mg/dL, ALT 6564 U/L, Alk P 691 U/L mg/dL and lactic acidosis, pH 7.09], without fever or eosinophilia; immunologic testing showed little anti-CYP 2E1, but high titers of anti-CYP 2A6 and presence of TFA-labeled microsomal proteins).
- Malnick SD, Mahlab K, Borchardt J, Sokolowski N, Attali M. Acute cholestatic hepatitis after exposure to isoflurane. Ann Pharmacother 2002; 36: 261-3. [PubMed: 11847945](70 year old woman developed jaundice and pruritus 2 weeks after isoflurane anesthesia [bilirubin 17 mg/dL, ALT 1533 U/L, Alk P 203 U/L], resolving over ensuing 4 months).
- Njoku DB, Shrestha S, Soloway R, Duray PR, Tsokos M, Abu-Asab MS, Pohl LR, West AB. Subcellular localization of trifluoroacetylated liver proteins in association with hepatitis following isoflurane. Anesthesiology 2002; 96: 757-61. [PubMed: 11873055](66 year old man developed fever and jaundice 7 days after isoflurane [repeat exposure] anesthesia [bilirubin 10.9 mg/dL, ALT 3973 U/L, PT 20.6 sec] and early coma, but eventual recovery; liver biopsy showed centrolobular necrosis, fat and cholestasis with TFA modified proteins).
- Russo MW, Galanko JA, Shrestha R, Fried MW, Watkins P. Liver transplantation for acute liver failure from drug-induced liver injury in the United States. Liver Transpl 2004; 10: 1018-23. PubMed Citation. [PubMed: 15390328](Among ~50,000 liver transplants done in the United States between 1990 and 2002, 137 [0.2%] were done for idiosyncratic drug induced acute liver failure, of which 3 were attributed to halothane and 1 to isoflurane, but none to other halogenated anesthetics).
- Björnsson E, Jerlstad P, Bergqvist A, Olsson R. Fulminant drug-induced hepatic failure leading to death or liver transplantation in Sweden. Scand J Gastroenterol 2005; 40: 1095-101. PubMed Citation. [PubMed: 16165719](36 years of reporting to Swedish registry identified 103 cases of acute liver failure due to drugs, of which 16 were attributed to halothane [ranking #1] but none to other halogenated anesthetics).
- Ihtiyar E, Algin C, Haciolu A, Isiksoy S. Fatal isoflurane hepatotoxicity without re-exposure. Indian J Gastroenterol 2006; 25: 41-2. [PubMed: 16567898](68 year old man developed immediate rise in ALT [7200 U/L], AST [20200 U/L] and LDH [20,730 U/L] on day 3 after cholecystectomy under isoflurane anesthesia, but also 2 days after episode of hypotension: died on day 6, possibly due to ischemic hepatitis).
- Chalasani N, Fontana RJ, Bonkovsky HL, Watkins PB, Davern T, Serrano J, Yang H, Rochon J; Drug Induced Liver Injury Network (DILIN). Causes, clinical features, and outcomes from a prospective study of drug-induced liver injury in the United States. Gastroenterology 2008; 135: 1924-34. [PMC free article: PMC3654244] [PubMed: 18955056](Among 300 cases of drug induced liver disease collected in the US between 2003 and 2008, 2 cases were attributed to desflurane, 1 to sevoflurane, but none to isoflurane).
- Côté G, Bouchard S. Hepatotoxicity after desflurane anesthesia in a 15 month old child with Mobius syndrome after previous exposure to isoflurane. Anesthesiology 2007; 107: 843-5. [PubMed: 18073559](15 month old boy developed ALT of 6,180 U/L and INR of 2.7 on postoperative day 3 after desflurane anesthesia [having had 2 previous exposures to isoflurane] with rapid recovery; bilirubin not mentioned and patient also received acetaminophen).
- Her C. Acetaminophen-induced, not desflurane-induced, hepatotoxicity. Anesthesiology 2008; 109: 570-1. [PubMed: 18719456](Letter in response to Côté and Bouchard suggesting that the liver injury was due to acetaminophen rather than desflurane using Rumack-Matthew nomogram and in view of the high ALT levels).
- Reuben A, Koch DG, Lee WM; Acute Liver Failure Study Group. Drug-induced acute liver failure: results of a U.S. multicenter, prospective study. Hepatology 2010; 52: 2065-76. [PMC free article: PMC3992250] [PubMed: 20949552](Among 1198 patients with acute liver failure enrolled in a US prospective study between 1998 and 2007, 133 were attributed to drug induced liver injury, of which 2 were attributed to anesthetic agents, 1 halothane and 1 isoflurane).
- Peiris LJ, Agrawal A, Morris JE, Basnyat PS. Isoflurane hepatitis-induced liver failure: a case report. J Clin Anesth 2012; 24: 477-9. [PubMed: 22658370](77 year old woman developed jaundice 2 days after a hemicolectomy for which she received isoflurane anesthesia [bilirubin 4.4 mg/dL, ALT 1063 U/L, Alk P 108 U/L], with rapid worsening and death on day 4 from multiorgan failure with massive, centrolobular coagulative necrosis on autopsy).
- Björnsson ES, Bergmann OM, Björnsson HK, Kvaran RB, Olafsson S. Incidence, presentation and outcomes in patients with drug-induced liver injury in the general population of Iceland. Gastroenterology 2013; 144: 1419-25. [PubMed: 23419359](In a population based study of drug induced liver injury from Iceland, 96 cases were identified over a 2 year period, none of which were due to anesthetic agents).
- Nishiyama T. Effects of repeat exposure to inhalation anesthetics on liver and renal function. J Anaesthesiol Clin Pharmacol 2013; 29: 83-7. [PMC free article: PMC3590549] [PubMed: 23493664](Retrospective analysis of 206 patients who underwent anaesthesia twice within a 1 year period found higher rates of ALT elevations within 16 days after isoflurane [60-83%] than sevoflurane [24-30%] or propofol-fentanyl [12-17%], most elevations being less than twice ULN and no differences between first and second exposure).
- Safari S, Motavaf M, Seyed Siamdoust SA, Alavian SM. Hepatotoxicity of halogenated inhalational anesthetics. Iran Red Crescent Med J 2014; 16: e20153. [PMC free article: PMC4270648] [PubMed: 25593732](Review of hepatotoxicity of the volatile halogenated anesthetics).
- Lin J, Moore D, Hockey B, Di Lernia R, Gorelik A, Liew D, Nicoll A. Drug-induced hepatotoxicity: incidence of abnormal liver function tests consistent with volatile anaesthetic hepatitis in trauma patients. Liver Int 2014; 34: 576-82. [PubMed: 23944929](Retrospective analysis of records from 1556 patients admitted to a trauma unit during 2008 identified 47 cases of possible volatile anesthetic related liver injury, including 12 who developed ALT levels above 200 U/L of whom 11 had fever and 6 eosinophilia, but none were jaundiced or developed acute liver failure).
- Hernández N, Bessone F, Sánchez A, di Pace M, Brahm J, Zapata R, A Chirino R, et al. Profile of idiosyncratic drug induced liver injury in Latin America. An analysis of published reports. Ann Hepatol 2014; 13: 231-9. (Systematic review of literature of drug induced liver injury in Latin American countries published from 1996 to 2012 identified 176 cases of which 5 [3%] were attributed to halothane and caused acute liver failure, while. [PubMed: 24552865]no other volatile anesthetic was listed).
- Chalasani N, Bonkovsky HL, Fontana R, Lee W, Stolz A, Talwalkar J, Reddy KR, et al.; United States Drug Induced Liver Injury Network. Features and outcomes of 899 patients with drug-induced liver injury: The DILIN Prospective Study. Gastroenterology 2015; 148: 1340-52.e7. [PMC free article: PMC4446235] [PubMed: 25754159](Among 899 cases of drug induced liver injury enrolled in a US prospective study between 2004 and 2013, 2 were attributed to isoflurane, 1 to sevoflurane, but none to halothane, enflurane or desflurane).
- PMCPubMed Central citations
- PubChem SubstanceRelated PubChem Substances
- PubMedLinks to PubMed
- Review Halogenated Anesthetics.[LiverTox: Clinical and Researc...]Review Halogenated Anesthetics.. LiverTox: Clinical and Research Information on Drug-Induced Liver Injury. 2012
- Biotransformation of halothane, enflurane, isoflurane, and desflurane to trifluoroacetylated liver proteins: association between protein acylation and hepatic injury.[Anesth Analg. 1997]Biotransformation of halothane, enflurane, isoflurane, and desflurane to trifluoroacetylated liver proteins: association between protein acylation and hepatic injury.Njoku D, Laster MJ, Gong DH, Eger EI 2nd, Reed GF, Martin JL. Anesth Analg. 1997 Jan; 84(1):173-8.
- Halothane and isoflurane inhibit endothelium-derived relaxing factor-dependent cyclic guanosine monophosphate accumulation in endothelial cell-vascular smooth muscle co-cultures independent of an effect on guanylyl cyclase activation.[Anesthesiology. 1995]Halothane and isoflurane inhibit endothelium-derived relaxing factor-dependent cyclic guanosine monophosphate accumulation in endothelial cell-vascular smooth muscle co-cultures independent of an effect on guanylyl cyclase activation.Johns RA, Tichotsky A, Muro M, Spaeth JP, Le Cras TD, Rengasamy A. Anesthesiology. 1995 Oct; 83(4):823-34.
- Review Anesthetics, General.[LiverTox: Clinical and Researc...]Review Anesthetics, General.. LiverTox: Clinical and Research Information on Drug-Induced Liver Injury. 2012
- Urinary neopterin and kynurenine in patients submitted to surgical stress with different inhalational anesthetics (halothane or isoflurane).[Int J Immunopharmacol. 1999]Urinary neopterin and kynurenine in patients submitted to surgical stress with different inhalational anesthetics (halothane or isoflurane).Marfella A, Bilancio A, Polese C, Iodice F, Edmondo C, Cerasuolo D, Esposito G, Zannoni V, Beneduce G. Int J Immunopharmacol. 1999 Jul; 21(7):423-33.
- Isoflurane - LiverToxIsoflurane - LiverTox
Your browsing activity is empty.
Activity recording is turned off.
See more...