NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
LiverTox: Clinical and Research Information on Drug-Induced Liver Injury [Internet]. Bethesda (MD): National Institute of Diabetes and Digestive and Kidney Diseases; 2012-.

LiverTox: Clinical and Research Information on Drug-Induced Liver Injury [Internet].
Show detailsOVERVIEW
Introduction
Tranylcypromine is a nonhydrazine monoamine oxidase inhibitor (MAO inhibitor) used in therapy of severe depression. Tranylcypromine therapy is associated with rare instances of clinically apparent acute liver injury.
Background
Tranylcypromine (tran" il sip' roe meen) is an antidepressant that acts through irreversible inhibition of monoamine oxidases, enzymes that inactivate several neurotransmitter amines such as norepinephrine and serotonin. Tranylcypromine is a nonspecific MAO inhibitor with activity against both MAO A (found in highest concentrations in the intestines) and MAO B (found largely in the brain and in platelets). By inhibition of catabolism of serotonin and norepinephrine, tranylcypromine increases brain levels of these neurotransmitters, actions which probably underlie its antidepressant effects. Tranylcypromine was approved for use as therapy of major depression in the United States in 1961, but it is now rarely used because of the availability of more potent and better tolerated antidepressants such as the tricyclic antidepressants and the selective serotonin reuptake inhibitors. Tranylcypromine is available in generic forms and under the brand name of Parnate as tablets of 10 mg. The usual adult dose of tranylcypromine is 30 to 60 mg daily in divided doses. Common side effects include drowsiness, dizziness, headache, insomnia, tremor, dry mouth, nausea, and sexual dysfunction. Tranylcypromine interacts with many medications as well as many foods and beverages, and patients require careful monitoring and education. Uncommon but potentially serious adverse events include hypertensive crises [often due to dietary tyramine], serotonin syndrome, withdrawal mania and hypersensitivity reactions.
Hepatotoxicity
Tranylcypromine, like most monoamine oxidase inhibitors, can cause transient serum aminotransferase elevations in a proportion of patients. These elevations are usually mild, asymptomatic and self-limited and do not require dose modification. Tranylcypromine has also been associated with rare cases of acute, clinically apparent liver injury. The few cases described have resembled those caused by other MAO inhibitors. The time to clinical onset is typically 1 to 4 months and the usual pattern of serum enzyme elevations is hepatocellular (Case 1), although cholestatic injury has also been described. Immunoallergic features (rash, fever, eosinophilia) are uncommon as is autoantibody formation.
Likelihood score: D (possible rare cause of clinically apparent liver injury).
Mechanism of Injury
The mechanism by which tranylcypromine causes serum aminotransferase elevation is not known. It undergoes extensive hepatic metabolism and a possible cause of liver injury is production of a toxic intermediate of metabolism. Unlike other nonselective MAO inhibitors, tranylcypromine is not a hydrazine derivative which may account in part for the apparent lower risk of hepatotoxicity compared to phenelzine.
Outcome and Management
The serum aminotransferase elevations that occur on tranylcypromine therapy are usually transient and mild and do not require dose modification or discontinuation of therapy. The acute liver injury caused by tranylcypromine is typically self-limited, but progressive and fatal instances of acute hepatitis have been reported. Rechallenge usually causes a prompt recurrence of the liver injury and should be avoided. Patients with tranylcypromine induced liver injury are likely to have cross sensitivity to other monoamine oxidase inhibitors, but should be able to tolerate tricyclic antidepressants or selective serotonin reuptake inhibitors.
Drug Class: Antidepressant Agents
Other drugs in the Subclass, MAO Inhibitors: Isocarboxazid, Phenelzine
CASE REPORT
Case 1. Acute self-limited hepatitis due to tranylcypromine.(1)
A 49 year old woman with recurrent depression was treated with tranylcypromine (20 mg per day) and developed fatigue after 6 and jaundice after 7 weeks of therapy. She had no history of liver disease, nor exposure to or risk factors for viral hepatitis, and drank minimal amounts of alcohol. She was not taking other medications. Physical examination showed jaundice and hepatomegaly, but no rash or fever. Blood tests showed elevations in serum enzymes and bilirubin levels of 14.9 mg/dL (Table). All medications were stopped and she began to improve with clearance of jaundice within a week. A liver biopsy showed inflammation, hepatocellular injury and intrahepatic cholestasis thought to be compatible with drug-induced liver injury. At 21 days after presentation, she was rechallenged with tranylcypromine for two days, developing nausea and vomiting with rise in AST levels from 19 U/L to 540 U/L without recurrence of jaundice (but a slight rise in direct bilirubin). A cholecystogram done after recovery was normal.
Key Points
| Medication: | Tranylcypromine (20-30 mg daily) |
|---|---|
| Pattern: | Hepatocellular (R=9) |
| Severity: | 3+ (jaundice, hospitalization) |
| Latency: | 6 weeks initially, within 24 hours on rechallenge |
| Recovery: | ~1 month |
| Other medications: | None mentioned |
Laboratory Values
| Time After Starting | Time After Starting | ALT (U/L) | Alk P (KA U/L) | Bilirubin (mg/dL) | Comments |
|---|---|---|---|---|---|
| Tranylcypromine taken for 7 weeks | |||||
| 7 weeks | 0 | 670 | 26.5 | 14.9 | |
| 8 weeks | 5 days | 410 | 5.0 | ||
| 9 weeks | 10 days | 340 | 3.2 | ||
| 10 weeks | 17 days | 36 | 6.5 | 0.9 | |
| Tranylcypromine restarted for 2 days | |||||
| 10 weeks (0) | 21 days | 19 | 0.6 | Rechallenge | |
| 22 (0) days | 540 | 1.1 | |||
| 23 (1) day | 420 | ||||
| 24 (2) days | 200 | 0.5 | |||
| 25 (3) days | 67 | ||||
| 27 (4) days | 31 | 0.4 | |||
| Normal Values | <35 | <13 | <1.2 | ||
Dates and values estimated from Figure 1. Numbers in parentheses are days after starting and stopping rechallenge doses.
Comment
The monoamine oxidase (MAO) inhibitors are not commonly used and most reported cases of hepatotoxicity were published before 1970. The described case is convincing because of the timing of onset and the response to rechallenge. The case report predates the availability of tests for hepatitis A, B and C and modern imaging methods that have made rechallenge less necessary in confirming the diagnosis. Several case reports have documented cross sensitivity to hepatic injury among the different MAO inhibitors.
PRODUCT INFORMATION
REPRESENTATIVE TRADE NAMES
Tranylcypromine – Parnate®
DRUG CLASS
Antidepressant Agents
Product labeling at DailyMed, National Library of Medicine, NIH
CHEMICAL FORMULA AND STRUCTURE
| DRUG | CAS REGISTRY NUMBER | MOLECULAR FORMULA | STRUCTURE |
|---|---|---|---|
| Tranylcypromine | 95-62-5 | C9-H11-N |
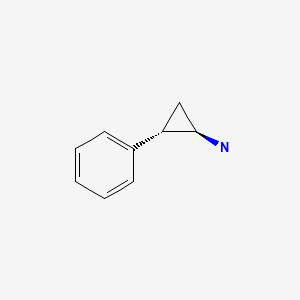
|
CITED REFERENCE
- 1.
- Bandt C, Hofbauer FW. Liver injury associated with tranylcypromine therapy. JAMA. 1964;188:752–3. [PubMed: 14122685]
ANNOTATED BIBLIOGRAPHY
References updated: 08 April 2020
Abbreviations: MAO, monoamine oxidase; SSRI, selective serotonin reuptake inhibitor; SNRI, serotonin and norepinephrine reuptake inhibitor.
- Zimmerman HJ. Antidepressants. In, Zimmerman HJ. Hepatotoxicity: the adverse effects of drugs and other chemicals on the liver. 2nd ed. Philadelphia: Lippincott, 1999, pp. 493-8.(Expert review of hepatotoxicity published in 1999; hepatic injury caused by monoamine oxidase [MAO] inhibitors is similar to that of isoniazid with which they share structural similarity as hydrazines; the pattern of injury is typically hepatocellular and arises within 1-6 months of starting therapy; cases of fatal acute liver failure have been described most commonly with the initial MAO inhibitor, iproniazid, and less commonly with phenelzine and isocarboxazid, and least commonly with the nonhydrazide MAO inhibitor, tranylcypromine).
- Larrey D, Ripault MP. Hepatotoxicity of psychotropic drugs and drugs of abuse. In, Kaplowitz N, DeLeve LD, eds. Drug-induced liver disease. 3rd ed. Amsterdam: Elsevier, 2013, pp. 443-62.(Review of hepatotoxicity of antidepressants mentions that among MAO inhibitors iproniazid most commonly caused liver injury and phenelzine rarely; tranylcypromine is not discussed).
- O'Donnell JM, Bies RR, Shelton RC. Drug therapy of depression and anxiety disorders. In, Brunton LL, Hilal-Dandan R, Knollman BC, eds. Goodman & Gilman’s the pharmacological basis of therapeutics. 13th ed. New York: McGraw-Hill, 2018, pp. 267-77.(Textbook of pharmacology and therapeutics).
- Rosenblum LE, Korn LJ, Zimmerman HJ. Hepatocellular jaundice as a complication of iproniazid therapy. Arch Intern Med 1960; 105: 115-25. 14438978. [PubMed: 14438978](Classic paper on iproniazid hepatotoxicity; review of 90 patients; more common in women, ages 25-75 years, onset in 1-4 months [~95%], usually hepatocellular pattern similar to viral hepatitis, 22% mortality and demonstration that this is higher than in acute viral hepatitis).
- Bandt C, Hofbauer FW. Liver injury associated with tranylcypromine therapy. JAMA. 1964;188:752–3. [PubMed: 14122685](49 year old developed fatigue after 6 and jaundice after 7 weeks of tranylcypromine therapy [bilirubin 14.9 mg/dL, AST 670 U/L, Alk P 2x ULN], with rapid rise in AST [to ~600 U/L] with rechallenge: Case 1).
- Holdsworth CD, Atkinson M, Goldie W. Hepatitis caused by the newer amine-oxidase-inhibiting drugs. Lancet. 1961;2:621–3. [PubMed: 13715243](Four cases of severe liver injury with cross sensitivity to several MAO inhibitors including iproniazid, pheniprazine and nialamide; case 4 was 56 year old woman who developed jaundice and itching after 5 months of phenelzine [bilirubin 2.8 mg/dL, ALT 150 U/L Alk P 3 times ULN], resolving rapidly upon stopping).
- Crisp AH, Hays P, Carter A. Three amine-oxidase inhibitor drugs in the treatment of depression. Relative value and toxic effects. Lancet. 1961;1:17–8. [PubMed: 13696480](Prospective study of liver test abnormalities during courses of iproniazid [n=17], nialamide [18] and peniprazine [20] with minor enzyme increases noted; no data on frequency of levels above normal).
- Cook GC, Sherlock S. Jaundice and its relation to therapeutic agents. Lancet. 1965;1:175–9. [PubMed: 14238042](Summary of cases of drug induced liver disease seen at Royal Free Hospital from 1959-65; 11 cases of acute liver failure due to drugs including iproniazid [n=3], phenelzine [2], phenoxypropazine [2], prochlorperazine [1], and halogenated anesthetics [3]; 20 cases of cholestatic hepatitis due to drugs, 18 due to chlorpromazine, 1 perphenazine and 1 nitrofurantoin).
- Steingart AB, Cotterchio M. Do antidepressants cause, promote, or inhibit cancers? J Clin Epidemiol. 1995;48:1407–12. [PubMed: 7490604](Conflicting data from animal studies and epidemiological surveys have provided little evidence of a link between antidepressant use and breast, liver or other cancer after control for confounding variables).
- Lucena MI, Carvajal A, Andrade RJ, Velasco A. Antidepressant-induced hepatotoxicity. Expert Opin Drug Saf. 2003;2:249–62. [PubMed: 12904104](Review of hepatotoxicity of antidepressants; antidepressant use has increased markedly between 1992 and 2002, accounting for 5% of cases of hepatotoxicity; MAO inhibitors were first antidepressants developed; iproniazid caused a severe hepatitis and was withdrawn; phenelzine is still in use, but has been associated with severe cases of hepatitis and development of cirrhosis).
- Chalasani N, Fontana RJ, Bonkovsky HL, Watkins PB, Davern T, Serrano J, Yang H, Rochon J., Drug Induced Liver Injury Network (DILIN). Causes, clinical features, and outcomes from a prospective study of drug-induced liver injury in the United States. Gastroenterology. 2008;135:1924–34. [PMC free article: PMC3654244] [PubMed: 18955056](Among 300 cases of drug induced liver disease in the US collected from 2004 to 2008, none were attributed to tranylcypromine or other MAO inhibitors).
- Shulman KI, Herrmann N, Walker SE. Current place of monoamine oxidase inhibitors in the treatment of depression. CNS Drugs. 2013;27:789–97. [PubMed: 23934742](History of the discovery that hydrazine-based drugs had potent antidepressant activity and subsequent development of nonspecific and specific, irreversible and reversible MAO A and B inhibitors which have similar antidepressant effects but different relative risks for complications such as hypertension from dietary intake of tyramine [as in aged cheese] and serotonin syndrome from use of a second serotonin-enhancing agent, such as a tricyclic, SSRI or SNRI as well as some opiates).
- Hernández N, Bessone F, Sánchez A, di Pace M, Brahm J, Zapata R, A, Chirino R, et al. Profile of idiosyncratic drug induced liver injury in Latin America. An analysis of published reports. Ann Hepatol. 2014;13:231–9. [PubMed: 24552865](Systematic review of literature of drug induced liver injury in Latin American countries published from 1996 to 2012 identified 176 cases, only one of which was attributed to an antidepressant [amitriptyline] and none to a MAO inhibitor, SSRI or SNRI).
- Heijnen WT, De Fruyt J, Wierdsma AI, Sienaert P, Birkenhäger TK. Efficacy of tranylcypromine in bipolar depression: a systematic review. J Clin Psychopharmacol. 2015;35:700–5. [PubMed: 26479223](Systematic review identified 4 studies in 145 patients showing a 74% response rate overall and conversion to mania in 6% of patients, but no discussion or adverse events or hepatotoxicity).
- Chalasani N, Bonkovsky HL, Fontana R, Lee W, Stolz A, Talwalkar J, Reddy KR, et al. United States Drug Induced Liver Injury Network. Features and outcomes of 899 patients with drug-induced liver injury: The DILIN Prospective Study. Gastroenterology. 2015;148:1340–52.e7. [PMC free article: PMC4446235] [PubMed: 25754159](Among 899 cases of drug induced liver injury enrolled in a US prospective study between 2004 and 2013, 20 cases [2%] were attributed to antidepressants including 9 due to SNRIs [7 to duloxetine, 1 each to nefazodone and trazodone], 5 to bupropion, 5 to SSRIs [3 to escitalopram, and 1 each to fluoxetine and sertraline], and only 1 to tricyclics [imipramine] but none to MAO inhibitors).
- Voican CS, Martin S, Verstuyft C, Corruble E, Perlemuter G, Colle R. Liver function test abnormalities in depressed patients treated with antidepressants: a real-world systematic observational study in psychiatric settings. PLoS One. 2016;11:e0155234. [PMC free article: PMC4865191] [PubMed: 27171561](Among 321 psychiatric inpatients, only 116 [36%] had liver tests performed and only 18 during therapy with an antidepressant, 3 of which were suspected to have drug induced liver injury, 1 each with escitalopram, venlafaxine and amitriptyline, all without jaundice and 2 without symptoms, all 3 resolving).
- Friedrich ME, Akimova E, Huf W, Konstantinidis A, Papageorgiou K, Winkler D, Toto S, et al. Drug-induced liver injury during antidepressant treatment: results of AMSP, a drug surveillance program. Int J Neuropsychopharmacol. 2016;19(4):pyv126. pii. [PMC free article: PMC4851269] [PubMed: 26721950](Among 184,234 psychiatric inpatients from 80 hospitals, 149 cases [0.08%] of drug induced liver injury were reported including 22 of 70,060 [0.03%] receiving SSRIs, 71 of 50,201 [0.14%] patients treated with tricyclics and 3 of 3869 receiving MAO inhibitors [0.08%]).
- Chen VC, Lin CF, Hsieh YH, Liang HY, Huang KY, Chiu WC, Lee Y, McIntyre RS, et al. Hepatocellular carcinoma and antidepressants: a nationwide population-based study. Oncotarget. 2017;8:30464–70. [PMC free article: PMC5444756] [PubMed: 27783998](Among almost 50,000 cases of hepatocellular carcinoma registered in the Taiwan National Health Insurance Research Database, the rate of antidepressant use was lower than in approximately 250,000 matched controls from the database).
- Ulrich S, Ricken R, Adli M. Tranylcypromine in mind (Part I): Review of pharmacology. Eur Neuropsychopharmacol. 2017;27:697–713. [PubMed: 28655495](Review of the mechanism of action, pharmacology and toxicity of tranylcypromine).
- Ricken R, Ulrich S, Schlattmann P, Adli M. Tranylcypromine in mind (Part II): Review of clinical pharmacology and meta-analysis of controlled studies in depression. Eur Neuropsychopharmacol. 2017;27:714–31. [PubMed: 28579071](Review of the clinical efficacy and adverse events of tranylcypromine therapy mentions that the most common adverse events are dizziness, sedation, insomnia, headache and dry mouth and that weight gain and hypertension are uncommon; no mention of hepatotoxicity or ALT elevations).
- Ferrajolo C, Scavone C, Donati M, Bortolami O, Stoppa G, Motola D, Vannacci A, et al. DILI-IT Study Group. Antidepressant-Induced Acute liver injury: a case-control study in an Italian inpatient population. Drug Saf. 2018;41:95–102. [PubMed: 28770534](Among 179 cases of hospitalizations for unexplained acute liver injury enrolled in an Italian prospective study between 2010 and 2014, 17 had been exposed to antidepressants the major implicated agents being citalopram [n=4], sertraline [n=3], paroxetine [n=3], tricyclics [n=2], trazodone [n=1], fluoxetine [n=1], and duloxetine [n=1]; no MAO inhibitors listed).
- Billioti de Gage S, Collin C, Le-Tri T, Pariente A, Bégaud B, Verdoux H, Dray-Spira R, et al. Antidepressants and hepatotoxicity: a cohort study among 5 million individuals registered in the French National Health Insurance Database. CNS Drugs. 2018;32:673–84. [PMC free article: PMC6061298] [PubMed: 29959758](Among 5 million persons identified in a national French health insurance database who started an antidepressant between 2010 and 2015, 382 developed serious liver injury resulting in hospitalization, rates per 100,0000 persons-years being 19 for SSRIs, 22 venlafaxine, 13 duloxetine, and 33 mirtazapine; no MAO inhibitors discussed).
- van der Heide D, Merckelbach H, van Harten P. Tijdschr Psychiatr. 2018;60:544–7. [Tranylcypromine and khat: a potentially fatal combination] [PubMed: 30132583](30 year old immigrant from East Africa to the Netherlands was treated with low doses of tranylcypromine and developed a severe headache and inability to speak after chewing 8 leaves of khat but then spontaneously recovered without residual neurologic defects, and was diagnosed as have hypertension related reversible cerebral vasoconstriction syndrome perhaps related to the inhibition of MAO and neurotransmitter substances in khat).
- Ferreira-Garcia R, da Rocha Freire RC, Appolinário JC, Levitan MN, Halkjær-Lassen RD, Bueno JR, Nardi AE. Tranylcypromine plus amitriptyline for electroconvulsive therapy-resistant depression: A Long-Term Study. J Clin Psychopharmacol. 2018;38:502–4. [PubMed: 30106881](Among 30 patients with resistant depression treated with the combination of tranylcypromine and amitriptyline, adverse events were common [dizziness, headache, dry mouth, nausea, sexual dysfunction] but generally mild, and there were no severe adverse events, no hypertensive crises, new onset hypertension or serotonin syndrome; no mention of hepatotoxicity).
- Drugs for depression. Med Lett Drugs Ther. 2020;62(1592):25–32. [PubMed: 32320387](Concise review of the mechanism of action, clinical efficacy, safety and costs of drugs for depression, mentions that tricyclics and MAO inhibitors remain valuable alternatives for treatment of moderate-to-severe depression, despite concerns about their safety; hepatotoxicity is mentioned only for nefazodone [now rarely used because of severe hepatotoxicity] and duloxetine [in heavy drinkers]).
- PMCPubMed Central citations
- PubChem SubstanceRelated PubChem Substances
- PubMedLinks to PubMed
- Insufficient recovery of monoamine oxidase in a bioequivalence study of the monoamine oxidase inhibitor tranylcypromine: Recommendation of the tranylcypromine enantiomer test.[Int J Clin Pharmacol Ther. 2022]Insufficient recovery of monoamine oxidase in a bioequivalence study of the monoamine oxidase inhibitor tranylcypromine: Recommendation of the tranylcypromine enantiomer test.Ulrich S, Hock D, Guth V, Erenmemisoglu A, Scheidel B. Int J Clin Pharmacol Ther. 2022 May; 60(5):242-252.
- [Psychopharmacotherapy with the MAO-inhibitor Tranylcypromine Key Aspects and Trends in Theory and Practice].[Fortschr Neurol Psychiatr. 2023][Psychopharmacotherapy with the MAO-inhibitor Tranylcypromine Key Aspects and Trends in Theory and Practice].Ulrich S, Lewitzka U. Fortschr Neurol Psychiatr. 2023 Nov 21; . Epub 2023 Nov 21.
- Review Tranylcypromine in mind (Part II): Review of clinical pharmacology and meta-analysis of controlled studies in depression.[Eur Neuropsychopharmacol. 2017]Review Tranylcypromine in mind (Part II): Review of clinical pharmacology and meta-analysis of controlled studies in depression.Ricken R, Ulrich S, Schlattmann P, Adli M. Eur Neuropsychopharmacol. 2017 Aug; 27(8):714-731. Epub 2017 Jun 1.
- Ring-substituted analogues of tranylcypromine as monoamine oxidase inhibitors.[J Neural Transm Suppl. 1990]Ring-substituted analogues of tranylcypromine as monoamine oxidase inhibitors.Sherry RL, Baker GB, Coutts RT, Mousseau DD. J Neural Transm Suppl. 1990; 32:107-12.
- Review Antidepressant treatment with MAO-inhibitors during general and regional anesthesia: a review and case report of spinal anesthesia for lower extremity surgery without discontinuation of tranylcypromine.[Int J Clin Pharmacol Ther. 2013]Review Antidepressant treatment with MAO-inhibitors during general and regional anesthesia: a review and case report of spinal anesthesia for lower extremity surgery without discontinuation of tranylcypromine.Krings-Ernst I, Ulrich S, Adli M. Int J Clin Pharmacol Ther. 2013 Oct; 51(10):763-70.
- Tranylcypromine - LiverToxTranylcypromine - LiverTox
Your browsing activity is empty.
Activity recording is turned off.
See more...