NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
LiverTox: Clinical and Research Information on Drug-Induced Liver Injury [Internet]. Bethesda (MD): National Institute of Diabetes and Digestive and Kidney Diseases; 2012-.

LiverTox: Clinical and Research Information on Drug-Induced Liver Injury [Internet].
Show detailsOVERVIEW
Introduction
Thioridazine is a phenothiazine and antipsychotic agent that is no longer in common use. Thioridazine has been linked to rare instances of clinically apparent acute cholestatic liver injury.
Background
Thioridazine is a piperazine phenothiazine derivative which acts by postsynaptic inhibition of dopamine receptors. Thioridazine has other peripheral and central nervous system effects, producing both alpha adrenergic stimulation and blocking histamine- and serotonin-mediated effects. Thioridazine is indicated for the therapy of acute and chronic psychosis. Thioridazine was approved for use in the United States in 1978 and was formerly a commonly prescribed antipsychotic medication, but in recent years has been replaced in large part by the atypical antipsychotics, which have fewer extrapyramidal side effects. Use of thioridazine is also restricted because of its propensity to cause prolongation of the QTc interval and increased risk of sudden death. Thioridazine is available as tablets of 10, 25, 50 and 100 mg in generic forms and previously under the brand name Mellaril. The usual recommended dose in adults is 50 to 100 mg three times daily, increasing based upon effect and tolerance to a maximum of 800 mg daily. Common side effects include drowsiness, dizziness, headache, blurred vision, dry mouth, constipation, tremor, restlessness, muscle spasms and weight gain. Uncommon but potentially severe adverse events include increased mortality in elderly patients with dementia-associated psychosis, neuroleptic malignant syndrome, tardive dyskinesia, hypotension and falls.
Hepatotoxicity
Liver test abnormalities have been reported to occur in a high proportion of patients on long term phenothiazine therapy, but elevations are uncommonly above 3 times the upper limit of normal. The aminotransferase abnormalities are usually mild, asymptomatic and transient, reversing even with continuation of medication. Rare instances of clinically apparent acute liver injury have been reported due to thioridazine, with some resemblance to cases of chlorpromazine jaundice. The onset of jaundice occurred within a few weeks to several months of therapy and the pattern of serum enzyme elevations was typically cholestatic, although hepatocellular patterns have also been reported. Immunoallergic manifestations (fever, rash and eosinophilia) were not prominent and autoantibodies were not detected. Some cases were associated with agranulocytosis which is a rare but known complication of the phenothiazines.
Likelihood score: B (likely but rare cause of clinically apparent liver injury).
Mechanism of Injury
The mechanism by which the phenothiazines cause serum aminotransferase elevations is not known. Thioridazine is extensively metabolized by the liver via sulfoxidation and oxidation, and some instances of serum aminotransferase elevations as well as more clinical apparent liver injury may be caused by production of a toxic intermediate of its metabolism.
Outcome and Management
The serum aminotransferase elevations that occur on thioridazine therapy are usually self-limited and do not require dose modification or discontinuation of therapy. The acute clinically apparent liver injury caused by thioridazine is typically self-limited and benign. Instances of chronic cholestasis and vanishing bile duct syndrome have not been reported with thioridazine, but many cases have been attributed to other phenothiazines. Rechallenge with thioridazine usually causes a prompt recurrence of the liver injury and should be avoided. Patients with thioridazine induced liver injury may have cross sensitivity to other phenothiazines, but generally tolerate the atypical antipsychotics.
Drug Class: Antipsychotic Agents
Other Drugs in the Subclass, Phenothiazines: Chlorpromazine, Fluphenazine, Perphenazine, Prochlorperazine, Trifluoperazine
PRODUCT INFORMATION
REPRESENTATIVE TRADE NAMES
Thioridazine – Generic, Mellaril®
DRUG CLASS
Antipsychotic Agents
Product labeling at DailyMed, National Library of Medicine, NIH
CHEMICAL FORMULA AND STRUCTURE
| DRUG | CAS REGISTRY NUMBER | MOLECULAR FORMULA | STRUCTURE |
|---|---|---|---|
| Thioridazine | 50-52-2 | C21-H26-N2-S2 |
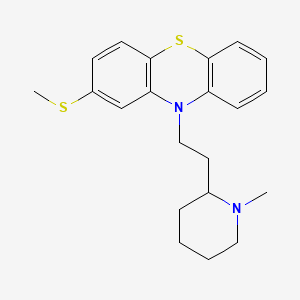
|
ANNOTATED BIBLIOGRAPHY
References updated: 01 July 2020
- Zimmerman HJ. Neuroleptic drugs. In, Zimmerman HJ. Hepatotoxicity: the adverse effects of drugs and other chemicals on the liver. 2nd ed. Philadelphia: Lippincott, 1999, pp. 483-91.(Expert review of hepatotoxicity of neuroleptic drugs including chlorpromazine published in 1999; several hundred cases of jaundice due to chlorpromazine have been reported, usually cholestatic, arising after 1-5 weeks, often with fever and eosinophilia, sometimes causing vanishing bile duct syndrome; other phenothiazines have only rarely been linked to a similar form of liver injury, except for prochlorperazine).
- Larrey D, Ripault M-P. Hepatotoxicity of psychotropic drugs and drugs of abuse. In, Kaplowitz N, DeLeve LD, eds. Drug-induced liver disease. 3rd ed. Amsterdam: Elsevier, 2013, pp. 443-62.(Review of hepatotoxicity of phenothiazines mentions that hundreds of cases of chlorpromazine jaundice have been published, frequency ~0.5-1%; onset in 2-5 weeks, usually acute cholestatic hepatitis with jaundice and pruritus; a prodrome of fever and abdominal pain is common; prolonged course in 7% but often benign; other phenothiazines have been linked to liver injury similar to that of chlorpromazine, “but with a lower frequency”).
- Meyer JM. Pharmacotherapy of psychosis and mania. In, Brunton LL, Hilal-Dandan R, Knollman BC, eds. Goodman & Gilman's the pharmacological basis of therapeutics. 13th ed. New York: McGraw-Hill, 2018, pp. 279-302.(Textbook of pharmacology and therapeutics).
- Brunold H. Ther Umsch. 1959;16:90–2. [Experiences with a new phenothiazine derivative. Mellaril, Sandoz] [PubMed: 13647410](Among 89 patients treated with thioridazine with escalating doses to 800 mg/day, one patient developed jaundice which was not otherwise characterized).
- Block SL. Jaundice following thioridazine administration. Am J Psychiatry. 1962;119:77. [PubMed: 13870055](79 year old woman with dementia developed elevated liver enzymes but without symptoms 9 months after starting thioridazine, resolving rapidly with stopping; jaundice was not mentioned in text of the report).
- Winkelmayer R. Subicterus following the administration of thioridazine and chlordiazepoxide. Del Med J. 1966;38:334–6. [PubMed: 5978248](35 year old man developed jaundice 24 days after starting thioridazine with slight elevation in “icteric index”, but normal serum bilirubin and aminotransferase levels, a pattern that recurred on chlordiazepoxide but not upon restarting thioridazine).
- Reinhart MJ, Benson RM, Kwass SK, Storey WF. Suggestive evidence of hepatotoxicity concomitant with thioridazine hydrochloride use. JAMA. 1966;197:767–9. [PubMed: 5953369](3 cases of thioridazine hepatotoxicity; case 1, 53 year old man with rise in ALT [600 U/L], Alk P [~10 fold] and bilirubin [5.2 mg/dL] within days of switching from chlorpromazine to thioridazine and rapid recovery with stopping; case 2, 32 year old woman switched from chlorpromazine to thioridazine because of ALT elevations and 4 months later developed fatigue [bilirubin normal, ALT 320 U/L, Alk P normal], resolving upon stopping; case 3, 17 year old boy had minor ALT elevations [<60 U/L] without Alk P or bilirubin abnormalities on thioridazine).
- Walker CO, Combes B. Biliary cirrhosis induced by chlorpromazine. Gastroenterology. 1966;51:631–40. [PubMed: 5926937](32 year old woman and 31 year old man developed persistent jaundice [>4 years], cholestasis and liver fibrosis 3 and 4 weeks after starting chlorpromazine; acute cholestatic hepatitis evolving into chronic form with biopsies showing cirrhosis and complications of portal hypertension, most likely due to vanishing bile duct syndrome).
- Barancik M, Brandborg LL, Albion MJ. Thioridazine-induced cholestasis. JAMA. 1967;200:69–70. [PubMed: 6071857](34 year old man with chronic alcoholism developed jaundice 5 months after being switched from chlorpromazine to thioridazine [bilirubin 6.7 mg/dL, ALT 59 U/L, Alk P 7 Bessey-Lowry U/L], resolving rapidly upon stopping; biopsy showed intrahepatic cholestasis and not alcoholic hepatitis).
- Kane FJ Jr, Moore LP. Hepatotoxicity occurring with thioridazine therapy. South Med J. 1971;64:573. [PubMed: 5573073](13 year old boy developed transient rash after 22 days of thioridazine [bilirubin 2.2 mg/dL, 1.1 direct], which then decreased to normal weeks after stopping; ALT and Alk P levels were not obtained at time of rash, but were normal in follow up).
- Ishak KG, Irey NS. Hepatic injury associated with the phenothiazines. Clinicopathologic and follow-up study of 36 patients. Arch Pathol. 1972;93:283–304. [PubMed: 5017281](Review of 36 liver biopsies of patients with phenothiazine induced liver injury from Armed Forces Institute of Pathology, 33 due to chlorpromazine and 3 to prochlorperazine hepatotoxicity; mean time to onset 15 days, eosinophilia in 73%, mean peak bilirubin 12.4 mg/dL, Alk P ~8 fold elevated, ALT 146 U/L; 6 [17%] had prolonged course for 10 to 16 months).
- Weiden PL, Buckner CD. Thioridazine toxicity. Agranulocytosis and hepatitis with encephalopathy. JAMA. 1973;224:518–20. [PubMed: 4739612](54 year old man developed cellulitis and jaundice 7 weeks after starting thioridazine [bilirubin 7.0 mg/dL, AST 68 U/L, Alk P ~5 times ULN], with neutropenia and agranulocytosis on bone marrow biopsy; slow but complete recovery of bone marrow and liver).
- Kristensen O. Tidsskr Nor Laegeforen. 1975;95:1910–1. [Icterus induced by thioridazine (Melleril). Report of 1 case] Norwegian. [PubMed: 1188902](58 year old with a history of chlorpromazine hepatotoxicity developed jaundice 15 months after starting thioridazine and imipramine [bilirubin 3.5 mg/dL, ALT 115 U/L, Alk P 1.5 times ULN], resolving upon stopping both drugs and worsening after short rechallenge with thioridazine).
- Døssing M, Andreasen PB. Drug-induced liver disease in Denmark. An analysis of 572 cases of hepatotoxicity reported to the Danish Board of Adverse Reactions to Drugs. Scand J Gastroenterol. 1982;17:205–11. [PubMed: 6982502](Among 572 cases of drug induced liver disease seen between 1968-78 in Denmark, 51 were attributed to chlorpromazine [9%, ranking 2nd behind halothane], latency averaged 14 days [range 11-46]; 5 deaths; no mention of other phenothiazines).
- Kaplowitz N, Aw TY, Simon FR, Stolz A. Drug-induced hepatotoxicity. Ann Intern Med. 1986;104:826–39. [PubMed: 3518564](Review of drug induced hepatotoxicity including phenothiazine jaundice).
- Munyon WH, Salo R, Briones DF. Cytotoxic effects of neuroleptic drugs. Psychopharmacology (Berl). 1987;91:182–8. [PubMed: 2883697](In vitro assay for cytotoxicity of 8 neuroleptic drugs found that chlorpromazine was more toxic than haloperidol or loxapine, but similar to other phenothiazines).
- Regal RE, Bili JE, Glazer HM. Phenothiazine-induced cholestatic jaundice. Clinical Pharmacy. 1987;6:787–94. [PubMed: 2905941](Review of phenothiazine induced liver injury; cross sensitivity is rare “but does exist”).
- Urberg M. Thioridazine-induced non-icteric hepatotoxicity. Report of a case. J Fam Pract. 1990;30:342–3. [PubMed: 2307948](34 year old man with 100 lb weight gain after 2 years of thioridazine therapy was thought to have “tense ascites” and “hepatic failure”, but liver tests were normal except for ALT of 46 U/L; ascites was not present 1 week later when ultrasound showed “loss of the normal internal echo architecture of the liver”).
- Pillans PI. Drug associated hepatic reactions in New Zealand: 21 years experience. N Z Med J. 1996;109:315–9. [PubMed: 8816722](Over 21 year period in New Zealand, there were 943 official reports of liver injury involving 205 drugs; chlorpromazine was in the top 20 drugs implicated accounting for 2.7% of cases; prochlorperazine was cause of 4 cases, but other phenothiazines not mentioned).
- Sabaté M, Ibáñez L, Pérez E, Vidal X, Buti M, Xiol X, Mas A, et al. Risk of acute liver injury associated with the use of drugs: a multicentre population survey. Aliment Pharmacol Ther. 2007;25:1401–9. [PubMed: 17539979](Among 126 cases of drug induced liver injury seen in Spain between 1993-2000, 3 were due to chlorpromazine with relative risk of 613: and frequency of 261 per 100,000 person year exposures; no other phenothiazine discussed).
- Chalasani N, Fontana RJ, Bonkovsky HL, Watkins PB, Davern T, Serrano J, Yang H, Rochon J., Drug Induced Liver Injury Network (DILIN). Causes, clinical features, and outcomes from a prospective study of drug-induced liver injury in the United States. Gastroenterology. 2008;135:1924–34. [PMC free article: PMC3654244] [PubMed: 18955056](Among 300 cases of drug induced liver disease in the US collected between 2004 and 2008, none were attributed to phenothiazines).
- Flanagan RJ. Fatal toxicity of drugs used in psychiatry. Hum Psychopharmacol. 2008;23 Suppl 1:43–51. [PubMed: 18098225](Deaths from fatal poisonings decreased in England and Wales between 1993-2004, antipsychotic overdose fatalities were higher for phenothiazines than atypicals; deaths/million prescriptions being 29 for chlorpromazine, 15.5 thioridazine, 3.9 trifluoperazine, 13.3 olanzapine, 21 clozapine and 31.3 quetiapine; deaths were due to respiratory depression, not acute liver failure).
- Reuben A, Koch DG, Lee WM., Acute Liver Failure Study Group. Drug-induced acute liver failure: results of a U.S. multicenter, prospective study. Hepatology. 2010;52:2065–76. [PMC free article: PMC3992250] [PubMed: 20949552](Among 1198 patients with acute liver failure enrolled in a US prospective study between 1998 and 2007, 133 were attributed to drug induced liver injury including 4 due to psychotropic agents; one each due to quetiapine, nefazodone, fluoxetine and venlafaxine, but none due to phenothiazines).
- Molleston JP, Fontana RJ, Lopez MJ, Kleiner DE, Gu J, Chalasani N., Drug-induced Liver Injury Network. Characteristics of idiosyncratic drug-induced liver injury in children: results from the DILIN prospective study. J Pediatr Gastroenterol Nutr. 2011;53:182–9. [PMC free article: PMC3634369] [PubMed: 21788760](Among 30 children with suspected drug induced liver injury, half [n=15] were due to antimicrobials [minocycline 4, INH 3, azithromycin 3] and the rest largely due to CNS agents and anticonvulsants; one case was attributed to perphenazine).
- Drugs for psychiatric disorders. Treat Guidel Med Lett. 2013;11(130):53–64. [PubMed: 23715100](Concise review and recommendations on use of antidepressants and antipsychotic medications including phenothiazines; no discussion of hepatotoxicity).
- Marwick KF, Taylor M, Walker SW. Antipsychotics and abnormal liver function tests: systematic review. Clin Neuropharmacol. 2012;35:244–53. [PubMed: 22986798](Systematic review of the literature found rates of any serum enzyme elevation during antipsychotic therapy to range from 5-78% and "clinically significant' elevations in 0-15%; lists 8 reports of clinically apparent liver injury due thioridazine).
- Hernández N, Bessone F, Sánchez A, di Pace M, Brahm J, Zapata R, A, Chirino R, et al. Profile of idiosyncratic drug induced liver injury in Latin America. An analysis of published reports. Ann Hepatol. 2014;13:231–9. [PubMed: 24552865](Systematic review of literature of drug induced liver injury in Latin American countries published from 1996 to 2012 identified 176 cases, only one of which was attributed to chlorpromazine, the only antipsychotic medication listed).
- Chalasani N, Bonkovsky HL, Fontana R, Lee W, Stolz A, Talwalkar J, Reddy KR, et al. United States Drug Induced Liver Injury Network. Features and outcomes of 899 patients with drug-induced liver injury: The DILIN Prospective Study. Gastroenterology. 2015;148:1340–52.e7. [PMC free article: PMC4446235] [PubMed: 25754159](Among 899 cases of drug induced liver injury enrolled in a US prospective study between 2004 and 2013, 5 cases [0.6%] were attributed to antipsychotic agents, including 3 due to quetiapine and 2 to olanzapine, but none to thioridazine or other phenothiazines).
- Drugs for psychotic disorders. Med Lett Drugs Ther. 2016;58(1510):160–4. [PubMed: 27960194](Concise review of medications available in the US for therapy of psychotic disorders; mentions that the phenothiazines commonly cause sedation, postural hypotension and weight gain and often have extrapyramidal effects, but does not mention ALT elevations or hepatotoxicity).
- Schreiner NM, Windham S, Barker A. Atypical neuroleptic malignant syndrome: diagnosis and proposal for an expanded treatment algorithm: a case report. A A Case Rep. 2017;9:339–43. [PubMed: 28767476](48 year old man with bipolar disorder and NASH underwent liver transplantation and developed confusion, dyskinesia, rigidity, hyperthermia and tachycardia/tachypnea postoperatively having been given lithium, lamotrigine, promethazine and ziprasidone, responding to therapy of neuroleptic malignant syndrome with benzodiazepines and propofol).
- Baeza I, de la Serna E, Calvo-Escalona R, Merchán-Naranjo J, Rodríguez-Latorre P, Martínez-Cantarero MC, Andrés P, et al. One-year prospective study of liver function tests in children and adolescents on second-generation antipsychotics: is there a link with metabolic syndrome? J Child Adolesc Psychopharmacol. 2018;28:463–73. [PubMed: 29975563](Among 216 children and adolescents starting atypical antipsychotics, mean weight gain at 6 months was 6.5 kg and mean ALT levels increased by 8.6 U/L, while among 37 taking olanzapine mean weight gain was 10.3 kg and ALT increase 2.6 U/L; increases in ALT associated with development of the metabolic syndrome, mean ALT increasing by 27.8 U/L at 6 months).
- Review Fluphenazine.[LiverTox: Clinical and Researc...]Review Fluphenazine.. LiverTox: Clinical and Research Information on Drug-Induced Liver Injury. 2012
- Metabolic activation of the phenothiazine antipsychotics chlorpromazine and thioridazine to electrophilic iminoquinone species in human liver microsomes and recombinant P450s.[Chem Biol Interact. 2009]Metabolic activation of the phenothiazine antipsychotics chlorpromazine and thioridazine to electrophilic iminoquinone species in human liver microsomes and recombinant P450s.Wen B, Zhou M. Chem Biol Interact. 2009 Oct 7; 181(2):220-6. Epub 2009 May 29.
- Effect of thioridazine on experimental cutaneous staphylococcal infections.[In Vivo. 2014]Effect of thioridazine on experimental cutaneous staphylococcal infections.Hahn BL, Sohnle PG. In Vivo. 2014 Jan-Feb; 28(1):33-8.
- Review Trifluoperazine.[LiverTox: Clinical and Researc...]Review Trifluoperazine.. LiverTox: Clinical and Research Information on Drug-Induced Liver Injury. 2012
- [ON THE ACTION OF A NEW PHARMACOLOGIC FORM OF A PHENOTHIAZINE DERIVATIVE, SLOW ACTING THIORIDAZINE, IN SCHIZOPHRENICS].[Rass Studi Psichiatr. 1965][ON THE ACTION OF A NEW PHARMACOLOGIC FORM OF A PHENOTHIAZINE DERIVATIVE, SLOW ACTING THIORIDAZINE, IN SCHIZOPHRENICS].BORGHESI R, MEDAGLINI E. Rass Studi Psichiatr. 1965; 54:55-78.
- Thioridazine - LiverToxThioridazine - LiverTox
Your browsing activity is empty.
Activity recording is turned off.
See more...