NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
Feingold KR, Anawalt B, Blackman MR, et al., editors. Endotext [Internet]. South Dartmouth (MA): MDText.com, Inc.; 2000-.
ABSTRACT
Empty sella is a radiological finding of a flattened pituitary in a sellar space filled with cerebrospinal fluid. It may be primary or secondary consequent to various processes causing injury and shrinkage of the pituitary gland (postpartum hemorrhage, pituitary surgery, irradiation, apoplexy, infection, head trauma, hypophysitis, etc.). The mechanisms involved in the pathogenesis of the so called “primary empty sella” may range from continuously or intermittently increased intracranial pressure due to idiopathic benign intracranial hypertension, obesity, arterial hypertension, or multiple pregnancies in female patients with accompanying insufficiency of the sellar diaphragm and changes in pituitary gland volume (hyperplasia during pregnancy, lactation, menopause etc.). Primary empty sella can be an incidental radiological finding in an asymptomatic patient with preserved pituitary function. In symptomatic patients with the so called “empty sella syndrome” (headache, visual disturbances and hormonal dysfunction), the radiological finding of an empty sella is important in the differential diagnosis of other sellar lesions. Hypopituitarism, partial or complete, and hyperprolactinemia are not uncommon in these patients. The treatment of hypopituitarism and hyperprolactinemia is advocated in all patients with confirmatory results. In patients with the secondary empty sella, hypopituitarism is more common and more readily recognized due to damage caused by surgery, radiation therapy, or various pathological causes. Rarely, empty sella can be associated with hormonal hypersecretion from an “invisible” micro adenoma producing prolactin, growth hormone (acromegaly) or ACTH (Cushing’s disease). A wide range of radiological findings in patients with secondary and primary empty sella coupled with clinical data (important hints from the history and data on endocrine function) are presented for further illustration of this topic. For complete coverage of all related areas of Endocrinology, please visit our on-line FREE web-text, WWW.ENDOTEXT.ORG.
HISTORY
The term ‘empty sella’ was first used by Bush in 1951 (1) to describe a peculiar anatomical condition, observed in 40 of 788 human cadavers, particularly females, characterized by a sella turcica with an incomplete diaphragm sellae that forms only a small peripheral rim, with a pituitary gland not absent, but flattened in such a manner as to form a thin layer of tissue at the bottom of the sella turcica. Kaufman (2), in 1968, speculated that ‘…empty sella is a distinct anatomical and radiographic entity, function of an incompleteness of the diaphragma sellae and of the cerebrospinal fluid (CSF) pressure, normal or elevated’. The role of the normal fluctuations of CSF pressures and the effect of a superimposed prolonged increase in CSF pressure were related to the anatomic changes involving the bony wall of the empty sella.
DEFINITION, ETIOLOGY, AND PREVALENCE OF EMPTY SELLA
Empty sella is defined as herniation of subarachnoid space into the sella turcica (arachnoidocele). It is a term for the radiological finding of “empty sellar space” on magnetic resonance imaging (MRI) and computerized tomography (CT) with a flattened pituitary and elongated stalk. It can be partial if less than 50% of sellar space is filled with cerebro-spinal fluid (CSF), or complete if CSF fills more than 50% of space in the sella and gland thickness is less than 2mm (3,4).
Regarding its etiology, it can be primary if there is no pathological process in the sellar region preceding the pituitary damage or secondary if it is consequent to a specific pathological process. Primary empty sella (PES) can be an incidental finding or may arise during imaging for headache, endocrine disorders, neurological symptoms, visual disturbances, abnormal sella turcica radiograph, and other reasons.
Primary empty sella (PES) can be caused by intracranial hypertension and/or insufficiency of the sellar diaphragm in subjects with no previous history of pituitary disease. Insufficiency of the sellar diaphragm, a deflection of dura matter separating the suprasellar cistern from the pituitary fossa, allows unobstructed pulsatile movements of CSF from chiasmatic cistern causing flattening of the pituitary to the sellar floor. In extreme cases bone erosion of the sellar floor and CSF leak (rhinorrhea) may occur, increasing the risk of meningitis. Partial or complete absence of the sellar diaphragm has been demonstrated in patients with PES.
Intracranial pressure can be intermittently increased due to obesity, sleep apnea, arterial hypertension, pregnancy, and labor. Intracranial hypertension may be idiopathic or associated with other intracranial processes such as tumors, venous thrombosis, infections, or malformations. Idiopathic intracranial hypertension (IIH) or “pseudo-tumor cerebri” is a rare condition affecting 1 in 100,000 persons. It can be due to impaired CSF absorption, increased CSF secretion and/or increased capillary permeability (5). Impaired CSF dynamics and absorption have been found in up to 77% and 84% of patients with PES, respectively (6), The prevalence of PES is very high in patients with IIH ranging from 70-94% (4).
Changes in the pituitary gland volume may also be involved in the pathogenesis of empty sella syndrome including hyperplasia during pregnancy and lactation and pituitary involution after menopause accounting for the significantly higher prevalence of this condition in female patients (female to male ratio 5:1).
Factors involved in the pathogenesis of primary empty sella are shown in Figure 1.
Secondary empty sella is more common and is related to various pathological processes of the sellar region. Among many causes of pituitary tumor shrinkage occurring after medical treatment, surgery, radiotherapy, and apoplexy of a pituitary adenoma are frequent causes of secondary empty sella. Likewise, postpartum pituitary necrosis, pituitary infection, hypophysitis, and traumatic brain injury may lead to pituitary atrophy. The diagnosis of secondary empty sella is more difficult if there is no known underlying pathology involving the pituitary gland. In these cases, the sella is normal in size, and the function of the flattened pituitary gland may or may not be compromised. Such is the case in congenital causes of hypopituitarism both acquired and genetic, presenting with a hypoplastic pituitary gland and ectopic posterior lobe. Large intracranial tumors such as slow-growing meningiomas can also cause increased intracranial pressure and secondary empty sella in a significant number of patients. Pituitary MRI images of patients with secondary and primary empty sella are presented in the section dedicated to radiological appearance of an empty sella (Fig. 2-6). Associated risk factors for primary and secondary empty sella are shown in Table 1.
The reported prevalence of empty sella depends on techniques used for detection. In autopsy studies empty sella has been found in up to 5.5-12% cases (1,2), On imaging the overall incidence has been estimated at 12% (4). The prevalence of PES is very high in patients with IIH.
Table 1.
Associated Risk Factors for Primary and Secondary Empty Sella
| Primary Empty Sella (PES) | Secondary Empty Sella (SES) |
|---|---|
| Female sex Multiple pregnancies Obesity and sleep apnea Arterial hypertension Benign intracranial hypertension | Medical therapy Pituitary surgery Irradiation Pituitary apoplexy Sheehan’s syndrome Traumatic brain injury Congenital hypopituitarism |
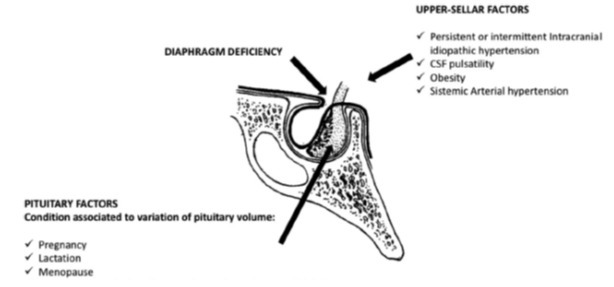
Figure 1.
Factors involved in pathogenesis of primary empty sella including the upper-sellar factors, incompetence or incomplete formation of the sellar diaphragm, and pituitary factors associated with the variation in the pituitary volume. Modified from Bioscientifica Ltd., Chiloiro S et al, European Journal of Endocrinology (2017) 177, R275–R285
RADIOLOGICAL APPEARANCE OF EMPTY SELLA
Most commonly an empty sella is incidentally discovered during MRI or CT imaging or during evaluation for headache, endocrine, neurological or visual disturbances. Less commonly it is observed after additional imaging for abnormal sella turcica radiographs. Chronic intracranial hypertension can lead to sellar remodeling and enlargement with thinning of the sellar floor and rarely rhinorrhea.
On typical presentation CSF filling is in continuity with overlying subarachnoid spaces and the residual pituitary gland is flattened against the sellar floor of enlarged bony sella with pituitary volume usually less than 611.21 mm3 (7). The differential diagnosis with cystic lesions and congenital pituitary abnormalities may pose a challenge. The stalk is usually thinned and located in the midline. Asymmetry is a frequent sign of the secondary empty sella. In rare cases the chiasm can herniate into the sella in cases of both primary and secondary etiology. Indirect signs of intracranial hypertension may also be present such as flattening of the posterior sclera, prominent subarachnoid spaces along the optic nerves, vertical tortuosity of the optic nerve sheath complex, and increased width of the optic nerve sheaths (8).
Sagittal and coronal T1-weighted (T1W) contrast enhanced images and coronal T2-weighted (T2W) images are strongly indicated for MR studies because they show CSF within the sella. On FLAIR sequences the intrasellar fluid completely suppresses and it presents without restriction in DWI sequences. After contrast T1W images show normal enhancement of residual pituitary gland and the stalk in PES in contrast to scaring and distortion in SES.
In patients with congenital hypopituitarism an ectopic posterior pituitary, stalk duplication or absence may be present in combination with other midline defect (agenesis of corpus callosum, supraoptic dysplasia, etc.).
Figures 2, 3, 4, 5 represent various MRI findings of patients with secondary empty sella due to postpartum hemorrhage (Sheehan’s syndrome Fig. 2), lymphocytic hypophysitis (Fig. 3), shrinkage of a macroprolactinoma after successful treatment with cabergoline (Fig.4), and congenital hypopituitarism with empty sella (Fig.5)
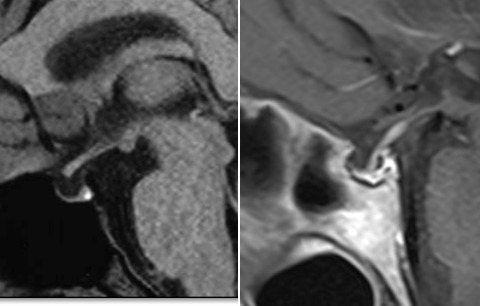
Figure 2.
Sagittal T1W images of two patients with empty sella and Sheehan’s syndrome
Left Panel (sagittal T1W image without contrast) and Right (sagittal T1W image after contrast enhancement) represent the MRI appearance of empty sella in two patients with Sheehan’s syndrome. Both patients presented with hyponatremic coma due to unrecognized panhypopituitarism and infection 3 and 20 years after delivery complicated by postpartum hemorrhage.
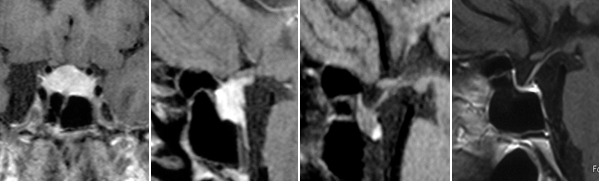
Figure 3.
Contrast enhanced coronal and sagittal T1W images of lymphocytic hypophysitis spontaneous evolution from the presentation (panel A, B), after 4 (panel C) and 10 years (panel D) of follow-up resulting in secondary empty sella.
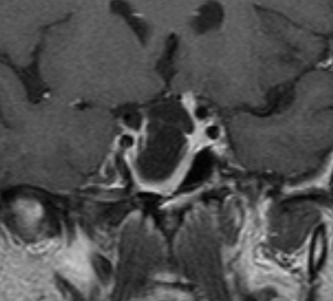
Figure 4.
Coronal T1W images demonstrating a pituitary tumor (macroprolactinoma) shrinkage in a patient treated with the dopamine agonist cabergoline for 10 years. The patient presented with hyperprolactinemia causing galactorrhea-amenorrhea, secondary adrenal insufficiency and central hypothyroidism. Hyperprolactinemia and adrenal insufficiency completely recovered during follow up.
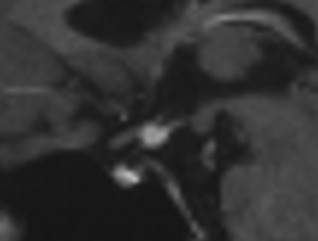
Figure 5.
Sagittal T1W showing small pituitary gland found at the bottom of sella, thin stalk and ectopic posterior lobe in a young adult with isolated childhood-onset growth hormone deficiency (congenital).
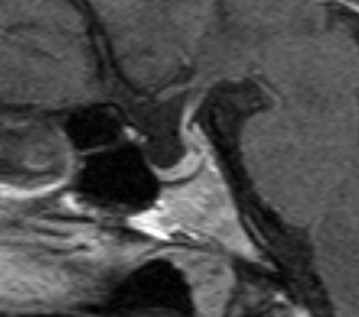
Figure 6.
Sagittal T1W images of pituitary stalk pressed against the dorsum sellae causing mild hyperprolactinemia in a patient with primary empty sella.
PRIMARY EMPTY SELLA (PES) AND EMPTY SELLA SYNDROME
Epidemiologically, this is associated with female sex (female to male ratio 5:1), multiple pregnancies, obesity, arterial hypertension and middle age. It may present with headaches, endocrine dysfunction, and visual disturbances due to pressure on the neighboring structures.
A typical clinical picture consists of headache and obesity. Women in the reproductive age may be affected by menstrual irregularities, galactorrhea and sterility. Man can develop gynecomastia and sexual disturbances. Primary empty sella due to the syndrome of increased intracranial pressure can also be associated with symptoms of intracranial hypertension.
Pathogenesis of Primary Empty Sella (PES)
Pregnancy may trigger the onset of PES. It is associated with pituitary hyperplasia and CSF hypertension especially in multiple pregnancies. PES has also been associated with CSF hypertension related to obesity and arterial hypertension. In the largest study with 175 patients, multiple pregnancies were reported in 58.3% women with PES, while obesity and arterial hypertension were recorded in 49.5% and 27.3% of patients (8). In patients with benign intracranial hypertension, empty sella is a common finding.
Endocrine Dysfunction in PES
Hyperprolactinemia, usually mild (less than 50 ng/ml), is present in approximately 10% of patients (8). It is often due to increased pressure of the CSF on the pituitary stalk and diminished dopamine inhibitory effect. Prolactin dynamics in PES may be influenced by gonadal status, intracranial pressure, neurotransmitters, and stalk integrity. Rarely, pituitary microadenomas causing acromegaly and Cushing’s disease may be associated with empty sella. In the recent study by Himes et al. empty sella was associated with an increased rate of MRI negative Cushing’s disease (9). Pituitary compression causing a relative reduction in the volume of the pituitary for imaging is a plausible cause for not detecting the tumor mass with MRI (9).
The prevalence of hypopituitarism in patients with PES is variable. In a study by Guitelman et al. it was found in 28% of patients (9,10). Panhypopituitarism was present in 40% of these patients, while partial or isolated hormone deficiencies were diagnosed in 60% of hypopituitary patients (10). The most prevalent pituitary deficiency was growth hormone deficiency.
In a pooled meta-analysis, which included 4 studies, the frequency of hypopituitarism was 52% (11). Multiple pituitary hormone deficiencies were present in 30%, isolated in 21% of patients with PES. Growth hormone and the gonadotropins were most common isolated insufficiencies (11).
In the recent retrospective single-center study of 765 patients by Ekhzaimy et al. 79% of PES was diagnosed incidentally on MRI. The majority of patients were evaluated by general practitioners with suboptimal hormonal evaluation while only 20% were referred to endocrinologists for hormonal evaluation (12).
Hormonal assessment is advocated in all patients with ES. In case of borderline results or suspected isolated or partial insufficiency stimulatory tests are recommended if clinically relevant for hormone replacement.
Other symptoms in patients with ES include: headache, visual and neurological disturbances. In patients with intracranial hypertension these symptoms are more common.
Neurological and Ophthalmic Dysfunction in PES
Headache is present in approximately 80% (3,6). In 20% of patients it may be accompanied by visual disturbances, even papilledema in intracranial hypertension (3,6).
Visual disturbances including worsening of visual acuity, blurred vision, diplopia, defects of oculomotor nerve, and optical neuritis were also reported in patients with PES. In case of benign intracranial hypertension ophthalmic echography and computerized visual field with evoked potentials should be performed in consultation with ophthalmologists. In case of chiasmal herniation into the empty sella with acute visual deterioration, new neurosurgical techniques of chiasmal transsphenoidal elevation are available (13, 14).
Study by Yilmaz et al. evaluated retinal optic nerve fiber thickness by optic coherence tomography in asymptomatic patients with empty sella and healthy controls (14, 16). Reduced values in asymptomatic patients provide valuable data for monitoring of these patients (15).
Neurological disturbances: dizziness, syncope, cranial nerve disorders, convulsions and depression were reported in approximately 40%of patients with PES (3, 6). Rhinorrhea imposes the risk of meningitis.
TREATMENT
In patients with increased idiopathic intracranial pressure osmotic diuretics or acetazolamide (Diamox) are advocated. Weight loss may be efficient in obese and overweight patients especially if accompanied by sleep apnea. Neurosurgical techniques may be indicated for rhinorrhea and some symptomatic secondary causes of empty sella syndrome with increased intracranial pressure and acute visual disturbances. If diagnosed hypopituitarism should be replaced following the current recommendations (16) and hyperprolactinemia treated with dopamine agonists.
CONCLUSION
Primary empty sella can be heterogeneous in origin and presentations range from an asymptomatic incidental radiological finding to endocrine and neuro-ophthalmological manifestations. Female sex, multiple pregnancies, obesity, and arterial hypertension are associated risk factors as well as the syndrome of benign intracranial hypertension. Secondary empty sella is caused by various pathological processes resulting in shrinkage of the pituitary gland. Routine hormonal status assessment and regular follow-up are indicated in all patients since the prevalence of pituitary dysfunction is significant.
REFERENCES
- 1.
- Busch W. Die Morphologie der Sella turcica und ihre Beziehungen zur Hypophyse. Virchows Archiv für Pathologische Anatomie und Physiologie und für klinische Medizin. 1951;320:437–458. [PubMed: 14942993]
- 2.
- Kaufman B. The ‘empty’ sella turcica-a manifestation of the intrasellar subarachnoid space. Radiology. 1968;90:931–941. [PubMed: 5300448]
- 3.
- De Marinis L, Bonadonna S, Bianchi A, Giulio M, Gustina A. Extensive clinical experience: primary empty sella. Journal of Clinical Endocrinology and Metabolism. 2005:5471–5477. [PubMed: 15972577]
- 4.
- Chiloiro S, Giampietro A., Bianchi A, Tartaglione T, Capobianco A, Anile C, De Marinis L. Primary empty sella: a comprehensive review. European Journal of Endocrinology. 2017;177(6):R275–R285. [PubMed: 28780516]
- 5.
- Friedman DI, Jacobson DM. Diagnostic criteria for idiopathic intracranial hypertension. Neurology. 2002;59:1492–1495. [PubMed: 12455560]
- 6.
- Maira G, Anile C, Mangiola A. Primary empty sella syndrome in a series of 142 patients. Journal of Neurosurery. 2005;103:831–836. [PubMed: 16304986]
- 7.
- Hoffmann J, Schmidt C, Kunte H, Klingebiel R, Harms L, Huppertz HJ, Lüdemann L, Wiener E. Volumetric assessment of optic nerve sheath and hypophysis in idiopathic intracranial hypertension. American Journal of Neuroradiology. 2014;35:513–518. [PMC free article: PMC7964733] [PubMed: 24029390]
- 8.
- Degnan AJ, Levy LM. Pseudotumor cerebri: brief review of clinical syndrome and imaging findings. American Journal of Neuroradiology. 2012 [PMC free article: PMC7964411] [PubMed: 21680652] [CrossRef]
- 9.
- Himes BT, Bhargav AG, Brown DA, Kaufmann TJ, Bancos I, Van Gompel JJ. Does pituitary compression/empty sella syndrome contribute to MRI-negative Cushing's disease? A single-institution experience. Neurosurg Focus. 2020 Jun;48(6):E3. doiPMID. [PubMed: 32480375] [CrossRef]
- 10.
- Guitelman M, Basalvibaso NG, Vitale M, Chervin A, Katz D, Miragaya K, Herrera J, Cornalo D, Servido M, Boero L, Manavela M, Danilowicz K, Alfieri A, Stalldecker G, Glerean M, Fainstein Day P, Ballarino C, Mallea Gil MS, Rogozinski A. Primary empty sella (PES): a review of 175 cases. Pituitary. 2013;16:270–274. [PubMed: 22875743]
- 11.
- Auer MK, Stieg MR, Crispin A, Sievers C, Stalla GK, Kopczak A. Primary empty sella syndrome and the prevalence of hormonal dysregulation. DeutschesArtzteblattInternational. 2018;115:99–105. [PMC free article: PMC5842341] [PubMed: 29510819]
- 12.
- Ekhzaimy AA, Mujammami M, Tharkar S, Alansary MA, Al Otaibi D. Clinical presentation, evaluation and case management of primary empty sella syndrome: a retrospective analysis of 10-year single-center patient data. BMC Endocr Disord. 2020 Sep 17;20(1):142. doiPMIDPMCID: PMC7495892. [PMC free article: PMC7495892] [PubMed: 32943019] [CrossRef]
- 13.
- Barzaghi LR, Donofrio CA, Panni P, Losa M, Mortini P. Treatment of empty sella associated with visual impairment: a systematic review of chiasmapexy techniques. Pituitary. 2018 Feb;21(1):98–106. doiReview. [PubMed: 29027644] [CrossRef]
- 14.
- Guinto G, Nettel B, Hernández E, Gallardo D, Aréchiga N, Mercado M. Osseous Remodeling Technique of the Sella Turcica: A New Surgical Option for Primary Empty Sella Syndrome. World Neurosurg. 2019 Jun;126:e953–e958. Epub 2019 Mar 12. PMID. [PubMed: 30877013] [CrossRef]
- 15.
- Yilmaz A, Gok M, Altas H, Yildirim T, Kaygisiz S, Isik HS. Retinal nerve fibre and ganglion cell inner plexiform layer analysis by optical coherence tomography in asymptomatic empty sella patients. Int J Neurosci. 2020 Jan;130(1):45–51. Epub 2019 Sep 13. PMID. [PubMed: 31462116] [CrossRef]
- 16.
- Flesseriu M, Hashim IA, Karavitaki N, Melmed S, Murad MH, Salvatori R, Samuels MH. Hormonal replacement in hypoituitarism in adults: an endocrine society clinical practice guideline. Journal of Clinical Endocrinology and metabolism. 2016;101:3888–3921. [PubMed: 27736313]
- Review Empty sella syndrome: Multiple endocrine disorders.[Handb Clin Neurol. 2021]Review Empty sella syndrome: Multiple endocrine disorders.Chiloiro S, Giampietro A, Bianchi A, De Marinis L. Handb Clin Neurol. 2021; 181:29-40.
- Review The empty sella. A reappraisal of etiology and pathogenesis.[Acta Neurol Scand Suppl. 1990]Review The empty sella. A reappraisal of etiology and pathogenesis.Bjerre P. Acta Neurol Scand Suppl. 1990; 130:1-25.
- Does pituitary compression/empty sella syndrome contribute to MRI-negative Cushing's disease? A single-institution experience.[Neurosurg Focus. 2020]Does pituitary compression/empty sella syndrome contribute to MRI-negative Cushing's disease? A single-institution experience.Himes BT, Bhargav AG, Brown DA, Kaufmann TJ, Bancos I, Van Gompel JJ. Neurosurg Focus. 2020 Jun; 48(6):E3.
- Review [The empty sella syndrome. Clinical, radiological and endocrinologic analysis in 20 cases].[Minerva Endocrinol. 1989]Review [The empty sella syndrome. Clinical, radiological and endocrinologic analysis in 20 cases].Degli Uberti EC, Teodori V, Trasforini G, Tamarozzi R, Margutti A, Bianconi M, Rossi R, Ambrosio MR, Pansini R. Minerva Endocrinol. 1989 Jan-Mar; 14(1):1-18.
- Effect of primary empty sella syndrome on pituitary surgery for Cushing's disease.[J Neurosurg. 2014]Effect of primary empty sella syndrome on pituitary surgery for Cushing's disease.Mehta GU, Bakhtian KD, Oldfield EH. J Neurosurg. 2014 Sep; 121(3):518-26. Epub 2014 May 23.
- Empty Sella - EndotextEmpty Sella - Endotext
Your browsing activity is empty.
Activity recording is turned off.
See more...
