33. Integrated patient information systems
33.1. Introduction
It is generally accepted that appropriate information sharing within departments in an organisation and between different organisations is of importance in supporting co-ordinated care for patients, improving patient experience and achieving greater efficiency and value from health delivery systems.
An integrated patient information system would allow authorised health and social care professionals to have access to the patient’s clinical information (for example, laboratory results, medications, allergies and clinical notes) from multiple providers. It could also allow the patient to view the record and where appropriate add any self-monitoring information. Many benefits and efficiencies can flow from information being recorded, at contact with health and care services, and shared securely between those providing care.
33.2. Review question: Do integrated patient information systems throughout the AME pathway (primary and secondary care) improve patient outcomes?
For full details see review protocol in Appendix A.
Table 1
PICO characteristics of review question.
33.3. Clinical evidence
One study was included in the review;7 these are summarised in Table 2 below. The study reported only important outcomes and did not report any critical outcomes stated in the protocol.
Table 2
Summary of studies included in the review.
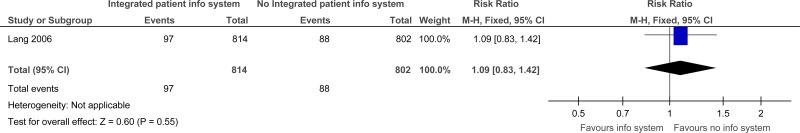
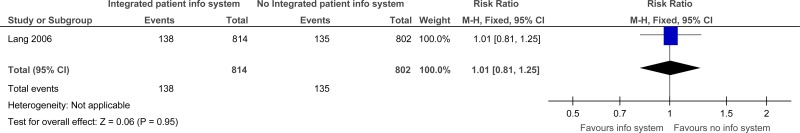
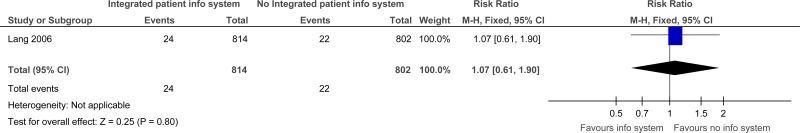
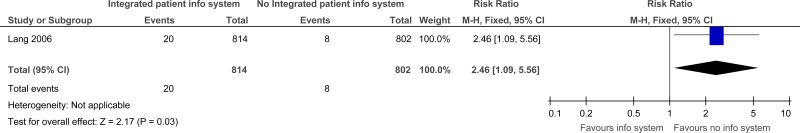
Evidence from these studies is summarised in the clinical evidence summary below (Table 3). See also the study selection flow chart in Appendix B, forest plots in Appendix C, study evidence tables in Appendix D, GRADE tables in Appendix E and excluded studies list in Appendix F.
Table 3
Clinical evidence summary: Integrated patient information systems versus no integrated patient information systems.
33.4. Economic evidence
Published literature
No relevant health economic studies were identified.
The economic article selection protocol and flow chart for the whole guideline can found in the guideline’s Appendix 41A and Appendix 41B.
In the absence of health economic evidence, unit costs were presented to the guideline committee – see Chapter 41 Appendix I.
33.5. Evidence statements
Clinical
One study comprising 1616 participants evaluated integrated patient information system for improving outcomes in secondary care in adults and young people at risk of an AME, or with a suspected or confirmed AME. The evidence for integrated patient information systems suggested there was no difference for repeat visits to the ED within 28 days (moderate quality) or duplication of diagnostic tests between ED and the family physician (very low). However, the evidence for integrated patient information systems suggested there was a possible increase of repeat visits to the ED within 14 days (low quality) and duplication of diagnostic tests in speciality consultations (low quality) compared to no integrated patient information systems.
Economic
No relevant economic evaluations were identified.
33.6. Recommendations and link to evidence
References
- 1.
- Akbarov A, Williams R, Brown B, Mamas M, Peek N, Buchan I et al. A two-stage dynamic model to enable updating of clinical risk prediction from longitudinal health record data: illustrated with kidney function. Studies in Health Technology and Informatics. 2015; 216:696–700 [PubMed: 26262141]
- 2.
- Aubin M, Vezina L, Verreault R, Fillion L, Hudon E, Lehmann F et al. Patient, primary care physician and specialist expectations of primary care physician involvement in cancer care. Journal of General Internal Medicine. 2012; 27(1):8–15 [PMC free article: PMC3250542] [PubMed: 21751057]
- 3.
- Cifuentes M, Davis M, Fernald D, Gunn R, Dickinson P, Cohen DJ. Electronic health record challenges, workarounds, and solutions observed in practices integrating behavioral health and primary care. Journal of the American Board of Family Medicine. 2015; 28: Suppl 1:S63–S72 [PMC free article: PMC7304941] [PubMed: 26359473]
- 4.
- Cox CE, Curtis JR. Using technology to create a more humanistic approach to integrating palliative care into the intensive care unit. American Journal of Respiratory and Critical Care Medicine. 2016; 193(3):242–250 [PubMed: 26599829]
- 5.
- Department of Health. Information: to share or not to share? The Information Governance Review, 2013. Available from: https://www
.gov.uk/government /uploads/system /uploads/attachment_data /file/192572 /2900774_InfoGovernance_accv2.pdf - 6.
- Flemming D, Hubner U. How to improve change of shift handovers and collaborative grounding and what role does the electronic patient record system play? Results of a systematic literature review. International Journal of Medical Informatics. 2013; 82(7):580–592 [PubMed: 23628146]
- 7.
- Lang E, Afilalo M, Vandal AC, Boivin JF, Xue X, Colacone A et al. Impact of an electronic link between the emergency department and family physicians: a randomized controlled trial. CMAJ Canadian Medical Association Journal. 2006; 174(3):313–318 [PMC free article: PMC1373712] [PubMed: 16399880]
- 8.
- Moore P, Armitage G, Wright J, Dobrzanski S, Ansari N, Hammond I et al. Medicines reconciliation using a shared electronic health care record. Journal of Patient Safety. 2011; 7(3):148–154 [PubMed: 21857238]
- 9.
- Overhage JM, Dexter PR, Perkins SM, Cordell WH, McGoff J, McGrath R et al. A randomized, controlled trial of clinical information shared from another institution. Annals of Emergency Medicine. 2002; 39(1):14–23 [PubMed: 11782726]
- 10.
- Sicotte C, Lapointe J, Clavel S, Fortin M-A. Benefits of improving processes in cancer care with a care pathway-based electronic medical record. Practical Radiation Oncology. 2016; 6(1):26–33 [PubMed: 26598908]
- 11.
- Van Eaton EG, Horvath KD, Lober WB, Rossini AJ, Pellegrini CA. A randomized, controlled trial evaluating the impact of a computerized rounding and sign-out system on continuity of care and resident work hours. Journal of the American College of Surgeons. 2005; 200(4):538–545 [PubMed: 15804467]
Appendices
Appendix A. Review protocol
Table 4
Review protocol: Integrated Patient Information Systems.
Appendix B. Clinical article selection
Appendix C. Forest plots
C.1. Integrated patient information systems versus No Integrated patient information systems
Appendix D. Clinical evidence tables
Download PDF (301K)
Appendix E. GRADE tables
Table 5
Clinical evidence profile: Integrated Patient Information Systems versus no Integrated Patient Information Systems.
Appendix F. Excluded clinical studies
Table 6
Studies excluded from the clinical review.
Publication Details
Copyright
Publisher
National Institute for Health and Care Excellence (NICE), London
NLM Citation
National Guideline Centre (UK). Emergency and acute medical care in over 16s: service delivery and organisation. London: National Institute for Health and Care Excellence (NICE); 2018 Mar. (NICE Guideline, No. 94.) Chapter 33, Integrated patient information systems.