NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
National Guideline Centre (UK). Emergency and acute medical care in over 16s: service delivery and organisation. London: National Institute for Health and Care Excellence (NICE); 2018 Mar. (NICE Guideline, No. 94.)

Emergency and acute medical care in over 16s: service delivery and organisation.
Show details14. Community palliative care
14.1. Introduction
Acute medical illness can present at the end of life and contribute to significant distress in patients, their families and their carers. Care models should be able to assess, treat and support patients with an acute medical illness at the end of life in the setting chosen by patients, which could include home, care home, hospice or hospital.
There is some uncertainty over the clinical and cost-effectiveness of different models of community based palliative care, which can support management of acute medical illnesses at the end of life outside hospices and hospitals. This is important to determine as it offers choice to patients and carers at a crucial time of life.
14.2. Review question: Does community-based palliative care improve outcomes compared with hospital care?
For full details see review protocol in Appendix A.
Table 1
PICO characteristics of review question.
14.3. Clinical evidence
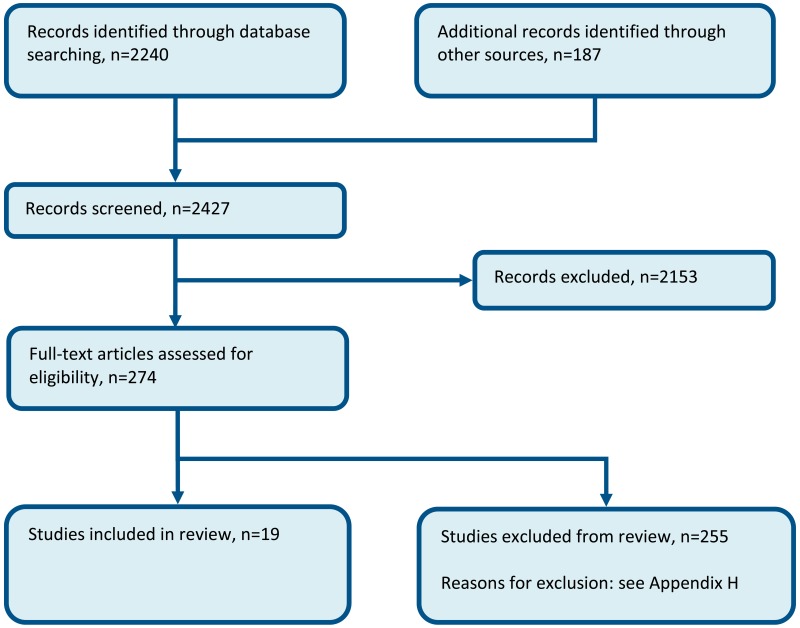
Nineteen studies were included in the review: 3 Cochrane reviews106,242,279 and 16 individual RCTs;5,18–20,35,40,110,111,132,136,147,177,210,263,280,290,291 these are summarised in Table 2 below. One study (out of 9) from the Cochrane review 278, all 4 studies from the Cochrane review 242 and 8 studies (out of 23) from the Cochrane review106 were included in our evidence review. Other studies from the Cochrane reviews were not included as they did not fit in our protocol criteria for study design, population, or interventions. Evidence from these studies is summarised in the GRADE clinical evidence profile below (Table 3 and Table 4). See also the study selection flow chart in Appendix B, study evidence tables in Appendix D, forest plots in Appendix C, GRADE tables in Appendix F and excluded studies list in Appendix G.
Table 2
Summary of studies included in the review.
Table 3
Clinical evidence profile: Community palliative care versus hospital palliative care.
Table 4
Clinical evidence summary: Enhanced community palliative care versus standard community palliative care.
We searched for randomised controlled trials comparing the effectiveness of the interventions listed in the protocol. Fifteen randomised controlled trials were identified:
- Life expectancy of patients included varied among the included studies from a few months, to as much as 2 years.
- Cancer, chronic heart failure and chronic obstructive pulmonary disease were the main diagnoses among those included.
Narrative findings
One study Hughes, 1992135 reported that roughly 50% of patients in each group died in hospital. The same study also reported that at 1 month, carers in the treatment group had a greater level of satisfaction compared to carers in the control group (p=0.005). At 6 month follow-up there was no difference in satisfaction anymore.
Table 5
Clinical evidence summary: Community based palliative care versus usual care.
14.4. Economic evidence
Published literature
Two economic evaluations were identified with the relevant comparison and have been included in this review.130,227 These are summarised in the economic evidence profile below (Table 6) and the economic evidence tables in Appendix E.
Table 6
Economic evidence profile: community-based palliative care versus usual care.
Four economic evaluations relating to this review question were excluded on the grounds of applicability, quality and the availability of more relevant evidence. The reasons summarised in Appendix H.
The economic article selection protocol and flow chart for the whole guideline can found in the guideline’s Appendix 41A and Appendix 41B.
14.5. Evidence statements
Clinical
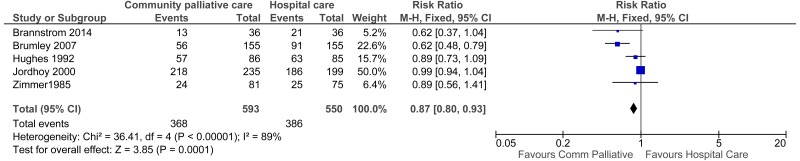
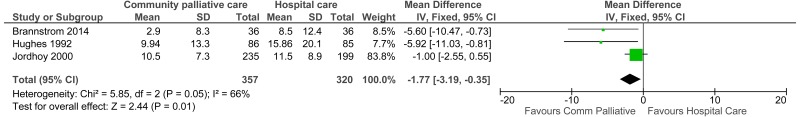
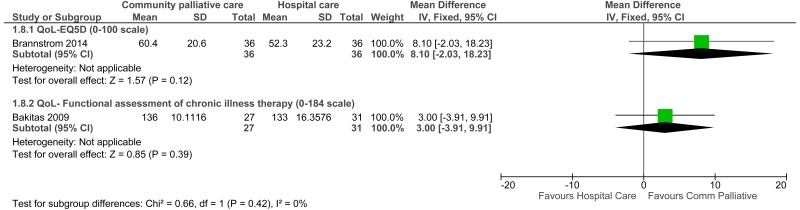
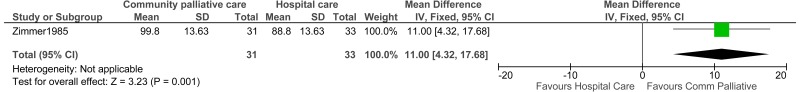
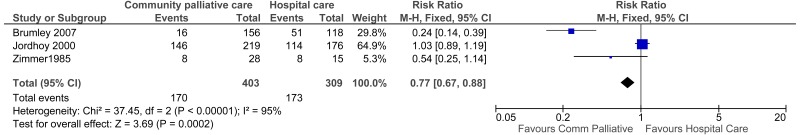
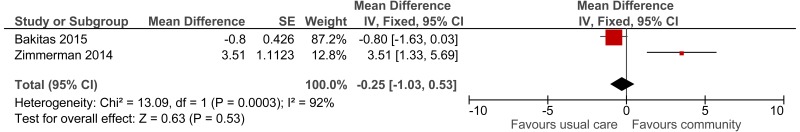
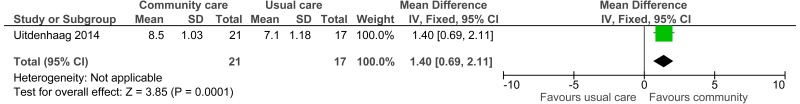
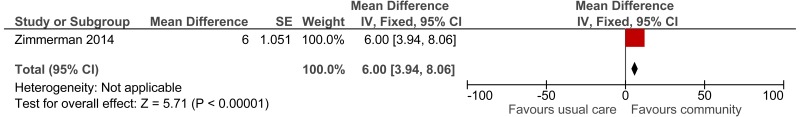
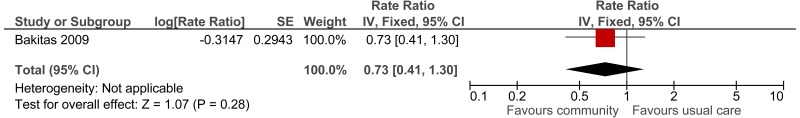
Seven studies comprising 1493 people evaluated the role of community based palliative care versus hospital based palliative care for improving outcomes in adults and young people at risk of an AME, or with a suspected or confirmed AME. The evidence suggested that community based palliative care may provide benefit in increased number of people in which home was the place of death (5 studies, low quality), decreased number of people in which hospital was the place of death (3 studies, very low quality), decreased the number of presentations to the ED (1 study, low quality) and improved patient and/or carer satisfaction (3 studies reported separately, low quality). However, the evidence suggested no difference on the number of hospital admissions (5 studies, very low quality), length of hospital stay (4 studies, low quality), mean number of ED visits (1 study, moderate quality) or quality of life (2 studies reporting different scores, low quality).
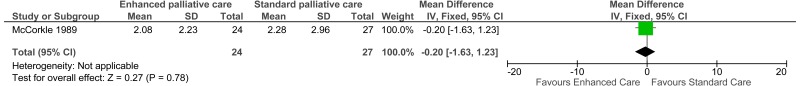
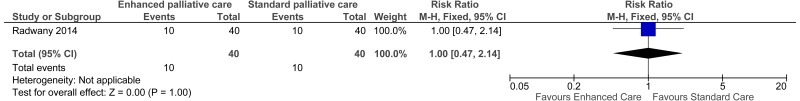
Five studies comprising 1404 people evaluated the role of enhanced community based palliative care versus standard community based palliative care for improving outcomes in adults and young people at risk of an AME, or with a suspected or confirmed AME. The evidence suggested that enhanced community based palliative care has no effect on number of hospital admissions (1 study, low quality), number of presentations to ED (1 study, low quality), length of hospital stay (1 study, very low quality) or quality of life (1 study, low quality). One study suggested there was no difference in place of death (1 study, moderate quality) while another study suggested an increase in the number of people achieving their preferred place of death (1 study, low quality).
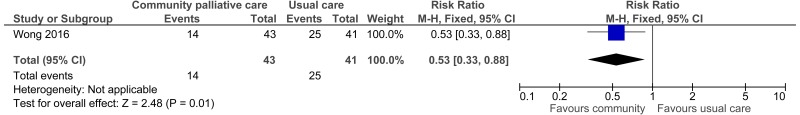
Four studies comprising 890 people evaluated the role of community based palliative care versus usual care for improving outcomes in adults and young people at risk of an AME, or with a suspected or confirmed AME. The evidence suggested that community based palliative care may provide benefit in increased number of people in which home was the place of death (1 study, very low quality), decreased the number of presentations to the ED (1 study, very low quality), improved patient and/or carer satisfaction (3 studies reporting different scores, very low to moderate quality), reduced length of hospital stay (1 study, very low quality) and reduced number of admissions (1 study, moderate quality) and readmissions to hospital (1 study, low quality). One study suggested there was a possible improvement in quality of life (low quality) while 2 other studies looking at different scores suggested no difference (moderate quality).
Economic
One cost-utility analysis found community-based specialist palliative care to dominate usual care, reducing costs and improving health outcomes. This evidence was assessed as partially applicable with potentially serious limitations.
One cost-effectiveness analysis found community-based specialist palliative care to reduce costs, however to also reduce quality of life, measured on the POS-8 scale. This evidence was assessed as partially applicable with minor limitations.
14.6. Recommendations and link to evidence
| Recommendations |
|
| Research recommendation | - |
| Relative values of different outcomes |
The guideline committee considered the following outcomes as critical: place of death, avoidable adverse events, quality of life, and patient and/or carer satisfaction. The following outcomes were identified as important to decision making: readmission, number of admissions to hospital, number of presentations to ED, number of presentations to GP and length of hospital stay. |
| Trade-off between benefits and harms |
The review was split into a comparison of community based palliative care versus hospital based palliative care, enhanced community based palliative care versus standard community based palliative care and community based palliative care versus usual care as defined by the studies (for example, comparators that included elements of both hospital and community care or comparators which were not well defined). A total of 16 randomised controlled trials were included in the review. Community palliative care versus hospital palliative care Seven studies comprising 1493 people evaluated the role of community based palliative care versus hospital based palliative care. The evidence suggested that community palliative care may provide benefit in increased number of people in which home was the place of death, decreased number of people in which hospital was the place of death, decreased number of presentations to ED and improved patient and/or carer satisfaction. The evidence suggested that there was no difference for the outcomes of number of hospital admissions, length of hospital stay, mean number of ED visits or quality of life. No evidence was found for the outcomes of avoidable adverse events, number of presentations to the GP and readmission. Enhanced versus standard community palliative care Five studies comprising 1404 people evaluated the role of enhanced community based palliative care versus standard community based palliative care. Enhanced palliative care is the provision of additional palliative care support care over and above the usual provision of community palliative care in the patient’s local healthcare system. The evidence suggested that enhanced community based palliative care has no effect on number of hospital admissions, number of presentations to ED, length of hospital stay or quality of life. One study suggested there was no difference in place of death while another study suggested an increase in the number of people achieving their preferred place of death. No evidence was found for the outcomes patient and/or carer satisfaction, readmission, number of presentations to GP and avoidable adverse events. Community based palliative care versus usual care Four studies comprising 890 people evaluated the role of community based palliative care versus usual as defined by the studies (for example, comparators that included elements of both hospital and community care or comparators which were not well defined). Usual care usually consisted of telephone or outpatient clinic follow up or a combination of both. The evidence suggested that community based palliative care may provide a benefit in increased number of people for whom home was the place of death, decreased number of presentations to the ED, improved patient and/or carer satisfaction, reduced length of hospital stay and reduced number of admissions and readmissions to hospital. One study suggested there was a possible improvement in quality of life while 2 other studies looking at different scores suggested no difference. No evidence was found for the outcomes avoidable adverse events or number of presentations to the GP. The committee emphasised that as far as possible the health system should respect patients’ wishes when planning palliative care at home or in a healthcare setting. Surveys of the public have consistently shown that home is the preferred place of death, and the provision of community palliative care would facilitate this. The committee also noted, however, that there would be occasions when managing the process of dying at home could be very difficult, and therefore alternative options should be retained. The committee agreed that community palliative care should be an option for all patients as an alternative to hospital admission. The service provided should incorporate staff with appropriate competencies to allow patients to be cared for in line with their preferences (for example, symptom management). No benefit was found for enhanced community based palliative over standard community palliative care and so this was not included in the recommendation. The reasons for this lack of benefit are unclear. It could be surmised that the interventions in both groups were very similar in terms of support at home except for intensity of support. Therefore, it is possible that more intensive input would only offer marginal gains, or none. |
| Trade-off between net effects and costs |
Two economic evaluations found community palliative care to be cost saving compared with usual care. One cost-effectiveness study found community palliative care to have a slightly poorer result on the palliative outcome-8 scale compared to usual care. However, the difference was small and not statistically significant whereas the evidence on the ‘Trade-off between benefits and harms’ above showed improvements in patient and/or carer satisfaction without evidence of adverse events. One cost-utility analysis found community palliative care improves health outcomes and reduces costs. The committee acknowledged the limitations, given it was conducted in a Swedish cohort and patient numbers were rather small. However, the committee noted the outcome of the study was largely in line with what was seen in other clinical studies presented in the clinical review. The evidence for patient and carer satisfaction evidence was in favour of community palliative care Although the economic evidence was not substantial it was based on data that largely coincided with the clinical evidence meaning it is unlikely that more economic evidence on this topic would change conclusions concerning cost effectiveness. The economic evidence identified would suggest there is a good chance community palliative care could reduce costs to the health service. The clinical evidence would suggest quality of life would remain unchanged or potentially improve therefore supporting the conclusion that it would be an effective use of NHS resources. |
| Quality of evidence |
For the comparison of community palliative care versus hospital palliative care the evidence for the outcome of number of presentations to ED (mean number of presentations) was of moderate quality due to risk of bias. The evidence for place of death, number of presentations to ED (number of visits), length of stay, quality of life and patient and/or carer satisfaction was low due to risk of bias, and inconsistency or imprecision. The evidence for number of hospital admissions was of very low quality due to risk of bias and inconsistency. For the comparison of enhanced versus standard community based palliative care, the evidence for the outcome of place of death (OR) was of moderate quality due to risk of bias. The evidence for the outcome of admissions, number of ED presentations, quality of life and place of death was of low quality due to risk of bias and imprecision. The quality of the evidence for length of stay was very low due to risk of bias and imprecision. For the comparison between community based palliative care and usual care, the evidence for quality of life and patient and/or carer satisfaction (FAMCARE scale) was of moderate quality due to inconsistency and imprecision. The evidence for patient and/or carer satisfaction (overall satisfaction) was of low quality due to risk of bias. The evidence for the outcomes of relatives’ satisfaction, place of death, length of stay and ED presentations was of very low quality due to risk of bias and imprecision. One cost-effectiveness analysis was assessed as partially applicable (no QALYs) with minor limitations. The other three economic evaluations were assessed as partially applicable (not UK and/or no QALYs) but with potentially serious limitations. |
| Other considerations |
Patient choice should always be considered in decision making, such as patient preference in terms of where they wish to die. Family and/or carer satisfaction and burden is also important when providing holistic palliative care. Ideally the service should follow the patient’s wishes if possible without increasing the burden on the family or carers. It is also important that the family or carers are supported and satisfied with the care provided. Healthcare professionals who are in contact with patients in the terminal phase of their life (for example, GPs, district nurses, hospital doctors and nurses) should be trained in the early identification of patients that might benefit from community based palliative care (see Linking Evidence to recommendation [LETR] in the Advanced Care Planning chapter [15]). Many people in the terminal phase of illness will have 1 or more AMEs at some point and are also likely to have more than 1 chronic long-term condition, which therefore gives the healthcare system ample opportunity to identify these patients to ensure that the focus is on managing the patient’s overall health status as well as optimising individual conditions (or their symptom management) independently. The committee noted that in the current service, the provision of community palliative care is variable and often not comprehensive. The service provided should be responsive to the patients’ needs and preferences, for example, provided 24 hours a day, 7 days a week (although no evidence was identified in relation to the timing of services). However, it is likely that a significant proportion of these patients’ deterioration will be out of the normal 9-5, Monday to Friday working hours. Healthcare professionals, particularly in secondary care, may be unaware of the availability of palliative care and other forms of support in the community. This could result in avoidable admission to, or delay in discharge from hospital. Early involvement of palliative care in hospital will ensure that patients receive the best balance between active treatment of underlying diseases and comorbidities while also ensuring effective symptom relief. Staff should be better trained in palliative care as current demographic changes will contribute to an increased demand for these specialised services. Pharmacists are a key component of the multidisciplinary community based palliative care service. As well as providing timely access to medicines they can advise on doses and combination of medicines. Recommendations on the management of people who are near the end of life can be found in the NICE clinical guideline on End of Life Care, currently in development (https://www |
References
- 1.
- Swing-beds meet patients needs and improve hospitals cash-flow. Hospitals. 1982; 56(13):39–40 [PubMed: 7084902]
- 2.
- Abernethy AP, Currow DC, Shelby-James T, Rowett D, May F, Samsa GP et al. Delivery strategies to optimize resource utilization and performance status for patients with advanced life-limiting illness: results from the “palliative care trial” [ISRCTN 81117481]. Journal of Pain and Symptom Management. 2013; 45(3):488–505 [PubMed: 23102711]
- 3.
- Addington-Hall JM, MacDonald LD, Anderson HR, Chamberlain J, Freeling P, Bland JM et al. Randomised controlled trial of effects of coordinating care for terminally ill cancer patients. BMJ. 1992; 305(6865):1317–1322 [PMC free article: PMC1883850] [PubMed: 1483075]
- 4.
- Adler MW, Waller JJ, Creese A, Thorne SC. Randomised controlled trial of early discharge for inguinal hernia and varicose veins. Journal of Epidemiology and Community Health. 1978; 32(2):136–142 [PMC free article: PMC1060932] [PubMed: 98548]
- 5.
- Aiken LS, Butner J, Lockhart CA, Volk-Craft BE, Hamilton G, Williams FG. Outcome evaluation of a randomized trial of the PhoenixCare intervention: program of case management and coordinated care for the seriously chronically ill. Journal of Palliative Medicine. 2006; 9(1):111–126 [PubMed: 16430351]
- 6.
- Aimonino N, Molaschi M, Salerno D, Roglia D, Rocco M, Fabris F. The home hospitalization of frail elderly patients with advanced dementia. Archives of Gerontology and Geriatrics. 2001; 7:19–23 [PubMed: 11431041]
- 7.
- Aimonino N, Salerno D, Roglia D, Molaschi M, Fabris F. The home hospitalization service of elderly patients with ischemic stroke: follow-up study. European Journal of Neurology. 2000; 7:(Suppl 3):111–112
- 8.
- Alcide A, Potocky M. Adult hospice social work intervention outcomes in the United States. Journal of Social Work in End-of-Life and Palliative Care. 2015; 11(3-4):367–385 [PubMed: 26654066]
- 9.
- Allen J. Surgical Internet at a glance: the Virtual Hospital. American Journal of Surgery. 1999; 178(1):1 [PubMed: 10456693]
- 10.
- Anderson C, Ni MC, Rubenach S, Clark M, Spencer C, Winsor A. Early supportive discharge and rehabilitation trial in stroke (ESPRIT). Royal Australasian College of Physicians Annual Scientific Meeting. 2000;16
- 11.
- Anderson C, Ni Mhurchu C, Brown PM, Carter K. Stroke rehabilitation services to accelerate hospital discharge and provide home-based care: an overview and cost analysis. Pharmacoeconomics. 2002; 20(8):537–552 [PubMed: 12109919]
- 12.
- Anderson DJ, Burrell AD, Bearne A. Cost associated with venous thromboembolism treatment in the community. Journal of Medical Economics. 2002; 5(1-10):1–10
- 13.
- Aoun SM, Grande G, Howting D, Deas K, Toye C, Troeung L et al. The impact of the carer support needs assessment tool (CSNAT) in community palliative care using a stepped wedge cluster trial. PloS One. 2015; 10(4):e0123012 [PMC free article: PMC4388632] [PubMed: 25849348]
- 14.
- Armstrong CD, Hogg WE, Lemelin J, Dahrouge S, Martin C, Viner GS et al. Home-based intermediate care program vs hospitalization: cost comparison study. Canadian Family Physician. 2008; 54(1):66–73 [PMC free article: PMC2293319] [PubMed: 18208958]
- 15.
- Aujesky D, Roy PM, Verschuren F, Righini M, Osterwalder J, Egloff M et al. Outpatient versus inpatient treatment for patients with acute pulmonary embolism: an international, open-label, randomised, non-inferiority trial. The Lancet. 2011; 378(9785):41–48 [PubMed: 21703676]
- 16.
- Bai M, Reynolds NR, McCorkle R. The promise of clinical interventions for hepatocellular carcinoma from the west to mainland China. Palliative and Supportive Care. 2013; 11(6):503–522 [PubMed: 23398641]
- 17.
- Baidoobonso S. Patient care planning discussions for patients at the end of life: an evidence-based analysis. Ontario Health Technology Assessment Series. 2014; 14(19):1–72 [PMC free article: PMC4561366] [PubMed: 26357528]
- 18.
- Bajwah S, Ross JR, Wells AU, Mohammed K, Oyebode C, Birring SS et al. Palliative care for patients with advanced fibrotic lung disease: a randomised controlled phase II and feasibility trial of a community case conference intervention. Thorax. 2015; 70(9):830–839 [PubMed: 26103995]
- 19.
- Bakitas M, Lyons KD, Hegel MT, Balan S, Brokaw FC, Seville J et al. Effects of a palliative care intervention on clinical outcomes in patients with advanced cancer: the Project ENABLE II randomized controlled trial. JAMA - Journal of the American Medical Association. 2009; 302(7):741–749 [PMC free article: PMC3657724] [PubMed: 19690306]
- 20.
- Bakitas MA, Tosteson TD, Li Z, Lyons KD, Hull JG, Li Z et al. Early versus delayed initiation of concurrent palliative oncology care: patient outcomes in the ENABLE III randomized controlled trial. Journal of Clinical Oncology. 2015; 33(13):1438–1445 [PMC free article: PMC4404422] [PubMed: 25800768]
- 21.
- Bakken MS, Ranhoff AH, Engeland A, Ruths S. Inappropriate prescribing for older people admitted to an intermediate-care nursing home unit and hospital wards. Scandinavian Journal of Primary Health Care. 2012; 30(3):169–175 [PMC free article: PMC3443941] [PubMed: 22830533]
- 22.
- Barnes MP. Community rehabilitation after stroke. Critical Reviews in Physical and Rehabilitation Medicine. 2003; 15(3-4):223–234
- 23.
- Beech R, Russell W, Little R, Sherlow-Jones S. An evaluation of a multidisciplinary team for intermediate care at home. International Journal of Integrated Care. 2004; 4:e02 [PMC free article: PMC1393274] [PubMed: 16773151]
- 24.
- Bernhaut J, Mackay K. Extended nursing roles in intermediate care: a cost-benefit evaluation. Nursing Times. 2002; 98(21):37–39 [PubMed: 12168441]
- 25.
- Bethell HJ, Mullee MA. A controlled trial of community based coronary rehabilitation. British Heart Journal. 1990; 64(6):370–375 [PMC free article: PMC1224812] [PubMed: 2271343]
- 26.
- Beynon JH, Padiachy D. The past and future of geriatric day hospitals. Reviews in Clinical Gerontology. 2009; 19(1):45–51
- 27.
- Blackburn GG, Foody JM, Sprecher DL, Park E, Apperson-Hansen C, Pashkow FJ. Cardiac rehabilitation participation patterns in a large, tertiary care center: evidence for selection bias. Journal of Cardiopulmonary Rehabilitation. 2000; 20(3):189–195 [PubMed: 10860201]
- 28.
- Blair J, Corrigall H, Angus NJ, Thompson DR, Leslie S. Home versus hospital-based cardiac rehabilitation: a systematic review. Rural and Remote Health. 2011; 11(2):1532 [PubMed: 21488706]
- 29.
- Board N, Brennan N, Caplan GA. A randomised controlled trial of the costs of hospital as compared with hospital in the home for acute medical patients. Australian and New Zealand Journal of Public Health. 2000; 24(3):305–311 [PubMed: 10937409]
- 30.
- Booth JE, Roberts JA, Flather M, Lamping DL, Mister R, Abdalla M et al. A trial of early discharge with homecare compared to conventional hospital care for patients undergoing coronary artery bypass grafting. Heart. 2004; 90(11):1344–1345 [PMC free article: PMC1768555] [PubMed: 15486143]
- 31.
- Boston NK, Boynton PM, Hood S. An inner city GP unit versus conventional care for elderly patients: prospective comparison of health functioning, use of services and patient satisfaction. Family Practice. 2001; 18(2):141–148 [PubMed: 11264263]
- 32.
- Bove DG, Lomborg K, Jensen AK, Overgaard D, Lindhardt BO, Midtgaard J. Efficacy of a minimal home-based psychoeducative intervention in patients with advanced COPD: a randomised controlled trial. Respiratory Medicine. 2016; 121:109–116 [PubMed: 27888984]
- 33.
- Bowman C, Black D. Intermediate not indeterminate care. Hospital Medicine. 1998; 59(11):877–879 [PubMed: 10197122]
- 34.
- Brandt A, Pilegaard MS, Oestergaard LG, Lindahl-Jacobsen L, Sorensen J, Johnsen AT et al. Effectiveness of the “Cancer Home-Life Intervention” on everyday activities and quality of life in people with advanced cancer living at home: a randomised controlled trial and an economic evaluation. BMC Palliative Care. 2016; 15(1):10 [PMC free article: PMC4724076] [PubMed: 26801394]
- 35.
- Brannstrom M, Boman K. Effects of person-centred and integrated chronic heart failure and palliative home care. PREFER: a randomized controlled study. European Journal of Heart Failure. 2014; 16(10):1142–1151 [PubMed: 25159126]
- 36.
- Brooks N. Intermediate care rapid assessment support service: an evaluation. British Journal of Community Nursing. 2002; 7(12):623–633 [PubMed: 12514491]
- 37.
- Brooks N, Ashton A, Hainsworth B. Pilot evaluation of an intermediate care scheme. Nursing Standard. 2003; 17(23):33–35 [PubMed: 12655764]
- 38.
- Brown L, Forster A, Young J, Crocker T, Benham A, Langhorne P et al. Medical day hospital care for older people versus alternative forms of care. Cochrane Database of Systematic Reviews. 2015; Issue 6:CD001730. DOI:10.1002/14651858.CD001730.pub3 [PMC free article: PMC7068157] [PubMed: 26102196] [CrossRef]
- 39.
- Brumley R, Enguidanos S, Jamison P, Seitz R, Morgenstern N, Saito S et al. Increased satisfaction with care and lower costs: results of a randomized trial of in-home palliative care. Journal of the American Geriatrics Society. 2007; 55(7):993–1000 [PubMed: 17608870]
- 40.
- Brumley RD, Enguidanos S, Cherin DA. Effectiveness of a home-based palliative care program for end-of-life. Journal of Palliative Medicine. 2003; 6(5):715–724 [PubMed: 14622451]
- 41.
- Brunner M, Skeat J, Morris ME. Outcomes of speech-language pathology following stroke: investigation of inpatient rehabilitation and rehabilitation in the home programs. International Journal of Speech-Language Pathology. 2008; 10(5):305–313 [PubMed: 20840030]
- 42.
- Bryan K. Policies for reducing delayed discharge from hospital. British Medical Bulletin. 2010; 95(1):33–46 [PubMed: 20647227]
- 43.
- Bryant-Lukosius D, Carter N, Reid K, Donald F, Martin-Misener R, Kilpatrick K et al. The clinical effectiveness and cost-effectiveness of clinical nurse specialist-led hospital to home transitional care: a systematic review. Journal of Evaluation in Clinical Practice. 2015; 21(5):763–781 [PubMed: 26135524]
- 44.
- Buus BJ, Refsgaard J, Kanstrup H, Paaske JS, Qvist I, Christensen B et al. Hospital-based versus community-based shared care cardiac rehabilitation after acute coronary syndrome: protocol for a randomized clinical trial. Danish Medical Journal. 2013; 60(9):A4699 [PubMed: 24001464]
- 45.
- Campbell H, Karnon J, Dowie R. Cost analysis of a hospital-at-home initiative using discrete event simulation. Journal of Health Services Research and Policy. 2001; 6(1):14–22 [PubMed: 11219355]
- 46.
- Caplan GA, Meller A, Squires B, Chan S, Willett W. Advance care planning and hospital in the nursing home. Age and Ageing. 2006; 35(6):581–585 [PubMed: 16807309]
- 47.
- Caplan GA, Sulaiman NS, Mangin DA, Aimonino Ricauda N, Wilson AD, Barclay L. A meta-analysis of “hospital in the home”. Medical Journal of Australia. 2012; 197(9):512–519 [PubMed: 23121588]
- 48.
- Caplan GA, Williams AJ, Daly B, Abraham K. A randomized, controlled trial of comprehensive geriatric assessment and multidisciplinary intervention after discharge of elderly from the emergency department-the DEED II study. Journal of the American Geriatrics Society. 2004; 52(9):1417–1423 [PubMed: 15341540]
- 49.
- Carroll C. Minding the Gap: what does intermediate care do? CME Journal Geriatric Medicine. 2005; 7(2):96–101
- 50.
- Cassel JB, Kerr K, Pantilat S, Smith TJ. Palliative care consultation and hospital length of stay. Journal of Palliative Medicine. 2010; 13(6):761–767 [PubMed: 20597710]
- 51.
- Chan R, Webster J. A Cochrane review on the effects of end-of-life care pathways: do they improve patient outcomes? Australian Journal of Cancer Nursing. 2011; 12(2):26–30
- 52.
- Chan RJ, Webster J. End-of-life care pathways for improving outcomes in caring for the dying. Cochrane Database of Systematic Reviews. 2013; Issue 11:CD008006. DOI:10.1002/14651858.CD008006.pub3 [PubMed: 24249255] [CrossRef]
- 53.
- Chang HT, Lin MH, Chen CK, Hwang SJ, Hwang IH, Chen YC. Hospice palliative care article publications: an analysis of the Web of Science database from 1993 to 2013. Journal of the Chinese Medical Association. 2016; 79(1):29–33 [PubMed: 26341454]
- 54.
- Chappell H, Dickey C. Decreased rehospitalization costs through intermittent nursing visits to nursing home patients. Journal of Nursing Administration. 1993; 23(3):49–52 [PubMed: 8473929]
- 55.
- Chard SE. Community neurorehabilitation: a synthesis of current evidence and future research directions. NeuroRx. 2006; 3(4):525–534 [PMC free article: PMC3593402] [PubMed: 17012066]
- 56.
- Chen A, Bushmeneva K, Zagorski B, Colantonio A, Parsons D, Wodchis WP. Direct cost associated with acquired brain injury in Ontario. BMC Neurology. 2012; 12:76 [PMC free article: PMC3518141] [PubMed: 22901094]
- 57.
- Chen L-F, Chang C-M, Huang C-Y. Home-based hospice care reduces end-of-life expenditure in Taiwan: a population-based study. Medicine. 2015; 94(38):no [PMC free article: PMC4635767] [PubMed: 26402827]
- 58.
- Chiang J-K, Kao Y-H, Lai N-S. The Impact of hospice care on survival and healthcare costs for patients with lung cancer: a national longitudinal population-based study in Taiwan. PloS One. 2015; 10(9):no [PMC free article: PMC4583292] [PubMed: 26406871]
- 59.
- Clark MM, Rummans TA, Sloan JA, Jensen A, Atherton PJ, Frost MH et al. Quality of life of caregivers of patients with advanced-stage cancer. American Journal of Hospice and Palliative Care. 2006; 23(3):185–191 [PubMed: 17060277]
- 60.
- Coast J, Richards SH, Peters TJ, Gunnell DJ, Darlow MA, Pounsford J. Hospital at home or acute hospital care? A cost minimisation analysis. BMJ. 1998; 316(7147):1802–1806 [PMC free article: PMC28581] [PubMed: 9624074]
- 61.
- Cobelli F, Tavazzi L. Relative role of ambulatory and residential rehabilitation. Journal of Cardiovascular Risk. 1996; 3(2):172–175 [PubMed: 8836859]
- 62.
- Coburn AF, Fortinsky RH, McGuire CA. The impact of Medicaid reimbursement policy on subacute care in hospitals. Medical Care. 1989; 27(1):25–33 [PubMed: 2492065]
- 63.
- Cohen IL, Booth FV. Cost containment and mechanical ventilation in the United States. New Horizons. 1994; 2(3):283–290 [PubMed: 8087585]
- 64.
- Colprim D, Inzitari M. Incidence and risk factors for unplanned transfers to acute general hospitals from an intermediate care and rehabilitation geriatric facility. Journal of the American Medical Directors Association. 2014; 15(9):687–4 [PubMed: 25086689]
- 65.
- Colprim D, Martin R, Parer M, Prieto J, Espinosa L, Inzitari M. Direct admission to intermediate care for older adults with reactivated chronic diseases as an alternative to conventional hospitalization. Journal of the American Medical Directors Association. 2013; 14(4):300–302 [PubMed: 23294969]
- 66.
- Cowie A, Moseley O. Home- versus hospital-based exercise training in heart failure: an economic analysis. British Journal of Cardiology. 2014; 21(2):76
- 67.
- Craig LE, Wu O, Bernhardt J, Langhorne P. Approaches to economic evaluations of stroke rehabilitation. International Journal of Stroke. 2014; 9(1):88–100 [PubMed: 23521855]
- 68.
- Crawford-Faucher A. Home- and center-based cardiac rehabilitation equally effective. American Family Physician. 2010; 82(8):994–995
- 69.
- Crotty M, Kittel A, Hayball N. Home rehabilitation for older adults with fractured hips: how many will take part? Journal of Quality in Clinical Practice. 2000; 20(2-3):65–68 [PubMed: 11057986]
- 70.
- Crotty M, Miller M, Whitehead C, Krishnan J, Hearn T. Hip fracture treatments-what happens to patients from residential care? Journal of Quality in Clinical Practice. 2000; 20(4):167–170 [PubMed: 11207957]
- 71.
- Crotty M, Whitehead C, Miller M, Gray S. Patient and caregiver outcomes 12 months after home-based therapy for hip fracture: a randomized controlled trial. Archives of Physical Medicine and Rehabilitation. 2003; 84(8):1237–1239 [PubMed: 12917867]
- 72.
- Crotty M, Whitehead CH, Gray S, Finucane PM. Early discharge and home rehabilitation after hip fracture achieves functional improvements: a randomized controlled trial. Clinical Rehabilitation. 2002; 16(4):406–413 [PubMed: 12061475]
- 73.
- Cummings JE, Hughes SL, Weaver FM, Manheim LM, Conrad KJ, Nash K et al. Cost-effectiveness of Veterans Administration hospital-based home care. A randomized clinical trial. Archives of Internal Medicine. 1990; 150(6):1274–1280 [PubMed: 2112906]
- 74.
- Cunliffe A, Husbands S, Gladman J. Satisfaction with an early supported discharge service for older people. Age and Ageing. 2002; 31:(Suppl 2):43
- 75.
- Dalal HM, Evans PH. Achieving national service framework standards for cardiac rehabilitation and secondary prevention. BMJ. 2003; 326(7387):481–484 [PMC free article: PMC150183] [PubMed: 12609946]
- 76.
- Daly BJ, Douglas SL, Gunzler D, Lipson AR. Clinical trial of a supportive care team for patients with advanced cancer. Journal of Pain and Symptom Management. 2013; 46(6):775–784 [PMC free article: PMC3715594] [PubMed: 23523362]
- 77.
- Davis MP, Temel JS, Balboni T, Glare P. A review of the trials which examine early integration of outpatient and home palliative care for patients with serious illnesses. Annals of Palliative Medicine. 2015; 4(3):99–121 [PubMed: 26231807]
- 78.
- Deutsch A, Granger CV, Heinemann AW, Fiedler RC, DeJong G, Kane RL et al. Poststroke rehabilitation: outcomes and reimbursement of inpatient rehabilitation facilities and subacute rehabilitation programs. Stroke. 2006; 37(6):1477–1482 [PubMed: 16627797]
- 79.
- Dey P, Woodman M, and FASTER trial group. Manchester FASTER trial [unpublished], 2003
- 80.
- Dias FD, Sampaio LMM, da Silva GA, Gomes ELFD, do Nascimento ESP, Alves VLS et al. Home-based pulmonary rehabilitation in patients with chronic obstructive pulmonary disease: a randomized clinical trial. International Journal of Chronic Obstructive Pulmonary Disease. 2013; 8:537–544 [PMC free article: PMC3821544] [PubMed: 24235824]
- 81.
- DiMartino LD, Weiner BJ, Mayer DK, Jackson GL, Biddle AK. Do palliative care interventions reduce emergency department visits among patients with cancer at the end of life? A systematic review. Journal of Palliative Medicine. 2014; 17(12):1384–1399 [PubMed: 25115197]
- 82.
- Dolansky MA, Xu F, Zullo M, Shishehbor M, Moore SM, Rimm AA. Post-acute care services received by older adults following a cardiac event: a population-based analysis. Journal of Cardiovascular Nursing. 2010; 25(4):342–349 [PMC free article: PMC2885047] [PubMed: 20539168]
- 83.
- Dombi WA. Avalere health study conclusively proves home care is cost effective, saves billions for Medicare yearly, and effectively limits re-hospitalization. Caring. 2009; 28(6):22–23 [PubMed: 19626962]
- 84.
- Donaldson RJ. Hospital versus domiciliary care in acute myocardial infarction. Health and Hygiene. 1982; 4(2-4):103–107
- 85.
- Donath S. Hospital in the home: real cost reductions or merely cost-shifting? Australian and New Zealand Journal of Public Health. 2001; 25(2):187–188 [PubMed: 11357920]
- 86.
- Donlevy JA, Pietruch BL. The connection delivery model: care across the continuum. Nursing Management. 1996; 27(5):34–36 [PubMed: 8710342]
- 87.
- Donnelly ML, Jamieson JL, Brett-Maclean P. Primary care geriatrics in British Columbia: a short report. Geriatrics Today: Journal of the Canadian Geriatrics Society. 2002; 5(4):175–178
- 88.
- Dorney-Smith S. Nurse-led homeless intermediate care: an economic evaluation. British Journal of Nursing. 2011; 20(18):1193–1197 [PubMed: 22067642]
- 89.
- Dow B. The shifting cost of care: early discharge for rehabilitation. Australian Health Review. 2004; 28(3):260–265 [PubMed: 15595907]
- 90.
- Dow B, Black K, Bremner F, Fearn M. A comparison of a hospital-based and two home-based rehabilitation programmes. Disability and Rehabilitation. 2007; 29(8):635–641 [PubMed: 17453984]
- 91.
- Duffy JR, Hoskins LM, Dudley-Brown S. Improving outcomes for older adults with heart failure: a randomized trial using a theory-guided nursing intervention. Journal of Nursing Care Quality. 2010; 25(1):56–64 [PubMed: 19512945]
- 92.
- Dyar S, Lesperance M, Shannon R, Sloan J, Colon-Otero G. A nurse practitioner directed intervention improves the quality of life of patients with metastatic cancer: results of a randomized pilot study. Journal of Palliative Medicine. 2012; 15(8):890–895 [PMC free article: PMC3396133] [PubMed: 22559906]
- 93.
- Eldar R. Rehabilitation in the community for patients with stroke: a review. Topics in Stroke Rehabilitation. 2000; 6(4):48–59
- 94.
- Elder AT. Can we manage more acutely ill elderly patients in the community? Age and Ageing. 2001; 30(6):441–443 [PubMed: 11742768]
- 95.
- Emme C, Mortensen EL, Rydahl-Hansen S, Ostergaard B, Svarre Jakobsen A, Schou L et al. The impact of virtual admission on self-efficacy in patients with chronic obstructive pulmonary disease - a randomised clinical trial. Journal of Clinical Nursing. 2014; 23(21-22):3124–3137 [PubMed: 24476457]
- 96.
- Emme C, Rydahl-Hansen S, Ostergaard B, Schou L, Svarre Jakobsen A, Phanareth K. How virtual admission affects coping - telemedicine for patients with chronic obstructive pulmonary disease. Journal of Clinical Nursing. 2014; 23(9-10):1445–1458 [PubMed: 24372676]
- 97.
- Engelhardt JB, McClive-Reed KP, Toseland RW, Smith TL, Larson DG, Tobin DR. Effects of a program for coordinated care of advanced illness on patients, surrogates, and healthcare costs: a randomized trial. American Journal of Managed Care. 2006; 12(2):93–100 [PubMed: 16464138]
- 98.
- Eron LJ, Marineau M, Baclig E, Yonehara C, King P. The virtual hospital: treating acute infections in the home by telemedicine. Hawaii Medical Journal. 2004; 63(10):291–293 [PubMed: 15570714]
- 99.
- Feltner C, Jones CD, Cene CW, Zheng ZJ, Sueta CA, Coker-Schwimmer EJL et al. Transitional care interventions to prevent readmissions for persons with heart failure: a systematic review and meta-analysis. Annals of Internal Medicine. 2014; 160(11):774–784 [PubMed: 24862840]
- 100.
- Ferrell B, Sun V, Hurria A, Cristea M, Raz DJ, Kim JY et al. Interdisciplinary palliative care for patients with lung cancer. Journal of Pain and Symptom Management. 2015; 50(6):758–767 [PMC free article: PMC4666729] [PubMed: 26296261]
- 101.
- Fischer SM, Cervantes L, Fink RM, Kutner JS. Apoyo con Carino: a pilot randomized controlled trial of a patient navigator intervention to improve palliative care outcomes for Latinos with serious illness. Journal of Pain and Symptom Management. 2015; 49(4):657–665 [PMC free article: PMC4705861] [PubMed: 25240788]
- 102.
- Gaspoz JM, Lee TH, Weinstein MC, Cook EF, Goldman P, Komaroff AL et al. Cost-effectiveness of a new short-stay unit to “rule out” acute myocardial infarction in low risk patients. Journal of the American College of Cardiology. 1994; 24(5):1249–1259 [PubMed: 7930247]
- 103.
- Glasby J, Martin G, Regen E. Older people and the relationship between hospital services and intermediate care: results from a national evaluation. Journal of Interprofessional Care. 2008; 22(6):639–649 [PubMed: 19012144]
- 104.
- Glick HA, Polsky D, Willke RJ, Alves WM, Kassell N, Schulman K. Comparison of the use of medical resources and outcomes in the treatment of aneurysmal subarachnoid hemorrhage between Canada and the United States. Stroke. 1998; 29(2):351–358 [PubMed: 9472873]
- 105.
- Gobbi M, Monger E, Watkinson G, Spencer A, Weaver M, Lathlean J et al. Virtual Interactive Practice: a strategy to enhance learning and competence in health care students. Studies in Health Technology and Informatics. 2004; 107(Pt 2):874–878 [PubMed: 15360937]
- 106.
- Gomes B, Calanzani N, Curiale V, McCrone P, Higginson IJ. Effectiveness and cost-effectiveness of home palliative care services for adults with advanced illness and their caregivers. Cochrane Database of Systematic Reviews. 2013; Issue 6:CD007760. DOI:10.1002/14651858.CD007760.pub2 [PMC free article: PMC4473359] [PubMed: 23744578] [CrossRef]
- 107.
- Gracey DR, Viggiano RW, Naessens JM, Hubmayr RD, Silverstein MD, Koenig GE. Outcomes of patients admitted to a chronic ventilator-dependent unit in an acute-care hospital. Mayo Clinic Proceedings. 1992; 67(2):131–136 [PubMed: 1545576]
- 108.
- Graham LA. Organization of rehabilitation services. Handbook of Clinical Neurology. 2013; 110:113–120 [PubMed: 23312635]
- 109.
- Grande GE, Farquhar MC, Barclay SI, Todd CJ. Caregiver bereavement outcome: relationship with hospice at home, satisfaction with care, and home death. Journal of Palliative Care. 2004; 20(2):69–77 [PubMed: 15332470]
- 110.
- Grande GE, Todd CJ, Barclay SI, Farquhar MC. Does hospital at home for palliative care facilitate death at home? Randomised controlled trial. BMJ. 1999; 319(7223):1472–1475 [PMC free article: PMC28293] [PubMed: 10582932]
- 111.
- Grande GE, Todd CJ, Barclay SI, Farquhar MC. A randomized controlled trial of a hospital at home service for the terminally ill. Palliative Medicine. 2000; 14(5):375–385 [PubMed: 11064784]
- 112.
- Graverholt B, Forsetlund L, Jamtvedt G. Reducing hospital admissions from nursing homes: a systematic review. BMC Health Services Research. 2014; 14:36 [PMC free article: PMC3906881] [PubMed: 24456561]
- 113.
- Greer JA, Pirl WF, Jackson VA, Muzikansky A, Lennes IT, Heist RS et al. Effect of early palliative care on chemotherapy use and end-of-life care in patients with metastatic non-small-cell lung cancer. Journal of Clinical Oncology. 2012; 30(4):394–400 [PubMed: 22203758]
- 114.
- Gregory P, Edwards L, Faurot K, Williams SW, Felix ACG. Patient preferences for stroke rehabilitation. Topics in Stroke Rehabilitation. 2010; 17(5):394–400 [PubMed: 21131265]
- 115.
- Gregory PC, Han E. Disparities in postacute stroke rehabilitation disposition to acute inpatient rehabilitation vs. home: findings from the North Carolina Hospital Discharge Database. American Journal of Physical Medicine and Rehabilitation. 2009; 88(2):100–107 [PubMed: 19169175]
- 116.
- Griffiths P. Intermediate care in nursing-led units - a comprehensive overview of the evidence base. Reviews in Clinical Gerontology. 2006; 16(1):71–77
- 117.
- Griffiths P, Harris R, Richardson G, Hallett N, Heard S, Wilson-Barnett J. Substitution of a nursing-led inpatient unit for acute services: randomized controlled trial of outcomes and cost of nursing-led intermediate care. Age and Ageing. 2001; 30(6):483–488 [PubMed: 11742777]
- 118.
- Griffiths P, Wilson-Barnett J. Influences on length of stay in intermediate care: lessons from the nursing-led inpatient unit studies. International Journal of Nursing Studies. 2000; 37(3):245–255 [PubMed: 10754190]
- 119.
- Griffiths P, Wilson-Barnett J, Richardson G, Spilsbury K, Miller F, Harris R. The effectiveness of intermediate care in a nursing-led in-patient unit. International Journal of Nursing Studies. 2000; 37(2):153–161 [PubMed: 10684957]
- 120.
- Griffiths P. Effectiveness of intermediate care delivered in nurse-led units. British Journal of Community Nursing. 2006; 11(5):205–208 [PubMed: 16723914]
- 121.
- Griffiths P, Edwards M, Forbes A, Harris R. Post-acute intermediate care in nursing-led units: a systematic review of effectiveness. International Journal of Nursing Studies. 2005; 42(1):107–116 [PubMed: 15582644]
- 122.
- Gunnell D, Coast J, Richards SH, Peters TJ, Pounsford JC, Darlow MA. How great a burden does early discharge to hospital-at-home impose on carers? A randomized controlled trial. Age and Ageing. 2000; 29(2):137–142 [PubMed: 10791448]
- 123.
- Hamlet KS, Hobgood A, Hamar GB, Dobbs AC, Rula EY, Pope JE. Impact of predictive model-directed end-of-life counseling for Medicare beneficiaries. American Journal of Managed Care. 2010; 16(5):379–384 [PubMed: 20469958]
- 124.
- Hannan EL, Racz MJ, Walford G, Ryan TJ, Isom OW, Bennett E et al. Predictors of readmission for complications of coronary artery bypass graft surgery. JAMA - Journal of the American Medical Association. 2003; 290(6):773–780 [PubMed: 12915430]
- 125.
- Hansen FR, Spedtsberg K, Schroll M. Geriatric follow-up by home visits after discharge from hospital: a randomized controlled trial. Age and Ageing. 1992; 21(6):445–450 [PubMed: 1471584]
- 126.
- Hardy C, Whitwell D, Sarsfield B, Maimaris C. Admission avoidance and early discharge of acute hospital admissions: an accident and emergency based scheme. Emergency Medicine Journal. 2001; 18(6):435–440 [PMC free article: PMC1725709] [PubMed: 11696489]
- 127.
- Hauser B, Robinson J, Powers JS, Laubacher MA. The evaluation of an intermediate care--geriatric evaluation unit in a Veterans Administration Hospital. Southern Medical Journal. 1991; 84(5):597–602 [PubMed: 2035080]
- 128.
- Herr K, Titler M, Fine PG, Sanders S, Cavanaugh JE, Swegle J et al. The effect of a translating research into practice (TRIP)-cancer intervention on cancer pain management in older adults in hospice. Pain Medicine. 2012; 13(8):1004–1017 [PMC free article: PMC3422373] [PubMed: 22758921]
- 129.
- Heseltine D. Community outreach rehabilitation. Age and Ageing. 2001; 30:(Suppl 3):40–42 [PubMed: 11511487]
- 130.
- Higginson IJ, McCrone P, Hart SR, Burman R, Silber E, Edmonds PM. Is short-term palliative care cost-effective in multiple sclerosis? A randomized phase II trial. Journal of Pain and Symptom Management. 2009; 38(6):816–826 [PubMed: 19833477]
- 131.
- Hill JD, Hampton JR, Mitchell JR. A randomised trial of home-versus-hospital management for patients with suspected myocardial infarction. The Lancet. 1978; 1(8069):837–841 [PubMed: 76794]
- 132.
- Holdsworth LM, Gage H, Coulton S, King A, Butler C. A quasi-experimental controlled evaluation of the impact of a hospice rapid response community service for end-of-life care on achievement of preferred place of death. Palliative Medicine. 2015; 29(9):817–825 [PubMed: 25881623]
- 133.
- Hudson P, Trauer T, Kelly B, O’Connor M, Thomas K, Summers M et al. Reducing the psychological distress of family caregivers of home-based palliative care patients: short-term effects from a randomised controlled trial. Psycho-Oncology. 2013; 22(9):1987–1993 [PubMed: 23335153]
- 134.
- Hudson P, Trauer T, Kelly B, O’Connor M, Thomas K, Zordan R et al. Reducing the psychological distress of family caregivers of home based palliative care patients: longer term effects from a randomised controlled trial. Psycho-Oncology. 2015; 24:19–24 [PMC free article: PMC4309500] [PubMed: 25044819]
- 135.
- Hughes SL, Cummings J, Weaver F, Manheim L, Braun B, Conrad K. A randomized trial of the cost effectiveness of VA hospital-based home care for the terminally ill. Health Services Research. 1992; 26(6):801–817 [PMC free article: PMC1069857] [PubMed: 1737710]
- 136.
- Hughes SL, Cummings J, Weaver F, Manheim LM, Conrad KJ, Nash K. A randomized trial of Veterans Administration home care for severely disabled veterans. Medical Care. 1990; 28(2):135–145 [PubMed: 2153881]
- 137.
- Hughes SL, Weaver FM, Giobbie-Hurder A, Manheim L, Henderson W, Kubal JD et al. Effectiveness of team-managed home-based primary care: a randomized multicenter trial. JAMA - Journal of the American Medical Association. 2000; 284(22):2877–2885 [PubMed: 11147984]
- 138.
- Huo J, Lairson DR, Du XL, Chan W, Buchholz TA, Guadagnolo BA. Survival and cost-effectiveness of hospice care for metastatic melanoma patients. American Journal of Managed Care. 2014; 20(5):366–373 [PubMed: 25181566]
- 139.
- Hwang SJ, Chang HT, Hwang IH, Wu CY, Yang WH, Li CP. Hospice offers more palliative care but costs less than usual care for terminal geriatric hepatocellular carcinoma patients: a nationwide study. Journal of Palliative Medicine. 2013; 16(7):780–785 [PubMed: 23790184]
- 140.
- Indredavik B, Bakke F, Slordahl SA, Rokseth R, Haheim LL. Treatment in a combined acute and rehabilitation stroke unit: which aspects are most important? Stroke. 1999; 30(5):917–923 [PubMed: 10229720]
- 141.
- Indredavik B, Rohweder G, Naalsund E, Lydersen S. Medical complications in a comprehensive stroke unit and an early supported discharge service. Stroke. 2008; 39(2):414–420 [PubMed: 18096834]
- 142.
- Jakobsen AS, Laursen LC, Ostergaard B, Rydahl-Hansen S, Phanareth KV. Hospital-admitted COPD patients treated at home using telemedicine technology in The Virtual Hospital Trial: methods of a randomized effectiveness trial. Trials. 2013; 14:280 [PMC free article: PMC3766220] [PubMed: 24139548]
- 143.
- Johnston B, Larkin P, Connolly M, Barry C, Narayanasamy M, Ostlund U et al. Dignity-conserving care in palliative care settings: an integrative review. Journal of Clinical Nursing. 2015; 24(13-14):1743–1772 [PubMed: 25706903]
- 144.
- Jolly K, Lip GY, Taylor RS, Mant JW, Lane DA, Lee KW et al. Recruitment of ethnic minority patients to a cardiac rehabilitation trial: the Birmingham Rehabilitation Uptake Maximisation (BRUM) study [ISRCTN72884263]. BMC Medical Research Methodology. 2005; 5:18 [PMC free article: PMC1166559] [PubMed: 15904499]
- 145.
- Jones J, Wilson A, Parker H, Wynn A, Jagger C, Spiers N et al. Economic evaluation of hospital at home versus hospital care: cost minimisation analysis of data from randomised controlled trial. BMJ. 1999; 319(7224):1547–1550 [PMC free article: PMC28300] [PubMed: 10591720]
- 146.
- Jones J, Carroll A. Hospital admission avoidance through the introduction of a virtual ward. British Journal of Community Nursing. 2014; 19(7):330–334 [PubMed: 25039341]
- 147.
- Jordhoy MS, Fayers P, Saltnes T, Ahlner-Elmqvist M, Jannert M, Kaasa S. A palliative-care intervention and death at home: a cluster randomised trial. The Lancet. 2000; 356(9233):888–893 [PubMed: 11036893]
- 148.
- Kane RL, Wales J, Bernstein L, Leibowitz A, Kaplan S. A randomised controlled trial of hospice care. The Lancet. 1984; 1(8382):890–894 [PubMed: 6143195]
- 149.
- Kenny RA, O’Shea D, Walker HF. Impact of a dedicated syncope and falls facility for older adults on emergency beds. Age and Ageing. 2002; 31(4):272–275 [PubMed: 12147565]
- 150.
- Kinley J, Hockley J, Stone L, Dewey M, Hansford P, Stewart R et al. The provision of care for residents dying in U.K. nursing care homes. Age and Ageing. 2014; 43:375–379 [PubMed: 24132855]
- 151.
- Konrad D, Corrigan ML, Hamilton C, Steiger E, Kirby DF. Identification and early treatment of dehydration in home parenteral nutrition and home intravenous fluid patients prevents hospital admissions. Nutrition in Clinical Practice. 2012; 27(6):802–807 [PubMed: 23069992]
- 152.
- Koopman MM, Prandoni P, Piovella F, Ockelford PA, Brandjes DP, van der Meer J et al. Treatment of venous thrombosis with intravenous unfractionated heparin administered in the hospital as compared with subcutaneous low-molecular-weight heparin administered at home. The Tasman Study Group. New England Journal of Medicine. 1996; 334(11):682–687 [PubMed: 8594426]
- 153.
- Kornowski R, Zeeli D, Averbuch M, Finkelstein A, Schwartz D, Moshkovitz M et al. Intensive home-care surveillance prevents hospitalization and improves morbidity rates among elderly patients with severe congestive heart failure. American Heart Journal. 1995; 129(4):762–766 [PubMed: 7900629]
- 154.
- Kortke H, Stromeyer H, Zittermann A, Buhr N, Zimmermann E, Wienecke E et al. New East-Westfalian postoperative therapy concept: a telemedicine guide for the study of ambulatory rehabilitation of patients after cardiac surgery. Telemedicine Journal and E-Health. 2006; 12(4):475–483 [PubMed: 16942420]
- 155.
- Korzeniowska-Kubacka I, Bilinska M, Dobraszkiewicz-Wasilewska B, Piotrowicz R. Comparison between hybrid and standard centre-based cardiac rehabilitation in female patients after myocardial infarction: a pilot study. Kardiologia Polska. 2014; 72(3):269–274 [PubMed: 24142752]
- 156.
- Langhorne P, Dennis MS, Kalra L, Shepperd S, Wade DT, Wolfe CD. Services for helping acute stroke patients avoid hospital admission. Cochrane Database of Systematic Reviews. 2000; Issue 2:CD000444. DOI:10.1002/14651858.CD000444 [PubMed: 10796366] [CrossRef]
- 157.
- Langhorne P, Taylor G, Murray G, Dennis M, Anderson C, Bautz-Holter E et al. Early supported discharge services for stroke patients: a meta-analysis of individual patients’ data. The Lancet. 2005; 365(9458):501–506 [PubMed: 15705460]
- 158.
- Lappegard O, Hjortdahl P. Acute admissions to a community hospital: experiences from Hallingdal sjukestugu. Scandinavian Journal of Public Health. 2012; 40(4):309–315 [PubMed: 22786914]
- 159.
- Last S. Intermediate care. Bed spread. Health Service Journal. 2000; 110(5717):22–23 [PubMed: 11183713]
- 160.
- Leon A, Caceres C, Fernandez E, Chausa P, Martin M, Codina C et al. A new multidisciplinary home care telemedicine system to monitor stable chronic human immunodeficiency virus-infected patients: a randomized study. PloS One. 2011; 6(1):e14515 [PMC free article: PMC3024968] [PubMed: 21283736]
- 161.
- Leppert W, Majkowicz M, Forycka M, Mess E, Zdun-Ryzewska A. Quality of life assessment in advanced cancer patients treated at home, an inpatient unit, and a day care center. OncoTargets and Therapy. 2014; 7:687–695 [PMC free article: PMC4020899] [PubMed: 24855379]
- 162.
- Lewis G. Virtual wards, real nursing. Nursing Standard. 2007; 21(43):64 [PubMed: 17695588]
- 163.
- Lewis G, Bardsley M, Vaithianathan R, Steventon A, Georghiou T, Billings J et al. Do ‘virtual wards’ reduce rates of unplanned hospital admissions, and at what cost? A research protocol using propensity matched controls. International Journal of Integrated Care. 2011; 11:e079 [PMC free article: PMC3178802] [PubMed: 21949489]
- 164.
- Lewis G, Vaithianathan R, Wright L, Brice MR, Lovell P, Rankin S et al. Integrating care for high-risk patients in England using the virtual ward model: lessons in the process of care integration from three case sites. International Journal of Integrated Care. 2013; 13:e046 [PMC free article: PMC3821539] [PubMed: 24250284]
- 165.
- Lewis G, Wright L, Vaithianathan R. Multidisciplinary case management for patients at high risk of hospitalization: comparison of virtual ward models in the United kingdom, United States, and Canada. Population Health Management. 2012; 15(5):315–321 [PubMed: 22788975]
- 166.
- Lewis GH, Georghiou T, and Steventon A. Impact of “Virtual Wards” on hospital use: a research study using propensity matched controls and a cost analysis. Southampton. National Institute for Health Research, 2013. Available from: http://www
.nets.nihr .ac.uk/__data/assets /pdf_file/0011/87923/FR-09-1816-1021.pdf - 167.
- Lim WK, Lambert SF, Gray LC. Effectiveness of case management and post-acute services in older people after hospital discharge. Medical Journal of Australia. Australia 2003; 178(6):262–266 [PubMed: 12633482]
- 168.
- Linertova R, Garcia-Perez L, Vazquez-Diaz JR, Lorenzo-Riera A, Sarria-Santamera A. Interventions to reduce hospital readmissions in the elderly: in-hospital or home care. A systematic review. Journal of Evaluation in Clinical Practice. 2011; 17(6):1167–1175 [PubMed: 20630005]
- 169.
- Luckett T, Davidson PM, Lam L, Phillips J, Currow DC, Agar M. Do community specialist palliative care services that provide home nursing increase rates of home death for people with life-limiting illnesses? A systematic review and meta-analysis of comparative studies. Journal of Pain and Symptom Management. 2013; 45(2):279–297 [PubMed: 22917710]
- 170.
- Martin F, Oyewole A, Moloney A. A randomized controlled trial of a high support hospital discharge team for elderly people. Age and Ageing. 1994; 23(3):228–234 [PubMed: 8085509]
- 171.
- Mason S, Wardrope J, Perrin J. Developing a community paramedic practitioner intermediate care support scheme for older people with minor conditions. Emergency Medicine Journal. 2003; 20(2):196–198 [PMC free article: PMC1726072] [PubMed: 12642544]
- 172.
- Mather HG, Morgan DC, Pearson NG, Read KL, Shaw DB, Steed GR et al. Myocardial infarction: a comparison between home and hospital care for patients. BMJ. 1976; 1(6015):925–929 [PMC free article: PMC1639298] [PubMed: 1268490]
- 173.
- Matukaitis J, Stillman P, Wykpisz E, Ewen E. Appropriate admissions to the appropriate unit: a decision tree approach. American Journal of Medical Quality. 2005; 20(2):90–97 [PubMed: 15851387]
- 174.
- Mayhew L, Lawrence D. The costs and service implications of substituting intermediate care for acute hospital care. Health Services Management Research. 2006; 19(2):80–93 [PubMed: 16643707]
- 175.
- Mayo N, Wood-Dauphinee S, Tamblyn R, Cote R, Gayton D, Carlton J et al. There’s no place like home: a trial of early discharge and intensive home rehabilitation post stroke. Cerebrovascular Diseases. 1998; 8:(Suppl 4):94
- 176.
- Mayo NE, Wood-Dauphinee S, Cote R, Gayton D, Carlton J, Buttery J et al. There’s no place like home: an evaluation of early supported discharge for stroke. Stroke. 2000; 31(5):1016–1023 [PubMed: 10797160]
- 177.
- McCorkle R, Benoliel JQ, Donaldson G, Georgiadou F, Moinpour C, Goodell B. A randomized clinical trial of home nursing care for lung cancer patients. Cancer. 1989; 64(6):1375–1382 [PubMed: 2670188]
- 178.
- McKegney FP, Bailey LR, Yates JW. Prediction and management of pain in patients with advanced cancer. General Hospital Psychiatry. 1981; 3(2):95–101 [PubMed: 6166512]
- 179.
- McLoughlin K, Rhatigan J, McGilloway S, Kellehear A, Lucey M, Twomey F et al. INSPIRE (INvestigating Social and PractIcal suppoRts at the End of life): pilot randomised trial of a community social and practical support intervention for adults with life-limiting illness. BMC Palliative Care. 2015; 14:65 [PMC free article: PMC4658760] [PubMed: 26603516]
- 180.
- McMillan SC, Small BJ. Using the COPE intervention for family caregivers to improve symptoms of hospice homecare patients: a clinical trial. Oncology Nursing Forum. 2007; 34(2):313–321 [PubMed: 17573295]
- 181.
- McMillan SC, Small BJ, Weitzner M, Schonwetter R, Tittle M, Moody L et al. Impact of coping skills intervention with family caregivers of hospice patients with cancer: a randomized clinical trial. Cancer. 2006; 106(1):214–222 [PubMed: 16329131]
- 182.
- McNamee P, Christensen J, Soutter J, Rodgers H, Craig N, Pearson P et al. Cost analysis of early supported hospital discharge for stroke. Age and Ageing. 1998; 27(3):345–351
- 183.
- McWhinney IR, Bass MJ, Donner A. Evaluation of a palliative care service: problems and pitfalls. BMJ. 1994; 309(6965):1340–1342 [PMC free article: PMC2541867] [PubMed: 7532501]
- 184.
- Melin AL, Bygren LO. Efficacy of the rehabilitation of elderly primary health care patients after short-stay hospital treatment. Medical Care. 1992; 30(11):1004–1015 [PubMed: 1331632]
- 185.
- Meyer RP. Consider medical care at home. Geriatrics. 2009; 64(6):9–11 [PubMed: 19572761]
- 186.
- Meyers FJ, Carducci M, Loscalzo MJ, Linder J, Greasby T, Beckett LA. Effects of a problem-solving intervention (COPE) on quality of life for patients with advanced cancer on clinical trials and their caregivers: simultaneous care educational intervention (SCEI): linking palliation and clinical trials. Journal of Palliative Medicine. 2011; 14(4):465–473 [PMC free article: PMC3070139] [PubMed: 21413846]
- 187.
- Miller DK, Chibnall JT, Videen SD, Duckro PN. Supportive-affective group experience for persons with life-threatening illness: reducing spiritual, psychological, and death-related distress in dying patients. Journal of Palliative Medicine. 2005; 8(2):333–343 [PubMed: 15890044]
- 188.
- Molassiotis A, Brearley S, Saunders M, Craven O, Wardley A, Farrell C et al. Effectiveness of a home care nursing program in the symptom management of patients with colorectal and breast cancer receiving oral chemotherapy: a randomized, controlled trial. Journal of Clinical Oncology. 2009; 27(36):6191–6198 [PubMed: 19917849]
- 189.
- Muijen M, Marks I, Connolly J, Audini B. Home based care and standard hospital care for patients with severe mental illness: a randomised controlled trial. BMJ. 1992; 304(6829):749–754 [PMC free article: PMC1881624] [PubMed: 1571681]
- 190.
- Nicholson C, Bowler S, Jackson C, Schollay D, Tweeddale M, O’Rourke P. Cost comparison of hospital- and home-based treatment models for acute chronic obstructive pulmonary disease. Australian Health Review. 2001; 24(4):181–187 [PubMed: 11842709]
- 191.
- Nissen I, Jensen MS. Nurse-supported discharge of patients with exacerbation of chronic obstructive pulmonary disease. Ugeskrift for Laeger. 2007; 169(23):2220–2223 [PubMed: 17592691]
- 192.
- Nordly M, Benthien KS, Von Der Maase H, Johansen C, Kruse M, Timm H et al. The DOMUS study protocol: a randomized clinical trial of accelerated transition from oncological treatment to specialized palliative care at home. BMC Palliative Care. 2014; 13:44 [PMC free article: PMC4169691] [PubMed: 25242890]
- 193.
- Nordly M, Vadstrup ES, Sjogren P, Kurita GP. Home-based specialized palliative care in patients with advanced cancer: a systematic review. Palliative and Supportive Care. 2016; 14(6):713–724 [PubMed: 27407075]
- 194.
- Nyatanga B. Extending virtual wards to palliative care delivered in the community. British Journal of Community Nursing. 2014; 19(7):328–329 [PubMed: 25039340]
- 195.
- Organisation for Economic Co-operation and Development (OECD). Purchasing power parities (PPP), 2007. Available from: http://www
.oecd.org/std/ppp - 196.
- Pace A, Villani V, Di Pasquale A, Benincasa D, Guariglia L, Ieraci S et al. Home care for brain tumor patients. Neuro-Oncology Practice. 2014; 1(1):8–12 [PMC free article: PMC4369701] [PubMed: 26034609]
- 197.
- Palmer Hill S, Flynn J, Crawford EJP. Early discharge following total knee replacement -- a trial of patient satisfaction and outcomes using an orthopaedic outreach team. Journal of Orthopaedic Nursing. 2000; 4(3):121–126
- 198.
- Pandian JD. A multicentre, randomized, blinded outcome assessor, controlled trial, whether a family-led caregiver-delivered home-based rehabilitation intervention versus usual care is an effective, affordable Early Support Discharge strategy for those with disabling stroke in India. 2013. Available from: http://www
.ctri.nic.in /Clinicaltrials/pmaindet2 .php?trialid=6195 [Last accessed: 29 December 14 A.D.] - 199.
- Patel A, Knapp M, Perez I, Evans A, Kalra L. Alternative strategies for stroke care: cost-effectiveness and cost-utility analyses from a prospective randomized controlled trial. Stroke. 2004; 35(1):196–203 [PubMed: 14684783]
- 200.
- Penque S, Petersen B, Arom K, Ratner E, Halm M. Early discharge with home health care in the coronary artery bypass patient. Dimensions of Critical Care Nursing. 1999; 18(6):40–48 [PubMed: 10640054]
- 201.
- Pergolotti M, Deal AM, Williams GR, Bryant AL, Reeve BB, Muss HB. A randomized controlled trial of outpatient CAncer REhabilitation for older adults: the CARE Program. Contemporary Clinical Trials. 2015; 44:89–94 [PMC free article: PMC4740286] [PubMed: 26253182]
- 202.
- Pirl WF, Greer JA, Traeger L, Jackson V, Lennes IT, Gallagher ER et al. Depression and survival in metastatic non-small-cell lung cancer: effects of early palliative care. Journal of Clinical Oncology. 2012; 30(12):1310–1315 [PMC free article: PMC3341144] [PubMed: 22430269]
- 203.
- Pittiglio LI, Harris MA, Mili F. Development and evaluation of a three-dimensional virtual hospital unit: VI-MED. Computers, Informatics, Nursing. 2011; 29(5):267–271 [PubMed: 21633205]
- 204.
- Plant NA, Kelly PJ, Leeder SR, D’Souza M, Mallitt KA, Usherwood T et al. Coordinated care versus standard care in hospital admissions of people with chronic illness: a randomised controlled trial. Medical Journal of Australia. 2015; 203(1):33–38 [PubMed: 26126565]
- 205.
- Plochg T, Delnoij DMJ, van der Kruk TF, Janmaat TACM, Klazinga NS. Intermediate care: for better or worse? Process evaluation of an intermediate care model between a university hospital and a residential home. BMC Health Services Research. 2005; 5:38 [PMC free article: PMC1168893] [PubMed: 15910689]
- 206.
- Pozzilli C, Brunetti M, Amicosante AMV, Gasperini C, Ristori G, Palmisano L et al. Home based management in multiple sclerosis: results of a randomised controlled trial. Journal of Neurology, Neurosurgery and Psychiatry. 2002; 73(3):250–255 [PMC free article: PMC1738043] [PubMed: 12185154]
- 207.
- Prior MK, Bahret BA, Allen RI, Pasupuleti S. The efficacy of a senior outreach program in the reduction of hospital readmissions and emergency department visits among chronically ill seniors. Social Work in Health Care. 2012; 51(4):345–360 [PubMed: 22489558]
- 208.
- Puig-Junoy J, Casas A, Font-Planells J, Escarrabill J, Hernandez C, Alonso J et al. The impact of home hospitalization on healthcare costs of exacerbations in COPD patients. European Journal of Health Economics. 2007; 8(4):325–332 [PubMed: 17221178]
- 209.
- Rabow MW, Dibble SL, Pantilat SZ, McPhee SJ. The comprehensive care team: a controlled trial of outpatient palliative medicine consultation. Archives of Internal Medicine. 2004; 164(1):83–91 [PubMed: 14718327]
- 210.
- Radwany SM, Hazelett SE, Allen KR, Kropp DJ, Ertle D, Albanese TH et al. Results of the promoting effective advance care planning for elders (PEACE) randomized pilot study. Population Health Management. 2014; 17(2):106–111 [PubMed: 24156664]
- 211.
- Raftery JP, Addington-Hall JM, MacDonald LD, Anderson HR, Bland JM, Chamberlain J et al. A randomized controlled trial of the cost-effectiveness of a district co-ordinating service for terminally ill cancer patients. Palliative Medicine. 1996; 10(2):151–161 [PubMed: 8800823]
- 212.
- Raphael MJ, Nadeau-Fredette AC, Tennankore KK, Chan CT. A virtual ward for home hemodialysis patients - a pilot trial. Canadian Journal of Kidney Health and Disease. 2015; 2:37 [PMC free article: PMC4628781] [PubMed: 26527130]
- 213.
- Ricauda NA, Bo M, Molaschi M, Massaia M, Salerno D, Amati D et al. Home hospitalization service for acute uncomplicated first ischemic stroke in elderly patients: a randomized trial. Journal of the American Geriatrics Society. 2004; 52(2):278–283 [PubMed: 14728641]
- 214.
- Richards SH. Correction: randomised controlled trial comparing effectiveness and acceptability of an early discharge, hospital at home scheme with acute hospital care (British Medical Journal (1998) 13 June (1796-1801)). BMJ. 1998; 317(7161):786 [PMC free article: PMC28580] [PubMed: 9624070]
- 215.
- Richards SH, Coast J, Gunnell DJ, Peters TJ, Pounsford J, Darlow MA. Randomised controlled trial comparing effectiveness and acceptability of an early discharge, hospital at home scheme with acute hospital care. BMJ. 1998; 316(7147):1796–1801 [PMC free article: PMC28580] [PubMed: 9624070]
- 216.
- Richardson G, Griffiths P, Wilson-Barnett J, Spilsbury K, Batehup L. Economic evaluation of a nursing-led intermediate care unit. International Journal of Technology Assessment in Health Care. 2001; 17(3):442–450 [PubMed: 11495387]
- 217.
- Robinson J. Facilitating earlier transfer of care from acute stroke services into the community. Nursing Times. 2009; 105(12):12–13 [PubMed: 19363928]
- 218.
- Rodriguez-Cerrillo M, Poza-Montoro A, Fernandez-Diaz E, Inurrieta-Romero A, Matesanz-David M. Home treatment of patients with acute cholecystitis. European Journal of Internal Medicine. 2012; 23(1):e10–e13 [PubMed: 22153541]
- 219.
- Rodriguez-Cerrillo M, Poza-Montoro A, Fernandez-Diaz E, Romero AI. Patients with uncomplicated diverticulitis and comorbidity can be treated at home. European Journal of Internal Medicine. 2010; 21(6):553–554 [PubMed: 21111943]
- 220.
- Rosbotham-Williams A. Integrating health care services for older people. Nursing Times. 2002; 98(32):40–41 [PubMed: 12211912]
- 221.
- Round A, Crabb T, Buckingham K, Mejzner R, Pearce V, Ayres R et al. Six month outcomes after emergency admission of elderly patients to a community or a district general hospital. Family Practice. 2004; 21(2):173–179 [PubMed: 15020387]
- 222.
- Rout A, Ashby S, Maslin-Prothero S, Masterson A, Priest H, Beach M et al. A literature review of interprofessional working and intermediate care in the UK. Journal of Clinical Nursing. 2011; 20(5-6):775–783 [PubMed: 20662994]
- 223.
- Rowley JM, Hampton JR, Mitchell JR. Home care for patients with suspected myocardial infarction: use made by general practitioners of a hospital team for initial management. BMJ. 1984; 289(6442):403–406 [PMC free article: PMC1442427] [PubMed: 6432118]
- 224.
- Ruckley CV, Cuthbertson C, Fenwick N, Prescott RJ, Garraway WM. Day care after operations for hernia or varicose veins: a controlled trial. British Journal of Surgery. 1978; 65(7):456–459 [PubMed: 352473]
- 225.
- Rudkin ST, Harrison S, Harvey I, White RJ. A randomised trial of hospital v home rehabilitation in severe chronic ostructive pulmonary disease (COPD). Thorax. 1997; 52:(Suppl 6):A11
- 226.
- Rummans TA, Clark MM, Sloan JA, Frost MH, Bostwick JM, Atherton PJ et al. Impacting quality of life for patients with advanced cancer with a structured multidisciplinary intervention: a randomized controlled trial. Journal of Clinical Oncology. 2006; 24(4):635–642 [PubMed: 16446335]
- 227.
- Sahlen KG, Boman K, Brannstrom M. A cost-effectiveness study of person-centered integrated heart failure and palliative home care: based on a randomized controlled trial. Palliative Medicine. 2016; 30(3):296–302 [PubMed: 26603186]
- 228.
- Sartain SA, Maxwell MJ, Todd PJ, Jones KH, Bagust A, Haycox A et al. Randomised controlled trial comparing an acute paediatric hospital at home scheme with conventional hospital care. Archives of Disease in Childhood. 2002; 87(5):371–375 [PMC free article: PMC1763073] [PubMed: 12390903]
- 229.
- Saysell E, Routley C. Pilot project of an intermediate palliative care unit within a registered care home. International Journal of Palliative Nursing. 2004; 10(8):393–398 [PubMed: 15365494]
- 230.
- Schachter ME, Bargman JM, Copland M, Hladunewich M, Tennankore KK, Levin A et al. Rationale for a home dialysis virtual ward: design and implementation. BMC Nephrology. 2014; 15:33 [PMC free article: PMC3930556] [PubMed: 24528505]
- 231.
- Scheinberg L, Koren MJ, Bluestone M, McDowell FH. Effects of early hospital discharge to home care on the costs and outcome of care of stroke patients: a randomised trial in progress. Cerebrovascular Diseases. 1986; 1:289–296
- 232.
- Schneller K. Intermediate care for homeless people: results of a pilot project. Emergency Nurse. 2012; 20(6):20–24 [PubMed: 23167008]
- 233.
- Schou L, Ostergaard B, Rasmussen LS, Rydahl-Hansen S, Jakobsen AS, Emme C et al. Telemedicine-based treatment versus hospitalization in patients with severe chronic obstructive pulmonary disease and exacerbation: effect on cognitive function. A randomized clinical trial. Telemedicine Journal and E-Health. 2014; 20(7):640–646 [PubMed: 24820535]
- 234.
- Scott IA. Public hospital bed crisis: too few or too misused? Australian Health Review. 2010; 34(3):317–324 [PubMed: 20797364]
- 235.
- Senaratne MP, Irwin ME, Shaben S, Griffiths J, Nagendran J, Kasza L et al. Feasibility of direct discharge from the coronary/intermediate care unit after acute myocardial infarction. Journal of the American College of Cardiology. 1999; 33(4):1040–1046 [PubMed: 10091833]
- 236.
- Seow H, Pataky R, Lawson B, O’Leary EM, Sutradhar R, Fassbender K et al. Temporal association between home nursing and hospital costs at end of life in three provinces. Current Oncology. 2016; 23:(Suppl 1):S42–S51 [PMC free article: PMC4780588] [PubMed: 26985145]
- 237.
- Shepperd S. Hospital at home: the evidence is not compelling. Annals of Internal Medicine. 2005; 143(11):840–841 [PubMed: 16330798]
- 238.
- Shepperd S, Harwood D, Gray A, Vessey M, Morgan P. Randomised controlled trial comparing hospital at home care with inpatient hospital care. II: cost minimisation analysis. BMJ. 1998; 316(7147):1791–1796 [PMC free article: PMC28579] [PubMed: 9624069]
- 239.
- Shepperd S, Iliffe S. The effectiveness of hospital at home compared with in-patient hospital care: a systematic review. Journal of Public Health Medicine. 1998; 20(3):344–350 [PubMed: 9793901]
- 240.
- Shepperd S, Doll H, Angus RM, Clarke MJ, Iliffe S, Kalra L et al. Hospital at home admission avoidance. Cochrane Database of Systematic Reviews. 2008; Issue 4:CD007491. DOI:10.1002/14651858.CD007491 [PMC free article: PMC4033791] [PubMed: 18843751] [CrossRef]
- 241.
- Shepperd S, Doll H, Angus RM, Clarke MJ, Iliffe S, Kalra L et al. Avoiding hospital admission through provision of hospital care at home: a systematic review and meta-analysis of individual patient data. CMAJ Canadian Medical Association Journal. 2009; 180(2):175–182 [PMC free article: PMC2621299] [PubMed: 19153394]
- 242.
- Shepperd S, Wee B, Straus SE. Hospital at home: home-based end of life care. Cochrane Database of Systematic Reviews. 2011; Issue 7:CD009231. DOI:10.1002/14651858.CD009231 [PMC free article: PMC4033790] [PubMed: 21735440] [CrossRef]
- 243.
- Shnoor Y, Szlaifer M, Aoberman AS, Bentur N. The cost of home hospice care for terminal patients in Israel. American Journal of Hospice and Palliative Care. 2007; 24(4):284–290 [PubMed: 17601831]
- 244.
- Sidebottom AC, Jorgenson A, Richards H, Kirven J, Sillah A. Inpatient palliative care for patients with acute heart failure: outcomes from a randomized trial. Journal of Palliative Medicine. 2015; 18(2):134–142 [PubMed: 25479182]
- 245.
- Singh T, Harding R. Palliative care in South Asia: a systematic review of the evidence for care models, interventions, and outcomes. BMC Research Notes. 2015; 8:172 [PMC free article: PMC4422038] [PubMed: 25925664]
- 246.
- Stephenson AE, Chetwynd SJ. A method of analysing general practioner decision making concerning home or hospital coronary care. Community Health Studies. 1984; 8(3):297–300 [PubMed: 6518748]
- 247.
- Steventon A, Bardsley M, Billings J, Georghiou T, Lewis GH. The role of matched controls in building an evidence base for hospital-avoidance schemes: a retrospective evaluation. Health Services Research. 2012; 47(4):1679–1698 [PMC free article: PMC3401405] [PubMed: 22224902]
- 248.
- Stewart S, Marley JE, Horowitz JD. Effects of a multidisciplinary, home-based intervention on unplanned readmissions and survival among patients with chronic congestive heart failure: a randomised controlled study. The Lancet. 1999; 354(9184):1077–1083 [PubMed: 10509499]
- 249.
- Stromberg A, Martensson J, Fridlund B, Levin LA, Karlsson JE, Dahlstrom U. Nurse-led heart failure clinics improve survival and self-care behaviour in patients with heart failure: results from a prospective, randomised trial. European Heart Journal. 2003; 24(11):1014–1023 [PubMed: 12788301]
- 250.
- Subirana Serrate R, Ferrer-Roca O, Gonzalez-Davila E. A cost-minimization analysis of oncology home care versus hospital care. Journal of Telemedicine and Telecare. 2001; 7(4):226–232 [PubMed: 11506758]
- 251.
- Suijker JJ, Buurman BM, ter Riet G, van Rijn M, de Haan RJ, de Rooij SE et al. Comprehensive geriatric assessment, multifactorial interventions and nurse-led care coordination to prevent functional decline in community-dwelling older persons: protocol of a cluster randomized trial. BMC Health Services Research. 2012; 12:85 [PMC free article: PMC3374886] [PubMed: 22462516]
- 252.
- Suwanwela NC, Phanthumchinda K, Limtongkul S, Suvanprakorn P. Comparison of short (3-day) hospitalization followed by home care treatment and conventional (10-day) hospitalization for acute ischemic stroke. Cerebrovascular Diseases. 2002; 13(4):267–271 [PubMed: 12011552]
- 253.
- Tamir O, Singer Y, Shvartzman P. Taking care of terminally-ill patients at home - the economic perspective revisited. Palliative Medicine. 2007; 21(6):537–541 [PubMed: 17846094]
- 254.
- Temel JS, Greer JA, Muzikansky A, Gallagher ER, Admane S, Jackson VA et al. Early palliative care for patients with metastatic non-small-cell lung cancer. New England Journal of Medicine. 2010; 363:733–742 [PubMed: 20818875]
- 255.
- Teng J, Mayo NE, Latimer E, Hanley J, Wood-Dauphinee S, Cote R et al. Costs and caregiver consequences of early supported discharge for stroke patients. Stroke. 2003; 34(2):528–536 [PubMed: 12574571]
- 256.
- Thorne D, Jeffery S. Intermediate care. Homeward bound. Health Service Journal. 2001; 111(5785):28–29 [PubMed: 11810755]
- 257.
- Thorsen AM, Holmqvist LW, de Pedro-Cuesta J, von Koch L. A randomized controlled trial of early supported discharge and continued rehabilitation at home after stroke: five-year follow-up of patient outcome. Stroke. 2005; 36(2):297–303 [PubMed: 15618441]
- 258.
- Thorsen AM, Widen Holmqvist L, von Koch L. Early supported discharge and continued rehabilitation at home after stroke: 5-year follow-up of resource use. Journal of Stroke and Cerebrovascular Diseases. 2006; 15(4):139–143 [PubMed: 17904066]
- 259.
- Tibaldi V, Aimonino N, Ponzetto M, Stasi MF, Amati D, Raspo S et al. A randomized controlled trial of a home hospital intervention for frail elderly demented patients: behavioral disturbances and caregiver’s stress. Archives of Gerontology and Geriatrics. 2004; 2004(9):431–436 [PubMed: 15207444]
- 260.
- Toseland RW, Blanchard CG, McCallion P. A problem solving intervention for caregivers of cancer patients. Social Science and Medicine. 1995; 40(4):517–528 [PubMed: 7725125]
- 261.
- Trappes-Lomax T, Ellis A, Fox M, Taylor R, Power M, Stead J et al. Buying time I: a prospective, controlled trial of a joint health/social care residential rehabilitation unit for older people on discharge from hospital. Health and Social Care in the Community. 2006; 14(1):49–62 [PubMed: 16324187]
- 262.
- Tzala S, Lord J, Ziras N, Repousis P, Potamianou A, Tzala E. Cost of home palliative care compared with conventional hospital care for patients with haematological cancers in Greece. European Journal of Health Economics. 2005; 6(2):102–106 [PubMed: 19787846]
- 263.
- Uitdehaag MJ, van Putten PG, van Eijck CHJ, Verschuur EML, van der Gaast A, Pek CJ et al. Nurse-led follow-up at home vs. conventional medical outpatient clinic follow-up in patients with incurable upper gastrointestinal cancer: a randomized study. Journal of Pain and Symptom Management. 2014; 47(3):518–530 [PubMed: 23880585]
- 264.
- Upton S, Culshaw M, Stephenson J. An observational study to identify factors associated with hospital readmission and to evaluate the impact of mandating validation of discharge prescriptions on readmission rate. International Journal of Pharmacy Practice. 2014; 22:45–46
- 265.
- Utens CMA, Goossens LMA, Smeenk FWJM, van Schayck OCP, van Litsenburg W, Janssen A et al. Effectiveness and cost-effectiveness of early assisted discharge for chronic obstructive pulmonary disease exacerbations: the design of a randomised controlled trial. BMC Public Health. 2010; 10:618 [PMC free article: PMC2965725] [PubMed: 20955582]
- 266.
- Van Hout HPJ, Nijpels G, van Marwijk HWJ, Jansen APD, Van’t Veer PJ, Tybout W et al. Design and pilot results of a single blind randomized controlled trial of systematic demand-led home visits by nurses to frail elderly persons in primary care [ISRCTN05358495]. BMC Geriatrics. 2005; 5:11 [PMC free article: PMC1242228] [PubMed: 16150147]
- 267.
- Ventura MdM. Effectiveness and cost-effectiveness of home palliative care services for adults with advanced illness and their caregivers. Sao Paulo Medical Journal. 2016; 134(1):93–94 [PMC free article: PMC10496588] [PubMed: 26786605]
- 268.
- von Koch L, de Pedro-Cuesta J, Kostulas V, Almazan J, Widen HL. Randomized controlled trial of rehabilitation at home after stroke: one-year follow-up of patient outcome, resource use and cost. Cerebrovascular Diseases. 2001; 12(2):131–138 [PubMed: 11490107]
- 269.
- von Koch L, Holmqvist LW, Kostulas V, Almazan J, de Pedro-Cuesta J. A randomized controlled trial of rehabilitation at home after stroke in Southwest Stockholm: outcome at six months. Scandinavian Journal of Rehabilitation Medicine. 2000; 32(2):80–86 [PubMed: 10853722]
- 270.
- Wakefield BJ, Ward MM, Holman JE, Ray A, Scherubel M, Burns TL et al. Evaluation of home telehealth following hospitalization for heart failure: a randomized trial. Telemedicine Journal and E-Health. 2008; 14(8):753–761 [PubMed: 18954244]
- 271.
- Walshe C, Luker KA. District nurses’ role in palliative care provision: a realist review. International Journal of Nursing Studies. 2010; 47(9):1167–1183 [PubMed: 20494357]
- 272.
- Weber C, Stirnemann J, Herrmann FR, Pautex S, Janssens JP. Can early introduction of specialized palliative care limit intensive care, emergency and hospital admissions in patients with severe and very severe COPD? a randomized study. BMC Palliative Care. 2014; 13:47 [PMC free article: PMC4448287] [PubMed: 25927907]
- 273.
- Widen Holmqvist L, de Pedro-Cuesta J, Holm M, Kostulas V. Intervention design for rehabilitation at home after stroke. A pilot feasibility study. Scandinavian Journal of Rehabilitation Medicine. 1995; 27(1):43–50 [PubMed: 7792549]
- 274.
- Widen HL, de Pedro-Cuesta J, Moller G, Holm M, Siden A. A pilot study of rehabilitation at home after stroke: a health-economic appraisal. Scandinavian Journal of Rehabilitation Medicine. 1996; 28(1):9–18 [PubMed: 8701237]
- 275.
- Widen HL, von Koch L, Kostulas V, Holm M, Widsell G, Tegler H et al. A randomized controlled trial of rehabilitation at home after stroke in southwest Stockholm. Stroke. 1998; 29(3):591–597 [PubMed: 9506598]
- 276.
- Winkel A, Ekdahl C, Gard G. Early discharge to therapy-based rehabilitation at home in patients with stroke: a systematic review. Physical Therapy Reviews. 2008; 13(3):167–187
- 277.
- Wolfe CD, Tilling K, Rudd AG. The effectiveness of community-based rehabilitation for stroke patients who remain at home: a pilot randomized trial. Clinical Rehabilitation. 2000; 14(6):563–569 [PubMed: 11128729]
- 278.
- Wong C, X, Carson K, V, Smith BJ. Home care by outreach nursing for chronic obstructive pulmonary disease. Cochrane Database of Systematic Reviews. 2012; Issue 4:CD000994. DOI:10.1002/14651858.CD000994.pub3 [PMC free article: PMC7047940] [PubMed: 22513899] [CrossRef]
- 279.
- Wong FKY, Chau J, So C, Tam SKF, McGhee S. Cost-effectiveness of a health-social partnership transitional program for post-discharge medical patients. BMC Health Services Research. 2012; 12:479 [PMC free article: PMC3547766] [PubMed: 23259498]
- 280.
- Wong FKY, Ng AYM, Lee PH, Lam PT, Ng JSC, Ng NHY et al. Effects of a transitional palliative care model on patients with end-stage heart failure: a randomised controlled trial. Heart. 2016; 102(14):1100–1108 [PMC free article: PMC4941184] [PubMed: 26969631]
- 281.
- Wong RC, Tan PT, Seow YH, Aziz S, Oo N, Seow SC et al. Home-based advance care programme is effective in reducing hospitalisations of advanced heart failure patients: a clinical and healthcare cost study. Annals of the Academy of Medicine, Singapore. 2013; 42(9):466–471 [PubMed: 24162321]
- 282.
- Woodend AK, Sherrard H, Fraser M, Stuewe L, Cheung T, Struthers C. Telehome monitoring in patients with cardiac disease who are at high risk of readmission. Heart and Lung: Journal of Acute and Critical Care. 2008; 37(1):36–45 [PubMed: 18206525]
- 283.
- Woodhams V, de Lusignan S, Mughal S, Head G, Debar S, Desombre T et al. Triumph of hope over experience: learning from interventions to reduce avoidable hospital admissions identified through an Academic Health and Social Care Network. BMC Health Services Research. 2012; 12:153 [PMC free article: PMC3476394] [PubMed: 22682525]
- 284.
- Yoshida S, Miyashita M, Morita T, Akizuki N, Akiyama M, Shirahige Y et al. Strategies for development of palliative care from the perspectives of general population and health care professionals: a Japanese outreach palliative care trial of integrated regional model study. American Journal of Hospice and Palliative Care. 2015; 32(6):604–610 [PubMed: 24907123]
- 285.
- Young J, Green J. Effects of delays in transfer on independence outcomes for older people requiring postacute care in community hospitals in England. Journal of Clinical Gerontology and Geriatrics. 2010; 1(2):48–52
- 286.
- Young J, Sharan U. Medical assessment and direct admissions to a community hospital. Clinical Governance. 2003; 8(3):213–217
- 287.
- Young JB, Robinson M, Chell S, Sanderson D, Chaplin S, Burns E et al. A whole system study of intermediate care services for older people. Age and Ageing. 2005; 34(6):577–583 [PubMed: 16267182]
- 288.
- Young T, Busgeeth K. Home-based care for reducing morbidity and mortality in people infected with HIV/AIDS. Cochrane Database of Systematic Reviews. 2010; Issue 1:CD005417. DOI:10.1002/14651858.CD005417.pub2 [PubMed: 20091575] [CrossRef]
- 289.
- Yuan X, Tao Y, Zhao JP, Liu XS, Xiong WN, Xie JG et al. Long-term efficacy of a rural community-based integrated intervention for prevention and management of chronic obstructive pulmonary disease: a cluster randomized controlled trial in China’s rural areas. Brazilian Journal of Medical and Biological Research. 2015; 48(11):1023–1031 [PMC free article: PMC4671529] [PubMed: 26352697]
- 290.
- Zimmer JG, Groth-Juncker A, McCusker J. A randomized controlled study of a home health care team. American Journal of Public Health. 1985; 75(2):134–141 [PMC free article: PMC1645992] [PubMed: 3966617]
- 291.
- Zimmermann C, Swami N, Krzyzanowska M, Hannon B, Leighl N, Oza A et al. Early palliative care for patients with advanced cancer: a cluster-randomised controlled trial. The Lancet. 2014; 383(9930):1721–1730 [PubMed: 24559581]
Appendices
Appendix A. Review protocol
Table 7Review protocol: Community base palliative care
| Review question | Does community based palliative care improve outcomes compared with hospital care? |
|---|---|
| Guideline condition and its definition | Acute Medical Emergencies. Definition: a medical emergency can arise in anyone, for example, in people without a previously diagnosed medical condition, with an acute exacerbation of underlying chronic illness, after surgery or after trauma. |
| Objectives | To determine if wider provision of community-based intermediate care prevents people from staying in hospitals longer than necessary while not impacting on patient and carer outcomes. |
| Review population |
Adults and young people (16 years and over) with a suspected or confirmed AME or patients at risk of AME. |
|
Adults (17 years and above). Young people (aged 16-17 years). | |
| Line of therapy not an inclusion criterion. | |
|
Interventions and comparators: generic/class; specific/drug (All interventions will be compared with each other, unless otherwise stated) |
Usual Care. Community based palliative care; enhanced palliative care in community. Community based palliative care; standard palliative care in community. Hospital based palliative care. |
| Outcomes |
|
| Study design | Systematic reviews (SRs) of RCTs, RCTs, observational studies only to be included if no relevant SRs or RCTs are identified. |
| Unit of randomisation | Patient. |
| Crossover study | Permitted. |
| Minimum duration of study | Not defined. |
| Population stratification |
Early discharge. Admission avoidance. |
| Reasons for stratification | Each of them targets a separate outcome: early discharge would be primarily aimed at reducing length of stay, while admission avoidance would be primarily aimed at reducing hospital admission. Also, the population would be different as the admission avoidance group could be managed at home for the whole episode of care (they could be cared for at home from the start) while the early discharge group needs to be “stabilised” at hospital first then discharged. |
| Subgroup analyses if there is heterogeneity |
|
| Search criteria |
Databases: Medline, Embase, the Cochrane Library, CINAHL. Date limits for search: 2010 (update of the search for a Cochrane review106). Language: English language only. |
Appendix B. Clinical article selection
Appendix C. Forest plots
C.1. Community palliative care versus hospital care
Figure 4Number of presentations to ED (continuous)
Source: SDs are the same for each group because they were calculated from the p-value, mean and n in each group.
Figure 6Length of stay (SD calculated)
Source: SDs are the same for each group because they were calculated from the p-value, mean and n in each group.
Figure 8Patient satisfaction (continuous)
Source: SDs are the same for each group because they were calculated from the p-value, mean and n in each group.
Figure 10Carer satisfaction
Source: SDs are the same for each group because they were calculated from the p-value, mean and n in each group.
C.2. Enhanced palliative care versus standard palliative care
C.3. Community palliative care versus usual care
Figure 19Quality of life (functional assessment of chronic illness therapy spiritual wellbeing scale)
Appendix D. Clinical evidence tables
Download PDF (816K)
Appendix E. Economic evidence tables
Download PDF (434K)
Appendix F. GRADE tables
Table 8Clinical evidence profile: Community palliative versus hospital care
| Quality assessment | No of patients | Effect | Quality | Importance | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| No of studies | Design | Risk of bias | Inconsistency | Indirectness | Imprecision | Other considerations | Community Palliative care | Hospital care | Relative (95% CI) | Absolute | ||
| Place of death (assessed with: deaths at home) | ||||||||||||
| 5 | randomised trials | serious1 | no serious inconsistency | no serious indirectness | serious2 | none |
316/532 (59.4%) | 50% | RR 1.27 (1.11 to 1.45) | 135 more per 1000 (from 55 more to 225 more) |
⨁⨁◯◯ LOW | CRITICAL |
| Admissions to hospital (follow-up median 6 months; assessed with: number of admissions) | ||||||||||||
| 5 | randomised trials | very serious1 | serious3 | no serious indirectness | no serious imprecision | none |
368/593 (62.1%) | 58.7% | RR 0.87 (0.8 to 0.93) | 76 fewer per 1000 (from 41 fewer to 117 fewer) |
⨁◯◯◯ VERY LOW | IMPORTANT |
| Number of presentations to ED (follow-up 12 months; assessed with: ED visits) | ||||||||||||
| 1 | randomised trials | serious1 | no serious inconsistency | no serious indirectness | serious2 | none |
29/145 (20%) | 32.9% | RR 0.61 (0.41 to 0.9) | 128 fewer per 1000 (from 33 fewer to 194 fewer) |
⨁⨁◯◯ LOW | IMPORTANT |
| Number of presentations to ED (continuous) (measured with: ED visits; Better indicated by lower values) | ||||||||||||
| 1 | randomised trials | serious1 | no serious inconsistency | no serious indirectness | no serious imprecision | none | 145 | 134 | - | MD 0.23 higher (0.49 lower to 0.95 higher) |
⨁⨁⨁◯ MODERATE | IMPORTANT |
| Length of stay (follow-up 6 months; measured with: length of hospital stay; Better indicated by lower values) | ||||||||||||
| 3 | randomised trials | serious1 | serious3 | no serious indirectness | no serious imprecision | none | 357 | 320 | - | MD 1.77 lower (3.19 to 0.35 lower) |
⨁⨁◯◯ LOW | IMPORTANT |
| Length of stay (measured with: length of hospital stay; Better indicated by lower values) | ||||||||||||
| 1 | randomised trials | very serious1 | no serious inconsistency | no serious indirectness | no serious imprecision | none | 145 | 134 | - | MD 0.1 higher (0.03 lower to 0.23 higher) |
⨁⨁◯◯ LOW | IMPORTANT |
| Quality of life (follow-up 6 months; measured with: QoL-EQ5D (0-100 scale); Better indicated by higher values) | ||||||||||||
| 1 | randomised trials | serious1 | no serious inconsistency | no serious indirectness | serious2 | none | 36 | 36 | - | MD 8.1 higher (2.03 lower to 18.23 higher) |
⨁⨁◯◯ LOW | CRITICAL |
| Quality of life (follow-up 12 months; measured with: QoL- Functional assessment of chronic illness therapy (0-184 scale); Better indicated by higher values) | ||||||||||||
| 1 | randomised trials | serious1 | no serious inconsistency | no serious indirectness | serious2 | none | 27 | 31 | - | MD 3 higher (3.91 lower to 9.91 higher) |
⨁⨁◯◯ LOW | CRITICAL |
| Patient Satisfaction (follow-up 6 months; Better indicated by higher values) | ||||||||||||
| 1 | randomised trials | serious1 | no serious inconsistency | no serious indirectness | serious2 | none | 17 | 14 | - | MD 0.27 higher (0 to 0.54 higher) |
⨁⨁◯◯ LOW | CRITICAL |
| Patient satisfaction (follow-up 3 months) | ||||||||||||
| 1 | randomised trials | serious1 | no serious inconsistency | no serious indirectness | serious2 | none |
135/145 (93.1%) | 80.9% | RR 1.15 (1.05 to 1.26) | 121 more per 1000 (from 40 more to 210 more) |
⨁⨁◯◯ LOW | CRITICAL |
| Carer satisfaction (follow-up 6 months; measured with: scale 26-130; Better indicated by higher values) | ||||||||||||
| 1 | randomised trials | serious1 | no serious inconsistency | no serious indirectness | serious2 | none | 31 | 33 | - | MD 11 higher (4.32 to 17.68 higher) |
⨁⨁◯◯ LOW | CRITICAL |
| In-hospital mortality (follow up mean 18 months) | ||||||||||||
| 3 | randomised trials | serious1 | serious inconsistency3 | no serious indirectness | serious2 | none |
170/403 (42.2%) | 53.3% | RR 0.77 (0.67 to 0.88) | 123 fewer per 1000 (from 64 fewer to 176 fewer) |
⨁◯◯◯ VERY LOW | CRITICAL |
- 1
Downgraded by 1 increment if the majority of the evidence was at high risk of bias, and downgraded by 2 increments if the majority of the evidence was at very high risk of bias.
- 2
Downgraded by 1 increment if the confidence interval crossed 1 MID or by 2 increments if the confidence interval crossed both MIDs.
- 3
Heterogeneity, I2=50%, p=0.04, unexplained by subgroup analysis.
Table 9Clinical evidence profile: Enhanced community palliative versus standard community palliative care
| Quality assessment | No of patients | Effect | Quality | Importance | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| No of studies | Design | Risk of bias | Inconsistency | Indirectness | Imprecision | Other considerations | Enhanced palliative care | standard palliative care | Relative (95% CI) | Absolute | ||
| Admissions (Better indicated by lower values) | ||||||||||||
| 1 | randomised trials | serious1 | no serious inconsistency | no serious indirectness | serious2 | none | 24 | 27 | - | MD 0.2 lower (1.63 lower to 1.23 higher) |
⨁⨁◯◯ LOW | IMPORTANT |
| Number of presentations to ED (follow-up 12 months) | ||||||||||||
| 1 | randomised trials | no serious risk of bias | no serious inconsistency | no serious indirectness | very serious2 | none |
10/40 (25%) | 25% | RR 1 (0.47 to 2.14) | 0 fewer per 1000 (from 132 fewer to 285 more) |
⨁⨁◯◯ LOW | IMPORTANT |
| Length of stay (follow-up 6 months; Better indicated by lower values) | ||||||||||||
| 1 | randomised trials | serious1 | no serious inconsistency | no serious indirectness | very serious2 | none | 14 | 18 | - | MD 0.82 higher (12.36 lower to 14 higher) |
⨁◯◯◯ VERY LOW | IMPORTANT |
| Quality of life (measured with: QUAL-E End of life Scale; Better indicated by higher values) | ||||||||||||
| 1 | randomised trials | serious1 | no serious inconsistency | no serious indirectness | serious2 | none | 0 | - | - | MD 4.05 lower (11.49 lower to 3.38 higher) |
⨁⨁◯◯ LOW | CRITICAL |
| Preferred place of death achieved | ||||||||||||
| 1 | randomised trials | serious1 | no serious inconsistency | no serious indirectness | no serious imprecision | none |
429/688 (62.4%) | 61.90% | OR 0.95 (0.78 to 1.15) | 12 fewer per 1000 (from 60 fewer to 32 more) |
⨁⨁⨁◯ MODERATE | CRITICAL |
| Preferred place of death achieved | ||||||||||||
| 1 | randomised trials | serious1 | no serious inconsistency | no serious indirectness | serious2 | none |
7/8 (87.5%) | 76.9% | RR 1.14 (0.77 to 1.69) | 108 more per 1000 (from 177 fewer to 531 more) |
⨁⨁◯◯ LOW | CRITICAL |
- 1
Downgraded by 1 increment if the majority of the evidence was at high risk of bias, and downgraded by 2 increments if the majority of the evidence was at very high risk of bias.
- 2
Downgraded by 1 increment if the confidence interval crossed 1 MID or by 2 increments if the confidence interval crossed both MIDs.
Table 10Clinical evidence profile: Community palliative care versus usual care
| Quality assessment | No of patients | Effect | Quality | Importance | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| No of studies | Design | Risk of bias | Inconsistency | Indirectness | Imprecision | Other considerations | Community palliative care | usual care | Relative (95% CI) | Absolute | ||
| Quality of life (follow-up 3-4 months; measured with: Quality of life at end of life scale; range of scores: 21-105; Better indicated by higher values) | ||||||||||||
| 2 | randomised trials | no serious risk of bias | serious1 | no serious indirectness | no serious imprecision | none | 183 | 231 | - | MD 025 lower (1.03 lower to 0.53 higher) |
⨁⨁⨁◯ MODERATE | CRITICAL |
| Quality of life (follow-up 3-4 months; measured with: functional assessment of chronic illness therapy spiritual well-being scale; range of scores: 0-184; Better indicated by higher values) | ||||||||||||
| 2 | randomised trials | no serious risk of bias | no serious inconsistency | no serious indirectness | serious2 | none | 194 | 232 | - | MD 4.63 higher (1.53 to 7.73 higher) |
⨁⨁⨁◯ MODERATE | CRITICAL |
| Patient satisfaction (follow-up 4 months; measured with: overall satisfaction rating; range of scores: 1-10; Better indicated by higher values) | ||||||||||||
| 1 | randomised trials | very serious3 | no serious inconsistency | no serious indirectness | no serious imprecision | none | 21 | 17 | - | MD 1.4 higher (0.69 to 2.11 higher) |
⨁⨁◯◯ LOW | CRITICAL |
| Patient satisfaction (follow-up 4 months; measured with: FAMCARE patient satisfaction with care scale; range of scores: 16-80; Better indicated by higher values) | ||||||||||||
| 1 | randomised trials | no serious risk of bias | no serious inconsistency | no serious indirectness | serious2 | none | 121 | 153 | - | MD 6 higher (3.94 to 8.06 higher) |
⨁⨁⨁◯ MODERATE | CRITICAL |
| Relatives satisfaction (follow-up 4 months; measured with: overall satisfaction rating; range of scores: 1-10; Better indicated by lower values) | ||||||||||||
| 1 | randomised trials | very serious3 | no serious inconsistency | no serious indirectness | serious2 | none | 21 | 12 | - | MD 1.6 higher (0.19 to 3.01 higher) |
⨁◯◯◯ VERY LOW | CRITICAL |
| Death at home | ||||||||||||
| 1 | randomised trials | very serious3 | no serious inconsistency | no serious indirectness | serious2 | none |
27/50 (54%) | 47.5% | RR 1.14 (0.79 to 1.65) | 66 more per 1000 (from 100 fewer to 309 more) |
⨁◯◯◯ VERY LOW | CRITICAL |
| Length of stay (assessed with: rate of hospital days) | ||||||||||||
| 1 | randomised trials | very serious3 | no serious inconsistency | no serious indirectness | very serious2 | none |
0/50 (0%) | 0% | RR 0.73 (0.41 to 1.3) | - |
⨁◯◯◯ VERY LOW | IMPORTANT |
| ED visits | ||||||||||||
| 1 | randomised trials | very serious3 | no serious inconsistency | no serious indirectness | serious2 | none |
0/50 (0%) | 0% | RR 0.73 (0.45 to 1.19) | - |
⨁◯◯◯ VERY LOW | IMPORTANT |
| Readmissions (28 days) | ||||||||||||
| 1 | randomised trials | no serious risk of bias | no serious inconsistency | no serious indirectness | very serious2 | none |
9/43 (20.9%) | 29.3% | RR 0.72 (0.34 to 1.52) | 82 fewer per 1000 (from 193 fewer to 152 more) |
⨁⨁◯◯ LOW | IMPORTANT |
| Admissions (84 days) | ||||||||||||
| 1 | randomised trials | no serious risk of bias | no serious inconsistency | no serious indirectness | serious2 | none |
14/43 (32.6%) | 61% | RR 0.53 (0.33 to 0.88) | 287 fewer per 1000 (from 73 fewer to 409 fewer) |
⨁⨁⨁◯ MODERATE | IMPORTANT |
| Quality of life (28 days) (Chronic heart failure questionnaire; higher score is better) | ||||||||||||
| 1 | randomised trials | serious3 | no serious inconsistency | no serious indirectness | serious2 | none | 43 | 41 | - | MD 0.79 higher (0.23 to 1.35 higher) |
⨁⨁◯◯ LOW | CRITICAL |
- 1
Heterogeneity, I2=50%, p=0.04, unexplained by subgroup analysis.
- 2
Downgraded by 1 increment if the confidence interval crossed 1 MID or by 2 increments if the confidence interval crossed both MIDs.
- 3
Downgraded by 1 increment if the majority of the evidence was at high risk of bias, and downgraded by 2 increments if the majority of the evidence was at very high risk of bias.
Appendix G. Excluded clinical studies
Table 11Studies excluded from the clinical review (all excluded for alternative to hospital care)
| Reference | Reason for exclusion |
|---|---|
| Abernethy 20132 | Data presented ‘per patient’ and not overall |
| Addington-Hall 19923 | Incorrect intervention (co-ordinators did not provide “practical nursing care” or “specialist palliative care advice”; co-ordination only) |
| Adler 19784 | Not relevant: patients following elective surgery |
| Aimonino 20007 | Conference abstract; later published as Ricauda 2004213 |
| Aimonino 20016 | Patients not treated for acute medical emergency (advanced dementia patients) – please note not linked to Tibaldi 2004259 |
| Alcide 20158 | Systematic review is not relevant to review question or unclear PICO |
| Allen 19999 | Not RCT; description of a website |
| Anderson 2000A10 | Conference abstract of protocol only |
| Anderson 2002B11 | Not RCT; Systematic review |
| Anderson 2002A12 | No clinical outcomes; Costs only |
| Anonymous 1982B1 | Not relevant comparison |
| Aoun 201513 | Incorrect intervention (caregiver assessment tool intervention) |
| Armstrong 2008B14 | Not RCT; Retrospective single arm study |
| Aujesky 201115 | RCT but no community care (self- administered injections) |
| Bai 201316 | Not RCT; systematic review |
| Baidoobonso 201417 | Systematic review is not relevant to review question or unclear PICO |
| Bakken 201221 | No RCT; not relevant |
| Barnes 200322 | Not RCT; review |
| Beech 200423 | Not RCT; service evaluation |
| Bernhaut 200224 | Not RCT, service evaluation |
| Bethell 199025 | No substitute for usual care; control group received no intervention, only advice what exercises they could do by themselves |
| Beynon 200926 | Not RCT; literature review |
| Blackburn 200027 | Not RCT; not relevant; costs only |
| Blair 201128 | Not RCT; systematic review |
| Board 200029 | Not relevant; costs only |
| Booth 200430 | Not relevant; patients following bypass surgery |
| Boston 200131 | Not RCT; prospective non-randomised comparative study |
| Bove 201632 | Incorrect intervention (psychoeducative intervention) |
| Bowman 199833 | Not RCT; review |
| Brandt 201634 | Study protocol |
| Brooks 200236 | Not RCT; retrospective case study |
| Brooks 200337 | Not RCT; retrospective documentary analysis |
| Brown 201538 | Systematic review is not relevant to review question or unclear PICO |
| Brunner 200841 | Not RCT; other experimental design |
| Bryan 201042 | Not RCT; literature review |
| Bryant-lukosius 201543 | Systematic review is not relevant to review question or unclear PICO |
| Buus 201344 | Protocol only; no study data |
| Campbell 200145 | No clinical outcomes; costs only |
| Caplan 200646 | Not RCT; service evaluation |
| Caplan 201247 | Not RCT; systematic review |
| Caplan 200448 | Comparison is not hospital-based care |
| Carroll 200549 | Not RCT; review |
| Cassel 201050 | Not RCT; review |
| Chan 201151 | Not RCT; Cochrane review, but NO included studies as none met the criteria |
| Chan 201352 | Not RCT; Cochrane review, but NO included studies as none met the criteria |
| Chang 201653 | Incorrect study design |
| Chappell 199354 | Not relevant; retrospective cost analysis |
| Chard 200655 | Not RCT; review |
| Chen 2012A56 | Not relevant; costs associated with acquired brain injury |
| Chen 201557 | Incorrect study design |
| Chiang 201558 | Incorrect study design |
| Clark 200659 | Incorrect interventions (advanced cancer intervention, participants did not meet qualification for hospice or palliative services) |
| Coast 60 | Not relevant; majority of patients with trauma and elective surgery |
| Cobelli 199661 | Not RCT; review |
| Coburn 198962 | Not RCT; quasi-experimental; cost |
| Cohen 199463 | Not RCT; review |
| Colprim 201265 | Not RCT; quasi-experimental study |
| Colprim 201464 | Not RCT; prospective cohort study |
| Cowie 201466 | Not RCT; economic analysis |
| Craig 201467 | Not RCT; review |
| Crawford-Faucher 201068 | Not RCT; systematic review |
| Crotty 200272 | RCT but not relevant as trauma patients only (hip fracture) |
| Crotty 200070 | Not RCT; audit of trauma patients |
| Crotty 2000A69 | RCT but not relevant as trauma patients only (hip fracture) |
| Crotty 200371 | RCT but not relevant as trauma patients only |
| Cummings 199073 | Incorrect interventions (home care intervention; <50% patients were terminally ill) |
| Cunliffe 200274 | Not RCT; qualitative study; abstract only |
| Dalal 200375 | Not RCT; non-randomised prospective study |
| Daly 201376 | Intervention incorrect. Set in outpatient setting |
| Davis 201577 | Systematic review is not relevant to review question or unclear PICO |
| Deutsch 200678 | Not RCT; retrospective study |
| Dey79 | RCT; but unpublished data only. We have no access to paper and information in Cochrane review (Hospital at home early discharge) is insufficient to categorise the intervention |
| Dias 2013 80 | RCT but not relevant (does not compare to inpatient rehabilitation) |
| DiMartino 81 2014 | Not RCT; systematic review |
| Dolansky 201082 | Not RCT |
| Dombi 200983 | Not RCT; commentary on costs |
| Donaldson 198284 | Not RCT; retrospective study |
| Donath 200185 | Not RCT; Commentary |
| Donlevy 1996A86 | Not relevant; article is on cross-training to provide care at home on discharge |
| Donnelly 200287 | Not RCT; not relevant; questionnaire survey |
| Dorney-Smith 201188 | Not RCT; case study of the cost of nurse-led hostels for the homeless |
| Dow 200489 | Not RCT; case study |
| Dow 200790 | Not RCT; qualitative study |
| Duffy 201091 | RCT but wrong comparison (control group not in hospital) |
| Dyar 201292 | Incorrect intervention. Only discussions of end of life |
| Eldar 2000A93 | Not RCT; review |
| Elder 200194 | Not RCT; literature review |
| Emme 201495 | RCT; but no relevant outcomes |
| Emme 2014A96 | RCT; but no relevant outcomes |
| Engelhardt 200697 | No extractable outcomes |
| Eron 200498 | Not RCT; no data |
| Feltner 201499 | Not RCT; systematic review |
| Ferrell 2015100 | Incorrect study design |
| Fischer 2015101 | No relevant outcomes |
| Gaspoz 1994102 | Not RCT; prospective cohort study |
| Glasby 2008103 | Not RCT; qualitative study |
| Glick 1998104 | Not relevant – observing outcome of aneurysmal subarachnoid haemorrhage |
| Gobbi 2004105 | Not RCT; and not relevant |
| Gracey 1992107 | Not RCT; case studies |
| Graham 2013108 | Not RCT; description of organisation of rehabilitation services |
| Grande 2004109 | RCT on bereavement. Not relevant. |
| Graverholt 2014 112 | Not RCT; review |
| Greer 2012113 | Intervention incorrect and no outcomes that match protocol |
| Gregory 2010114 | Not RCT; Cross-sectional study |
| Gregory 2009115 | Not RCT; retrospective study |
| Griffiths 2000118 | Not RCT; exploratory analyses |
| Griffiths 2005121 | Not RCT; systematic review |
| Griffiths 2001117 | RCT but not relevant comparison; both arms in-patient care (nurse led versus consultant managed) |
| Griffiths 2006A116 | Not RCT; review |
| Griffiths 2006120 | Not RCT; review |
| Griffiths 2000A119 | RCT but not relevant comparison (in-patients only) |
| Gunnell 2000122 | Not relevant; majority of patients with trauma and elective surgery |
| Hamlet 2010123 | Not RCT; uses secondary data. Focus is telemedicine |
| Hannan 2003124 | Not RCT |
| Hardy 2001126 | Not RCT; description of a service; and mainly trauma patients |
| Hansen 1992125 | Cochrane excluded list: Hospital at home early discharge (study did not evaluate hospital at home, but a model for follow-up visits at home after discharge from hospital) |
| Hauser 1991127 | Not RCT; retrospective study |
| Herr 2012128 | Not RCT; retrospective study |
| Heseltine 2001129 | Not RCT; review on cost |
| Hill 1978131 | RCT but not relevant to today’s approach of managing MI as thrombolytic therapy made admission necessary (Cochrane) |
| Hudson 2013133 | Incorrect intervention; preparation of caregivers for home palliative acre with education and discussion |
| Hudson 2013134 | Incorrect intervention; preparation of caregivers for home palliative acre with education and discussion |
| Hughes 1990136 | RCT but has wrong comparison (not in hospital) |
| Hughes 2000137 | Incorrect interventions (home based primary care intervention; only 20% of patients were terminally ill) |
| Huo 2014138 | Not RCT; retrospective study. No outcomes of interest |
| Hwang 2013139 | Not RCT; observational study. Large sample, but set in Taiwan |
| Indredavik 1999140 | No RCT and compares stroke unit rehabilitation with general medical ward treatment |
| Indredavik 2008141 | RCT but no relevant outcomes |
| Jakobsen 2013142 | Methodology of RCT only |
| Johnston 2015143 | Systematic review is not relevant to review question or unclear PICO |
| Jolly 2005144 | RCT but study aborted prematurely due to language barriers with participants. No data |
| Jones 1999145 | Costs only |
| Jones 2014146 | Not RCT; case study with little data |
| Kane 1984148 | Incorrect intervention (intensive hospice care delivered by a hospice unit of a hospital versus usual hospital care) |
| Kenny 2002149 | Not RCT and not relevant |
| Kinley 2014150 | Not RCT; retrospective observational study |
| Konrad 2012151 | Not RCT; retrospective study |
| Koopman 1996152 | RCT but excluded as home care was self-administered |
| Kornowski 1995153 | Not RCT; observational study |
| Kortke 2006154 | Not RCT; open clinical study (non-randomised) |
| Korzeniowska-Kubacka 2014155 | Not RCT; prospective observational study |
| Langhorne 2000156 | Cochrane systematic review withdrawn from publication and superseded by Shepperd 2008240 |
| Langhorne 2005157 | Not RCT; review |
| Lappegard 2012158 | Not RCT; retrospective study |
| Last 2000159 | Not RCT, service description |
| Leon 2011160 | RCT, but patient group and outcomes not relevant (stable HIV patients) |
| Leppert 2014161 | Not RCT |
| Lewis 2007162 | Not RCT; commentary |
| Lewis 2011163 | Not RCT; research protocol only |
| Lewis 2012165 | Not RCT; commentary/conceptual paper |
| Lewis 2013164 | Not RCT; case studies without data |
| Lewis 2013166 | Not RCT; propensity matched controls study based on observational study data |
| Lim 2003167 | RCT but not relevant comparison |
| Linertova 2011168 | Not RCT; Systematic review |
| Luckett 2013169 | Systematic review: study designs inappropriate |
| Martin 1994170 |
RCT but wrong comparison (control group received ‘appropriate conventional community services) – Cochrane (early discharge) says it is in-hospital but I checked paper -to be included into district nurse section – |
| Mason 2003171 | Not RCT; description of a service |
| Mather 1976172 | No description of the type of service patients at home received (excluded by Cochrane too) |
| Matukaitis 2005173 | Not RCT. Pilot study and no comparison study |
| Mayhew 2006174 | Not RCT; health economics only |
| Mayo 1998175 | Conference abstract of study protocol only; duplicate of full paper Mayo 2000176 |
| McKegney 1981178 | No outcomes of interest |
| Mcloughlin 2015179 | Study protocol |
| Mcmillan 2006181 | Incorrect interventions (caregiver intervention); no relevant outcomes (caregiver outcomes) |
| Mcmillan 2007180 | Incorrect interventions and comparison (caregiver intervention versus usual care in the same setting (hospice)) |
| McNamee 1998182 | Health economic evaluation |
| McWhinney 1994183 | No outcome data reported. Authors describe the challenges of conducting a trail in this area |
| Melin 1992184 | Not relevant: patients with long-term care needs were recruited. Hospital at Home was substitute for long-term care and not necessarily in-hospital |
| Meyer 2009185 | Not RCT; case studies |
| Meyers 2011186 | Incorrect intervention (education) |
| Miller 2005187 | No relevant outcomes |
| Molassiotis 2009188 | Incorrect interventions (home care nursing intervention for symptom management in patients receiving oral chemotherapy) |
| Muijen 1992189 | RCT but patients treated for acute, severe mental illness (psychiatric ward versus home); not relevant to AME guideline |
| Nicholson 2001190 | Health economics only |
| Nissen 2007191 | Not in English (Danish) |
| Nordly 2014192 | Protocol only; no study data |
| Nordly 2016193 | Systematic review (included incorrect study design) |
| Nyatanga 2014194 | Not RCT; commentary/conceptual paper |
| Palmer Hill 2000197 | Not relevant: patients recovering from knee replacement |
| Pandian 2013198 | Trial register only; no data |
| Patel 2004199 | Health economic evaluation |
| Penque 1999200 | Not RCT; retrospective study |
| Pergolotti 2015201 | Study protocol |
| Pirl 2012202 | No relevant outcomes |
| Pittiglio 2011203 | Not RCT; not relevant |
| Plant 2015204 | Incorrect interventions (coordination of care intervention for patients with chronic conditions) |
| Plochg 2005205 | Not RCT; process evaluation |
| Pozzilli 2002206 | RCT BUT not relevant (Multiple Sclerosis patients) |
| Prior 2012 207 | Not RCT |
| Puig-Junoy 2007208 | Health economic evaluation |
| Rabow 2004209 | Incorrect study design |
| Raftery 1996211 | Incorrect intervention (co-ordinators did not provide “practical nursing care” or “specialist palliative care advice”; co-ordination only) |
| Raphael 2015212 | Inappropriate comparison (no comparator) |
| Richards 1998 215 | Not relevant; majority of patients with trauma and elective surgery |
| Richards 1998A214 | Not relevant; correction to excluded trial with majority of patients with trauma and elective surgery |
| Richardson 2001 216 | Health economic evaluation |
| Robinson 2009217 | Not RCT; description of new model of acute care |
| Rodriguez-Cerrillo 2010219 | Not RCT; Non-randomised prospective study |
| Rodriguez-Cerrillo 2012A218 | Not RCT; no comparison group to home treatment |
| Round 2004221 | Not RCT; prospective cohort study |
| Rosbotham-Williams 2002220 | Not RCT; review |
| Rout 2011222 | Not RCT; review |
| Rowley 1984223 | Not RCT. No comparison group |
| Ruckley 1978224 | Not relevant: patients following elective surgery |
| Rudkin 1997225 | No service provided in community |
| Rummans 2006226 | Incorrect interventions (advanced cancer intervention, participants did not meet qualification for hospice or palliative services) |
| Sahlen 2016227 | No relevant outcomes |
| Sartain 2002228 | Paediatric patient population |
| Saysell 2004229 | Not RCT; pilot study of intermediate palliative care in care home |
| Schachter 2014230 | Not RCT; study protocol only |
| Scheinberg 1986231 | RCT but does not state what the control group intervention is |
| Schneller 2012232 | Not RCT; case study |
| Schou 2014233 | RCT; but no relevant outcomes |
| Scott 2010234 | Not RCT; literature review |
| Senaratne 1999235 | Cost evaluation |
| Seow 2016236 | Non-RCT; cohort study |
| Subirana Serrate 2001250 | Not RCT; health economics evaluation |
| Shepperd 1998239 | Not RCT; systematic review |
| Shepperd 2005A237 | Not RCT; editorial |
| Shepperd 2009A241 | Not RCT; systematic review |
| Shepperd 1998A238 | Costs only; no clinical outcomes |
| Sidebottom 2015244 | In-patient care only considered. No alternative. |
| Singh 2015245 | Systematic review is not relevant to review question or unclear PICO |
| Stephenson 1984246 | Not RCT; conceptual paper |
| Steventon 2012247 | Not RCT; retrospective analysis |
| Stewart 1999248 | RCT but control group not in hospital. |
| Stromberg 2003249 | RCT but only nurse-led follow up appointments in hospital. No actual community care given |
| Suijker 2012251 | Protocol only; incorrect intervention |
| Suwanwela 2002252 | RCT but not comparable to UK setting as home treatment was managed by Red Cross Volunteers and family members (Thailand) |
| Temel 2010254 | Incorrect intervention (outpatient meetings with patients at a large academic medical centre; not specifically aimed to support patients or caregivers at home) |
| Teng 2003255 | Health economic evaluation |
| Tibaldi 2004259 | RCT but no relevant outcomes (carer stress data incomplete) |
| Thorne 2001256 | Not RCT; service description |
| Toseland 1995260 | Incorrect interventions (intervention for caregivers of patients prior to the terminal stage of illness) |
| Trappes-Lomax 2006261 | RCT but comparison group not appropriate; did not receive ‘usual’ hospital care. |
| Upton 2014264 | No RCT; not relevant |
| Utens 2010265 | Study protocol of RCT only |
| Van hout 2005266 | Incorrect interventions (frail elderly care, not palliative care) |
| Ventura 2016267 | Abstract (Cochrane review already included) |
| Walshe 2010 271 | Not RCT; review of qualitative papers |
| Wakefield 2008270 | RCT but all self-care; wrong comparison |
| Weber 2014272 | Study protocol |
| Widen Holmqvist 1996274 | Health economic evaluation |
| Widen Holmqvist 1995273 | Not RCT; observational study |
| Widen-Holmqvist 1998275 | Superseded by Thorsen 2005 257, 2006258 and Von Koch 2000269,2001268 |
| Winkel 2008276 | Not RCT; systematic review |
| Wolfe 2000277 | RCT but excluded from Cochrane because intervention does not substitute for inpatient care; not valid comparison |
| Woodend 2008282 | RCT but wrong control group; both at home with no actual care provided. |
| Woodhams 2012283 | Not RCT; literature review |
| Yoshida 2015284 | Incorrect study design |
| Young 2003B286 | Not RCT; audit |
| Young 2005B287 | Not RCT; quasi-experimental study |
| Young 2010B285 | RCT but not relevant outcomes |
| Young 2010288 | Incorrect intervention; not palliative |
| Yuan 2015289 | Incorrect interventions (early prevention and management of COPD) |
Appendix H. Excluded economic studies
Table 12Studies excluded from the economic review
| Reference | Reason for exclusion |
|---|---|
| Pace 2014196 | This study was selectively excluded as it was conducted in a non-UK setting and does not report any health outcomes. It only looks at costs related re-hospitalisation and is based on observational evidence. |
| Shnoor 2007243 | This study was excluded as it was conducted in a non-UK setting using costs from 2003 and does not report any health outcomes. It was also based on observational evidence. Given a UK RCT cost effectiveness study was included it was felt more appropriate and relevant evidence was available for this review question. |
| Tamir 2007253 | This study was excluded as it was conducted in a non-UK setting using costs from the year 2000 and does not report any health outcomes. |
| Tzala 2005262 | This study was assessed as partially applicable with potentially serious limitations. However, the committee judged that the treatment included in the intervention and comparators was for a specific population, and therefore this study was selectively excluded. |
Appendix I
This appendix is not available from the publisher at this time.
- Community palliative care - Emergency and acute medical care in over 16s: servic...Community palliative care - Emergency and acute medical care in over 16s: service delivery and organisation
Your browsing activity is empty.
Activity recording is turned off.
See more...