NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
National Guideline Centre (UK). Emergency and acute medical care in over 16s: service delivery and organisation. London: National Institute for Health and Care Excellence (NICE); 2018 Mar. (NICE Guideline, No. 94.)

Emergency and acute medical care in over 16s: service delivery and organisation.
Show details32. Structured patient handovers
32.1. Introduction
Handover is the system by which the responsibility for immediate and ongoing care is transferred between healthcare professions. Changing work patterns mean that establishing standards for handover “should be a priority”.102
Although the process of handing over between shifts has been embedded in nursing practice for many years, the changing patterns of work in the hospital setting mean that there may be different medical teams looking after groups of patients across a 24 hour period. The medical and nursing professions both recognise the importance of effective handover between shifts and between health care professionals;
“Incomplete or delayed information can compromise safety, quality and the patient’s experience of health care.”78
The Royal College of Nursing dedicate a section of The Principles of Nursing Practice101 to communication and reporting stating;
“Evidence suggests that communication improves when nursing handover involves the patient and is carried out using a structured reporting format.”70,116
The World Health Organisation goes as far as to recommend the use of SBAR (Situation, Background, Assessment, Recommendation) as a tool to standardise handover communications.125 It is recognised in the literature that one system does not fit all settings and that local adaptations may be needed.
Despite the evidence and apparent agreement that handovers are improved by following a structure, the Royal College of Physicians make further recommendations which suggest that there are still improvements to be made and that this is not yet standard practice in all areas.
“Improvement and standardisation of handover are vital keys to improvement in efficiency, patient safety, and patient experience. There is a need to define common core principles for handover, which can be adapted locally. For example, a standardised proforma for written handover is essential, preferably in conjunction with face-to-face verbal handover. Furthermore, in the current technological climate, where possible, electronic handover processes should be encouraged.”102
Although the evidence to date points to the value of structured patient handover, there may be cost implications for services if there is a need for change in shift pattern and an overlap required to allow time for handover. It is therefore important to investigate the most appropriate form of handover for best patient outcomes and the impact this may have on services.
32.2. Review question: Do structured patient handovers between healthcare professionals improve outcomes?
For full details see review protocol in Appendix A.
Table 1
PICO characteristics of review question.
32.3. Clinical evidence
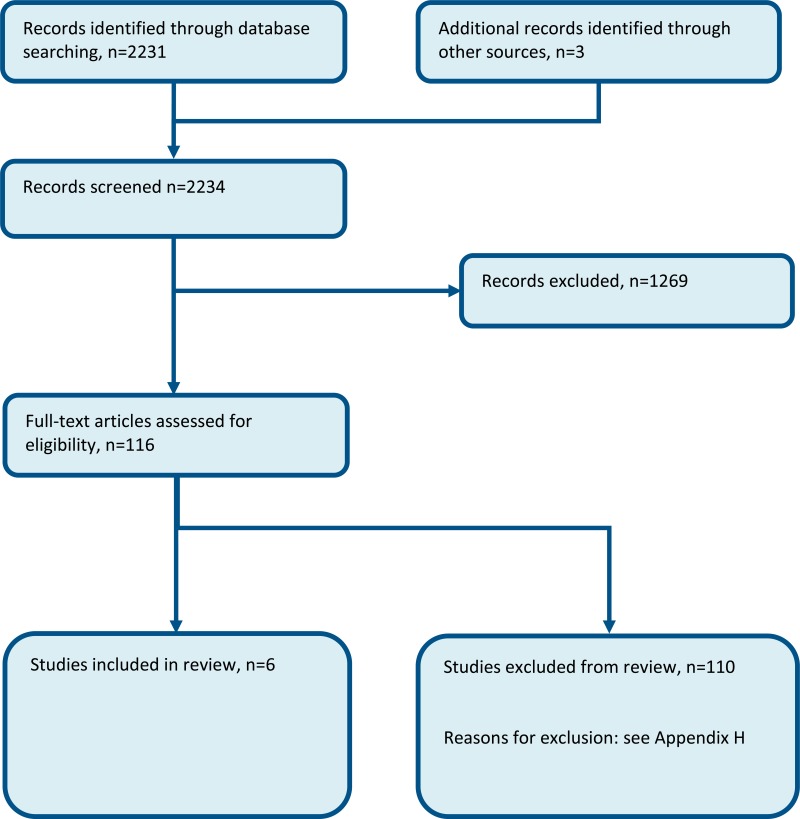
Six studies were included in the review; 1 non-randomised controlled study and 5 before-after studies20,34,42,46,58,127 and these are summarised in Table 2 below. Evidence from these studies is summarised in the GRADE clinical evidence profile/clinical evidence summary below. See also the study selection flow chart in Appendix B, study evidence tables in Appendix D, forest plots in Appendix C, GRADE tables in Appendix F and excluded studies list in Appendix G.
Table 2
Summary of studies included in the review.
Table 3
Clinical evidence summary: Intensive Care Unit.
Table 4
Clinical evidence summary: Neurological Care Unit.
Table 5
Clinical evidence summary: Emergency Department.
Table 6
Clinical evidence summary: Internal Medicine.
32.4. Economic evidence
Published literature
One economic evaluation was identified with the relevant comparison and has been included in this review.126 This study is summarised in the economic evidence profile below (Table 7) and the economic evidence tables in Appendix E.
Table 7
Economic evidence profile: Structured patient handover versus usual care.
The economic article selection protocol and flow chart for the whole guideline can found in the guideline’s Appendix 41A and Appendix 41B.
32.5. Evidence statements
Clinical
Intensive care unit
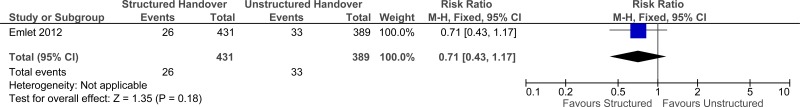
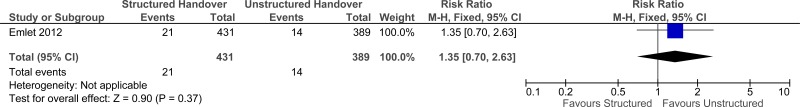
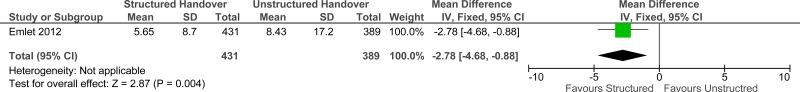
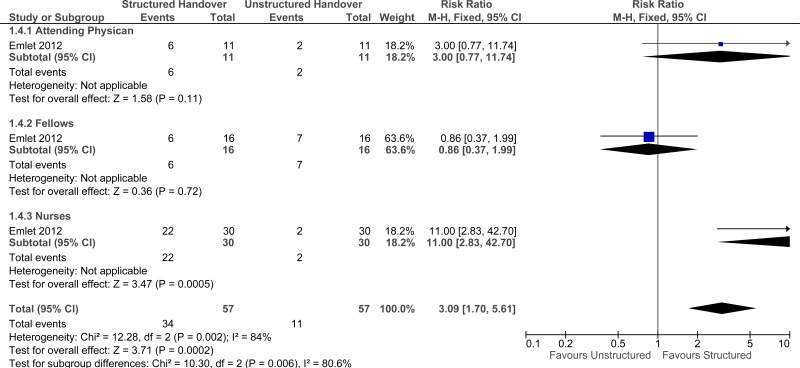
One study comprising 820 people evaluated the role of structured patient handover within the intensive care unit setting for improving outcomes in secondary care in adults and young people at risk of an AME, or with a suspected or confirmed AME. The evidence suggested that structured patient handovers provide a benefit in reduced mortality, length of stay and improved staff satisfaction (overall, nurse satisfaction and attending physician). However, the evidence suggested there was no effect on readmission (very low quality for all outcomes) and a reduction in staff satisfaction by fellows.
Neurointensive care unit
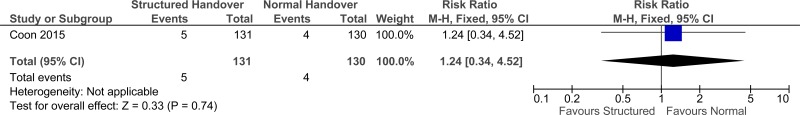
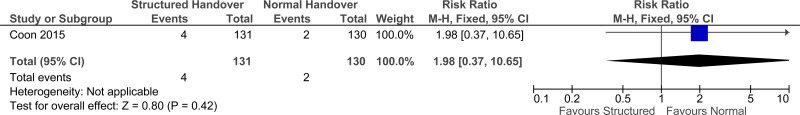
One study comprising 261 people evaluated the role of structured patient handover within the neurointensive care unit setting for improving outcomes in secondary care in adults and young people at risk of an AME, or with a suspected or confirmed AME. The evidence suggested that structured patient handovers have no effect on ICU readmission and avoidable adverse events defined as rapid response team call at 6 months (very low quality for both outcomes).
Emergency department
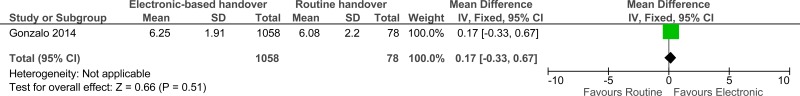
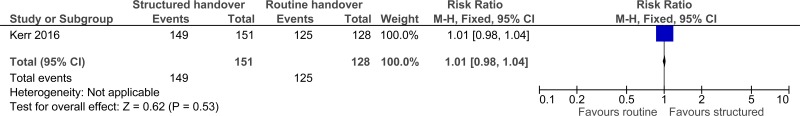
Two studies comprising 1415 people evaluated the role of structured patient handover within the emergency department setting for improving outcomes in secondary care in adults and young people at risk of an AME, or with a suspected or confirmed AME. The evidence suggested that structured patient handovers have no effect on staff satisfaction (1 study, very low quality) or avoidable adverse events defined as medications not administered as prescribed (1 study, very low quality).
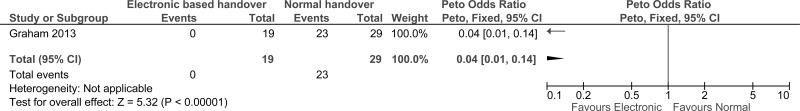
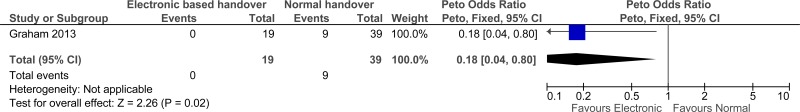
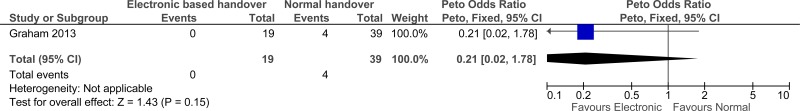
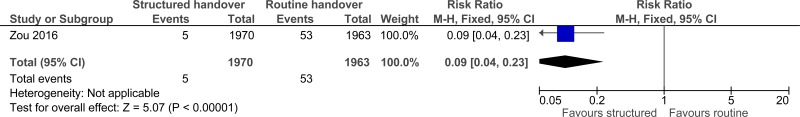
Internal medicine
Two studies comprising 3991 people evaluated the role of structured patient handover within the internal medicine setting for improving outcomes in secondary care in adults and young people at risk of an AME, or with a suspected or confirmed AME. The evidence suggested that structured patient handovers may provide a benefit in reduced avoidable adverse events defined as critical data omissions, near misses, adverse events and handoffs related errors (1 study, very low quality).
Economic
One cost-utility analysis found that structured handover was cost effective compared to usual care for patients discharged from hospital to the community (ICER: £180 per QALY gained). This analysis was assessed as partially applicable with potentially serious limitations.
32.6. Recommendations and link to evidence
| Recommendations |
|
| Research recommendations | - |
| Relative values of different outcomes | Mortality, avoidable adverse events (including prescribing errors, errors of omission, cardiopulmonary resuscitation, unplanned admission to intensive care, delayed or missed investigations and delayed or missed treatment), patient and/or carer satisfaction, length of stay and quality of life were considered critical outcomes by the guideline committee. Staff satisfaction was considered an important outcome by the committee. |
| Trade-off between benefits and harms |
Six studies were considered in the clinical review. The committee noted the variation in interventions and heterogeneity in how the intervention was delivered (that is, some were structured electronic forms while other studies just documented a handover process). Therefore, the results for each study were presented by setting and not meta-analysed. Mixed medical and Surgical ICU The evidence suggested that structured patient handovers may provide a benefit in reduced mortality, length of stay, improved senior clinical staff satisfaction and nurse satisfaction. The evidence suggested there was no effect on readmission and a reduced staff satisfaction for fellows. The group discussed the decreased staff satisfaction of junior doctors (compared to senior doctors and nurses) with a structured handover but suggested that this may be due to the imbalanced amount of time placed on junior doctors in the handover process. Overall, the evidence suggested a benefit of structured patient handover in the intensive care unit setting. There was no evidence for quality of life or patient and/or carer satisfaction. Neurological care unit The evidence suggested that structured patient handovers have no effect on readmission and avoidable adverse events defined as a rapid response team. The committee noted that this evidence was from 1 small study reporting for 1 unit and both outcomes were very low quality. There was no evidence for mortality, quality of life, patient and/or carer satisfaction, staff satisfaction or length of stay. Emergency department The evidence suggested that structured patient handovers have no effect on staff satisfaction or avoidable adverse events defined as medications not administered as prescribed. There was no evidence for mortality, quality of life, patient and/or carer satisfaction or length of stay. Internal Medicine The evidence suggested that structured patient handovers may provide a benefit in reduced avoidable adverse events defined as critical data omissions, near misses, adverse events and handoffs-related errors. The committee discussed the reductions in avoidable adverse events with the structured handover and suggested this may be due to the multi-factorial nature of the intervention. In this case it was a verbal (face-to-face) handover with an electronic sign-off sheet compared to no structured handover. There was no evidence for mortality, quality of life, patient and/or carer satisfaction, staff satisfaction or length of stay. Overall, the committee considered that structured handovers were associated with improvement in patient outcomes and staff satisfaction and should be part of current patient care. They discussed the evidence with regards to their own clinical experience and decided to support a strong recommendation for structured handovers for an AME population. They noted that while structured handovers could become a ‘tick box’ process and could lead to reduced communication both between healthcare professionals and with patients, when conducted properly a formal structure for exchanging information would improve outcomes. The committee discussed the best type of structured handover but the evidence was not strong enough to make a recommendation on a particular handover model. |
| Trade-off between net effects and costs |
A single study conducting a cost-utility analysis was included. The intervention included an online database with handover tools, shared staff experience of handovers and online staff training. As well as the online resource, the intervention required staff time to undertake classroom education in patient handovers. The study showed structured patient handovers between the hospital and community are cost-effective at £180 per QALY, significantly under the £20,000 threshold. Quality of life was not measured in a trial. Instead quality of life scores were estimated by categorising adverse events into groups and assigning the groups to an indicative state. However, the committee felt that the intervention would have low costs and for this reason, it would only need to have a small benefit to be cost-effective. There was evidence for this in the analysis, with the study showing the intervention only needing to be 1.6% effective at reducing preventable adverse events to be cost-effective. The transition between hospital and community would most likely involve more intensive handovers than those within a hospital. Therefore, the cost-effectiveness results might be extrapolated to other areas of patient handover, such as between staff members or shifts, wards and different hospitals. There was no evidence around the type of structured patient handover, for example, electronic, paper or verbal. It seems unlikely that there would be a large difference in the cost-effectiveness of the different structures. However, there was evidence in the clinical review of change in resource use for structured patient handover. One study outlined a change in shift patterns, increasing the shift duration of junior doctors to undertake structured handovers and adding further costs to the intervention. There was also evidence that structured handovers reduced the length of stay for patients in the ICU, freeing up resources and decreasing costs as a result of the intervention. The committee concluded that there may be an increase in staff time associated with structured handover but this would potentially be offset by reduced length of stay and clinical errors avoided. |
| Quality of evidence |
Clinical evidence For all comparisons the clinical evidence was considered to be very low quality due to the study type (observational or before and after), risk of bias (outcome reporting) and imprecision. In particular, the subgroup noted the composite outcomes reported as adverse effects and how these were reported poorly by most studies. Economic evidence The included economic study was deemed partially applicable because resource use and costs were from the Netherlands. It was also assessed to have potentially serious limitations because the effectiveness of the intervention was elicited from experts, rather than being based on a trial. |
| Other considerations |
The committee noted that electronic systems for patient handovers could provide benefits in terms of documenting and identifying trends, in data analysis and audit, sharing information between different members of the multidisciplinary team, and in preserving patient confidentiality. Important contextual modifiers may include training, shift length and the quality of electronic systems. The Professional Record Standards body48 has published clinical standards for electronic systems for patient handovers to ensure consistency and interoperability. The committee highlighted that structured handover of care between transferring and receiving teams is well established within NHS current practice and is reinforced by related NICE guidance (CG50)15 and the Acute Care RCP Toolkit.102 Currently, structured handover practice takes place through a range of methods including updated written lists, electronic and verbal face-to-face and this varies between departments and hospitals. However, standardisation across trusts is not common and would be difficult to implement. It is also important to understand that the ability to deliver a structured handover does not come naturally and training is vital to ensure that the benefits are realised. Handover is not just a simple matter of imparting information. It is about providing the required information in a format that is useful and beneficial to patient care. One key issue in the training is to ensure staff understand the importance of a good handover in delivering good patient care. Electronic systems would entail some training, resources to obtain and modify or develop the system and a change in the nature of the shift. The committee noted that it is important to provide a structured handover between primary and secondary care as this is a point of escalation and that this may require different emphasis and amount of information. Therefore, there was scope for further research in this area covering the bridge between secondary and primary care. |
References
- 1.
- Evidence appraisal of Salzwedel C, Bartz HJ, Kuhnelt I, et al. The effect of a checklist on the quality of post-anaesthesia patient handover: a randomized controlled trial.: Int J Qual Health Care. 2013;25(2):176–181. AORN Journal. 2016; 104(2):174-179 [PubMed: 27472978]
- 2.
- Abraham J, Kannampallil T, Patel B, Almoosa K, Patel VL. Ensuring patient safety in care transitions: an empirical evaluation of a Handoff Intervention Tool. AMIA. 2012;17–26 [PMC free article: PMC3540511] [PubMed: 23304268]
- 3.
- Abraham J, Kannampallil T, Patel VL. A systematic review of the literature on the evaluation of handoff tools: implications for research and practice. Journal of the American Medical Informatics Association. 2014; 21(1):154–162 [PMC free article: PMC3912721] [PubMed: 23703824]
- 4.
- Abraham J, Kannampallil TG, Almoosa KF, Patel B, Patel VL. Comparative evaluation of the content and structure of communication using two handoff tools: implications for patient safety. Journal of Critical Care. 2014; 29(2):311–317 [PubMed: 24360818]
- 5.
- Ah-Kye L, Moore M. A simple prioritisation system to improve the electronic handover. BMJ Quality Improvement Reports. 2015; 4(1) [PMC free article: PMC4693058] [PubMed: 26734404]
- 6.
- Ahmed J, Mehmood S, Rehman S, Ilyas C, Khan LUR. Impact of a structured template and staff training on compliance and quality of clinical handover. International Journal of Surgery. 2012; 10(9):571–574 [PubMed: 22983018]
- 7.
- Anderson J, Malone L, Shanahan K, Manning J. Nursing bedside clinical handover - an integrated review of issues and tools. Journal of Clinical Nursing. 2015; 24(5-6):662–671 [PubMed: 25319724]
- 8.
- Arora VM, Manjarrez E, Dressler DD, Basaviah P, Halasyamani L, Kripalani S. Hospitalist handoffs: a systematic review and task force recommendations. Journal of Hospital Medicine. 2009; 4(7):433–440 [PMC free article: PMC3575739] [PubMed: 19753573]
- 9.
- Barnes SL, Campbell DA, Stockman KA, Wunderlink D. From theory to practice of electronic handover. Australian Health Review. 2011; 35(3):384–391 [PubMed: 21871202]
- 10.
- Berkenstadt H, Haviv Y, Tuval A, Shemesh Y, Megrill A, Perry A et al. Improving handoff communications in critical care: utilizing simulation-based training toward process improvement in managing patient risk. Chest. 2008; 134(1):158–162 [PubMed: 18628218]
- 11.
- Blaz JW, Staggers N. The format of standard tools for nursing handoff: an integrative review. Nursing Informatics. 2012; 2012:23 [PMC free article: PMC3799142] [PubMed: 24199041]
- 12.
- Bost N, Crilly J, Wallis M, Patterson E, Chaboyer W. Clinical handover of patients arriving by ambulance to the emergency department - a literature review. International Emergency Nursing. 2010; 18(4):210–220 [PubMed: 20869662]
- 13.
- Brown E, Jarrett H, Churchhouse G, Hartley M, Cohen D, Kyprianou K et al. Improving phlebotomy handover of untaken blood tests to junior doctors. BMJ Quality Improvement Reports. 2015; 4(1) [PMC free article: PMC4693092] [PubMed: 26734434]
- 14.
- Bump GM, Bost JE, Buranosky R, Elnicki M. Faculty member review and feedback using a sign-out checklist: improving intern written sign-out. Academic Medicine. 2012; 87(8):1125–1131 [PubMed: 22722359]
- 15.
- Centre for Clinical Practice at NICE. Acutely ill patients in hospital: recognition of and response to acute illness in adults in hospital. NICE clinical guideline 50. London. National Institute of Health and Clinical Excellence, 2007. Available from: http://guidance
.nice.org.uk/CG50 [PubMed: 21204323] - 16.
- Christie P, Robinson H. Using a communication framework at handover to boost patient outcomes. Nursing Times. 2009; 105(47):13–15 [PubMed: 20063616]
- 17.
- Chu ES, Reid M, Schulz T, Burden M, Mancini D, Ambardekar AV et al. A structured handoff program for interns. Academic Medicine. 2009; 84(3):347–352 [PubMed: 19240442]
- 18.
- Cohen MD, Hilligoss PB. The published literature on handoffs in hospitals: deficiencies identified in an extensive review. Quality and Safety in Health Care. 2010; 19(6):493–497 [PubMed: 20378628]
- 19.
- Collins SA, Stein DM, Vawdrey DK, Stetson PD, Bakken S. Content overlap in nurse and physician handoff artifacts and the potential role of electronic health records: a systematic review. Journal of Biomedical Informatics. 2011; 44(4):704–712 [PMC free article: PMC3119775] [PubMed: 21295158]
- 20.
- Coon EA, Kramer NM, Fabris RR, Burkholder DB, Klaas JP, Graff-Radford J et al. Structured handoff checklists improve clinical measures in patients discharged from the neurointensive care unit. Neurology: Clinical Practice. 2015; 5(1):42–49 [PMC free article: PMC5764427] [PubMed: 29443183]
- 21.
- Cornell P, Gervis MT, Yates L, Vardaman JM. Impact of SBAR on nurse shift reports and staff rounding. Medsurg Nursing. 2014; 23(5):334–342 [PubMed: 26292447]
- 22.
- Craig SR, Smith HL, Downen AM, Yost WJ. Evaluation of patient handoff methods on an inpatient teaching service. Ochsner Journal. 2012; 12(4):331–337 [PMC free article: PMC3527860] [PubMed: 23267259]
- 23.
- Curtis O, Fisher R. Improving medical SHO weekend handover at a tertiary referral centre. BMJ Quality Improvement Reports. 2013; 2(1) [PMC free article: PMC4652704] [PubMed: 26734174]
- 24.
- Dawson S, King L, Grantham H. Review article: Improving the hospital clinical handover between paramedics and emergency department staff in the deteriorating patient. EMA - Emergency Medicine Australasia. 2013; 25(5):393–405 [PubMed: 24099367]
- 25.
- Dhillon P, Murphy RKJ, Ali H, Burukan Z, Corrigan MA, Sheikh A et al. Development of an adhesive surgical ward round checklist: a technique to improve patient safety. Irish Medical Journal. 2011; 104(10):303–305 [PubMed: 22256442]
- 26.
- Dixon JL, Stagg HW, Wehbe-Janek H, Jo C, Culp WCJ, Shake JG. A standard handoff improves cardiac surgical patient transfer: operating room to intensive care unit. Journal for Healthcare Quality. 2015; 37(1):22–32 [PubMed: 26042374]
- 27.
- Donnelly MJ, Clauser JM, Tractenberg RE. A multicenter intervention to improve ambulatory care handoffs at the end of residency. Journal of Graduate Medical Education. 2014; 6(1):112–116 [PMC free article: PMC3963766] [PubMed: 24701320]
- 28.
- Donnelly MJ, Clauser JM, Weissman NJ. An intervention to improve ambulatory care handoffs at the end of residency. Journal of Graduate Medical Education. 2012; 4(3):381–384 [PMC free article: PMC3444197] [PubMed: 23997888]
- 29.
- Dowding D. Examining the effects that manipulating information given in the change of shift report has on nurses’ care planning ability. Journal of Advanced Nursing. 2001; 33(6):836–846 [PubMed: 11298222]
- 30.
- Downey LV, Zun L, Burke T. What constitutes a good hand offs in the emergency department: a patient’s perspective. International Journal of Health Care Quality Assurance. 2013; 26(8):760–767 [PubMed: 24422264]
- 31.
- Drach-Zahavy A, Hadid N. Nursing handovers as resilient points of care: linking handover strategies to treatment errors in the patient care in the following shift. Journal of Advanced Nursing. 2015; 71(5):1135–1145 [PubMed: 25641374]
- 32.
- Dubosh NM, Carney D, Fisher J, Tibbles CD. Implementation of an emergency department sign-out checklist improves transfer of information at shift change. Journal of Emergency Medicine. 2014; 47(5):580–585 [PubMed: 25130675]
- 33.
- Dufault M, Duquette CE, Ehmann J, Hehl R, Lavin M, Martin V et al. Translating an evidence-based protocol for nurse-to-nurse shift handoffs. Worldviews on Evidence-Based Nursing. 2010; 7(2):59–75 [PubMed: 20345512]
- 34.
- Emlet LL, Al-Khafaji A, Kim YH, Venkataraman R, Rogers PL, Angus DC. Trial of shift scheduling with standardized sign-out to improve continuity of care in intensive care units. Critical Care Medicine. 2012; 40(12):3129–3134 [PubMed: 23034459]
- 35.
- Evans AS, Yee MS, Hogue CW. Often overlooked problems with handoffs: from the intensive care unit to the operating room. Anesthesia and Analgesia. 2014; 118(3):687–689 [PMC free article: PMC5508102] [PubMed: 24413554]
- 36.
- Field TS, Tjia J, Mazor KM, Donovan JL, Kanaan AO, Harrold LR et al. Randomized trial of a warfarin communication protocol for nursing homes: an SBAR-based approach. American Journal of Medicine. 2011; 124(2):179–7 [PMC free article: PMC10362478] [PubMed: 21295198]
- 37.
- Flanagan ME, Patterson ES, Frankel RM, Doebbeling BN. Evaluation of a physician informatics tool to improve patient handoffs. Journal of the American Medical Informatics Association. 2009; 16(4):509–515 [PMC free article: PMC2705254] [PubMed: 19390111]
- 38.
- Flemming D, Hubner U. How to improve change of shift handovers and collaborative grounding and what role does the electronic patient record system play? Results of a systematic literature review. International Journal of Medical Informatics. 2013; 82(7):580–592 [PubMed: 23628146]
- 39.
- Foster S, Manser T. The effects of patient handoff characteristics on subsequent care: a systematic review and areas for future research. Academic Medicine. 2012; 87(8):1105–1124 [PubMed: 22722354]
- 40.
- Gakhar B, Spencer AL. Using direct observation, formal evaluation, and an interactive curriculum to improve the sign-out practices of internal medicine interns. Academic Medicine. 2010; 85(7):1182–1188 [PubMed: 20375830]
- 41.
- Gardiner TM, Marshall AP, Gillespie BM. Clinical handover of the critically ill postoperative patient: an integrative review. Australian Critical Care. 2015; 28(4):226–234 [PubMed: 25797689]
- 42.
- Gonzalo JD, Yang JJ, Stuckey HL, Fischer CM, Sanchez LD, Herzig SJ. Patient care transitions from the emergency department to the medicine ward: evaluation of a standardized electronic signout tool. International Journal for Quality in Health Care. 2014; 26(4):337–347 [PubMed: 24737836]
- 43.
- Govier M, Medcalf P. Living for the weekend: electronic documentation improves patient handover. Clinical Medicine, Journal of the Royal College of Physicians of London. 2012; 12(2):124–127 [PMC free article: PMC4954095] [PubMed: 22586785]
- 44.
- Graan SM, Botti M, Wood B, Redley B. Nursing handover from ICU to cardiac ward: standardised tools to reduce safety risks. Australian Critical Care. 2016; 29(3):165–171 [PubMed: 26515413]
- 45.
- Graham KL, Marcantonio ER, Huang GC, Yang J, Davis RB, Smith CC. Effect of a systems intervention on the quality and safety of patient handoffs in an internal medicine residency program. Journal of General Internal Medicine. 2013; 28(8):986–993 [PMC free article: PMC3710376] [PubMed: 23595931]
- 46.
- Graham LA. Organization of rehabilitation services. Handbook of Clinical Neurology. 2013; 110:113–120 [PubMed: 23312635]
- 47.
- Halm MA. Nursing handoffs: ensuring safe passage for patients. American Journal of Critical Care. 2013; 22(2):158–162 [PubMed: 23455866]
- 48.
- Health & Social Care Information Centre. Standards for the clinical structure and content of patient records. Health & Social Care Information Centre, 2013. Available from: http://theprsb
.org/publications /bible-sets-out-the-latest-agreed-standards - 49.
- Health Information and Quality Authority. Health technology assessment of the use of information technology for early warning and clinical handover systems. Ireland. Dublin: Health Information and Quality Authority, 2015. Available from: https://www
.hiqa.ie/healthcare /health-technology-assessment /new-assessments /it-early-warning - 50.
- Hesselink G, Schoonhoven L, Barach P, Spijker A, Gademan P, Kalkman C et al. Improving patient handovers from hospital to primary care: a systematic review. Annals of Internal Medicine. 2012; 157(6):417–428 [PubMed: 22986379]
- 51.
- Hill CE, Varma P, Lenrow D, Price RS, Kasner SE. Reducing errors in transition from acute stroke hospitalization to inpatient rehabilitation. Frontiers in Neurology. 2015; 6:227 [PMC free article: PMC4621425] [PubMed: 26579070]
- 52.
- Iedema R, Ball C, Daly B, Young J, Green T, Middleton PM et al. Design and trial of a new ambulance-to-emergency department handover protocol: ‘IMIST-AMBO’. BMJ Quality & Safety. 2012; 21(8):627–633 [PubMed: 22626739]
- 53.
- Jensen SM, Lippert A, Ostergaard D. Handover of patients: a topical review of ambulance crew to emergency department handover. Acta Anaesthesiologica Scandinavica. 2013; 57(8):964–970 [PubMed: 23639134]
- 54.
- Johnson M, Sanchez P, Zheng C. The impact of an integrated nursing handover system on nurses’ satisfaction and work practices. Journal of Clinical Nursing. 2016; 25(1-2):257–268 [PubMed: 26769213]
- 55.
- Kaufmnan J, Twite M, Barrett C, Peyton C, Koehler J, Rannie M et al. A handoff protocol from the cardiovascular operating room to cardiac ICU is associated with improvements in care beyond the immediate postoperative period. Joint Commission Journal on Quality and Patient Safety. 2013; 39(7):306–311 [PubMed: 23888640]
- 56.
- Keebler JR, Lazzara EH, Patzer BS, Palmer EM, Plummer JP, Smith DC et al. Meta-analyses of the effects of standardized handoff protocols on patient, provider, and organizational outcomes. Human Factors. 2016; 58(8):1187–1205 [PubMed: 27821676]
- 57.
- Keenan G, Yakel E, Marriott D. HANDS: a revitalized technology supported care planning method to improve nursing handoffs. Studies in Health Technology and Informatics. 2006; 122:580–584 [PubMed: 17102326]
- 58.
- Kerr D, Klim S, Kelly AM, McCann T. Impact of a modified nursing handover model for improving nursing care and documentation in the emergency department: a pre- and post-implementation study. International Journal of Nursing Practice. 2016; 22(1):89–97 [PubMed: 25354345]
- 59.
- Kessler C, Williams MC, Moustoukas JN, Pappas C. Transitions of care for the geriatric patient in the emergency department. Clinics in Geriatric Medicine. 2013; 29(1):49–69 [PubMed: 23177600]
- 60.
- Kitson AL, Muntlin Athlin A, Elliott J, Cant ML. What’s my line? A narrative review and synthesis of the literature on Registered Nurses’ communication behaviours between shifts. Journal of Advanced Nursing. 2014; 70(6):1228–1242 [PubMed: 24329886]
- 61.
- Kochendorfer KM, Morris LE, Kruse RL, Ge BG, Mehr DR. Attending and resident physician perceptions of an EMR-generated rounding report for adult inpatient services. Family Medicine. 2010; 42(5):343–349 [PubMed: 20461566]
- 62.
- Kuhn EN, Davis MC, Agee BS, Oster RA, Markert JM. Effect of resident handoffs on length of hospital and intensive care unit stay in a neurosurgical population: a cohort study. Journal of Neurosurgery. 2016; 125(1):222–228 [PubMed: 26684784]
- 63.
- Lamond D. The information content of the nurse change of shift report: a comparative study. Journal of Advanced Nursing. 2000; 31(4):794–804 [PubMed: 10759975]
- 64.
- Lee LH, Levine JA, Schultz HJ. Utility of a standardized sign-out card for new medical interns. Journal of General Internal Medicine. 1996; 11(12):753–755 [PubMed: 9016423]
- 65.
- Li P, Ali S, Tang C, Ghali WA, Stelfox HT. Review of computerized physician handoff tools for improving the quality of patient care. Journal of Hospital Medicine. 2013; 8(8):456–463 [PubMed: 23169534]
- 66.
- Malekzadeh J, Mazluom SR, Etezadi T, Tasseri A. A standardized shift handover protocol: improving nurses’ safe practice in intensive care units. Journal of Caring Sciences. 2013; 2(3):177–185 [PMC free article: PMC4134157] [PubMed: 25276725]
- 67.
- Manser T. Fragmentation of patient safety research: a critical reflection of current human factors approaches to patient handover. Journal of Public Health Research. 2013; 2(3):e33 [PMC free article: PMC4147745] [PubMed: 25170504]
- 68.
- Manser T, Foster S. Effective handover communication: an overview of research and improvement efforts. Best Practice and Research Clinical Anaesthesiology. 2011; 25(2):181–191 [PubMed: 21550543]
- 69.
- Mardis T, Mardis M, Davis J, Justice EM, Riley Holdinsky S, Donnelly J et al. Bedside shift-to-shift handoffs: a systematic review of the literature. Journal of Nursing Care Quality. 2016; 31(1):54–60 [PubMed: 26192148]
- 70.
- Mascioli S, Laskowski-Jones L, Urban S, Moran S. Improving handoff communication. Nursing. 2009; 39(2):52–55 [PubMed: 19158646]
- 71.
- Matic J, Davidson PM, Salamonson Y. Review: bringing patient safety to the forefront through structured computerisation during clinical handover. Journal of Clinical Nursing. 2011; 20(1-2):184–189 [PubMed: 20815861]
- 72.
- McQuillan A, Carthey J, Catchpole K, McCulloch P, Ridout DA, Goldman AP. Republished: creating a safe, reliable hospital at night handover: a case study in implementation science. Postgraduate Medical Journal. 2014; 90(1067):493–501 [PubMed: 25140006]
- 73.
- Moller TP, Madsen MD, Fuhrmann L, Ostergaard D. Postoperative handover: characteristics and considerations on improvement: a systematic review. European Journal of Anaesthesiology. 2013; 30(5):229–242 [PubMed: 23492933]
- 74.
- Moseley BD, Smith JH, Diaz-Medina GE, Paz Soldan MM, Wicklund M, Dhamija R et al. Standardized sign-out improves completeness and perceived accuracy of inpatient neurology handoffs. Neurology. 2012; 79(10):1060–1064 [PubMed: 22875095]
- 75.
- Mueller S, Patel R, O’Toole J, Schnipper J. Best practices in inpatient handoffs of care. Hospital Medicine Clinics. 2016; 5(4):518–528
- 76.
- Nakagawa H, Sakuramoto H, Unoki T, Yoshino Y, Yamaguchi S. 923: positive effects of the handoff sheet system on pain management. Critical Care Medicine. 2016; 44(12 Suppl 1):307
- 77.
- Nakhleh RE. Error reduction in surgical pathology. Archives of Pathology and Laboratory Medicine. 2006; 130(5):630–632 [PubMed: 16683877]
- 78.
- National Patients Safety Agency. Safe handover: safe patients. Guidance on clinical handover for clinicians and managers. London. British Medical Association, 2004. Available from: https://www
.bma.org.uk/-/media/Files/ ... /safe%20handover%20safe%20patients.pdf - 79.
- O’Byrne WTI, Weavind L, Selby J. The science and economics of improving clinical communication. Anesthesiology Clinics. 2008; 26(4):729–744 [PubMed: 19041626]
- 80.
- Ong MS, Coiera E. A systematic review of failures in handoff communication during intrahospital transfers. Joint Commission Journal on Quality and Patient Safety. 2011; 37(6):274–284 [PubMed: 21706987]
- 81.
- Organisation for Economic Co-operation and Development (OECD). Purchasing power parities (PPP), 2007. Available from: http://www
.oecd.org/std/ppp - 82.
- Palmer E, Richardson E, Newcombe H, Borg CM. The F.R.I.D.A.Y.S. checklist - preparing our patients for a safe weekend. BMJ Quality Improvement Reports. 2014; 2(2) [PMC free article: PMC4663813] [PubMed: 26734210]
- 83.
- Patel R, Thiagarajan P. Structured approach in improving weekend handovers in a medical high dependency unit. BMJ Quality Improvement Reports. 2014; 3(1) [PMC free article: PMC4645858] [PubMed: 26734283]
- 84.
- Patterson ES. Technology support of the handover: promoting observability, flexibility and efficiency. BMJ Quality & Safety. 2012; 21:(Suppl 1):i19–i21 [PubMed: 23173184]
- 85.
- Patterson ES, Wears RL. Patient handoffs: standardized and reliable measurement tools remain elusive. Joint Commission Journal on Quality and Patient Safety. 2010; 36(2):52–61 [PubMed: 20180437]
- 86.
- Payne CE, Stein JM, Leong T, Dressler DD. Avoiding handover fumbles: a controlled trial of a structured handover tool versus traditional handover methods. BMJ Quality & Safety. 2012; 21(11):925–932 [PubMed: 22706931]
- 87.
- Petrovic MA, Aboumatar H, Baumgartner WA, Ulatowski JA, Moyer J, Chang TY et al. Pilot implementation of a perioperative protocol to guide operating room-to-intensive care unit patient handoffs. Journal of Cardiothoracic and Vascular Anesthesia. 2012; 26(1):11–16 [PubMed: 21889365]
- 88.
- Phillips A. The effect of a standardized form in guiding communication between peers during the hand-off of patients in a hospital setting. Studies in Health Technology and Informatics. 2009; 146:885 [PubMed: 19593034]
- 89.
- Pincavage AT, Dahlstrom M, Prochaska M, Ratner S, Beiting KJ, Oyler J et al. Results of an enhanced clinic handoff and resident education on resident patient ownership and patient safety. Academic Medicine. 2013; 88(6):795–801 [PubMed: 23619066]
- 90.
- Poore SO, Sillah NM, Mahajan AY, Gutowski KA. Patient safety in the operating room: II. Intraoperative and postoperative. Plastic and Reconstructive Surgery. 2012; 130(5):1048–1058 [PubMed: 23096605]
- 91.
- Pothier D, Monteiro P, Mooktiar M, Shaw A. Pilot study to show the loss of important data in nursing handover. British Journal of Nursing. 2005; 14(20):1090–1093 [PubMed: 16301940]
- 92.
- Pucher PH, Johnston MJ, Aggarwal R, Arora S, Darzi A. Effectiveness of interventions to improve patient handover in surgery: a systematic review. Surgery. 2015; 158(1):85–95 [PubMed: 25999255]
- 93.
- Raduma-Tomas MA, Flin R, Yule S, Williams D. Doctors’ handovers in hospitals: a literature review. BMJ Quality & Safety. 2011; 20(2):128–133 [PubMed: 21209133]
- 94.
- Raiten JM, Lane-Fall M, Gutsche JT, Kohl BA, Fabbro M, Sophocles A et al. Transition of care in the cardiothoracic intensive care unit: a review of handoffs in perioperative cardiothoracic and vascular practice. Journal of Cardiothoracic and Vascular Anesthesia. 2015; 29(4):1089–1095 [PubMed: 25910986]
- 95.
- Raptis DA, Fernandes C, Chua W, Boulos PB. Electronic software significantly improves quality of handover in a London teaching hospital. Health Informatics Journal. 2009; 15(3):191–198 [PubMed: 19713394]
- 96.
- Reid C, Moorthy C, Forshaw K. Referral patterns: an audit into referral practice among doctors in emergency medicine. Emergency Medicine Journal. 2005; 22(5):355–358 [PMC free article: PMC1726757] [PubMed: 15843705]
- 97.
- Riesenberg LA, Leitzsch J, Cunningham JM. Nursing handoffs: a systematic review of the literature. American Journal of Nursing. 2010; 110(4):24–26 [PubMed: 20335686]
- 98.
- Riesenberg LA, Leitzsch J, Little BW. Systematic review of handoff mnemonics literature. American Journal of Medical Quality. 2009; 24(3):196–204 [PubMed: 19269930]
- 99.
- Riesenberg LA, Leitzsch J, Massucci JL, Jaeger J, Rosenfeld JC, Patow C et al. Residents’ and attending physicians’ handoffs: a systematic review of the literature. Academic Medicine. 2009; 84(12):1775–1787 [PubMed: 19940588]
- 100.
- Robertson ER, Morgan L, Bird S, Catchpole K, McCulloch P. Interventions employed to improve intrahospital handover: a systematic review. BMJ Quality & Safety. 2014; 23(7):600–607 [PubMed: 24811239]
- 101.
- Royal College of Nursing. The principles of nursing practice. RCN Publishing; 2012
- 102.
- Royal College of Physicians. Acute care toolkit 1: handover. London: 2015. Available from: https://www
.rcplondon .ac.uk/guidelines-policy /acute-care-toolkit-1-handover - 103.
- Ryan S, O’Riordan JM, Tierney S, Conlon KC, Ridgway PF. Impact of a new electronic handover system in surgery. International Journal of Surgery. 2011; 9(3):217–220 [PubMed: 21129508]
- 104.
- Salzwedel C, Bartz HJ, Kuhnelt I, Appel D, Haupt O, Maisch S et al. The effect of a checklist on the quality of post-anaesthesia patient handover: a randomized controlled trial. International Journal for Quality in Health Care. 2013; 25(2):176–181 [PubMed: 23360810]
- 105.
- Segall N, Bonifacio AS, Barbeito A, Schroeder RA, Perfect SR, Wright MC et al. Operating room-to-ICU patient handovers: a multidisciplinary human-centered design approach. Joint Commission Journal on Quality and Patient Safety. 2016; 42(9):400–414 [PMC free article: PMC6152817] [PubMed: 27535457]
- 106.
- Segall N, Bonifacio AS, Schroeder RA, Barbeito A, Rogers D, Thornlow DK et al. Can we make postoperative patient handovers safer? A systematic review of the literature. Anesthesia and Analgesia. 2012; 115(1):102–115 [PMC free article: PMC6152818] [PubMed: 22543067]
- 107.
- Siefferman JW, Lin E, Fine JS. Patient safety at handoff in rehabilitation medicine. Physical Medicine and Rehabilitation Clinics of North America. 2012; 23(2):241–257 [PubMed: 22537691]
- 108.
- Singer JI, Dean J. Emergency physician intershift handovers: an analysis of our transitional care. Pediatric Emergency Care. 2006; 22(10):751–754 [PubMed: 17047478]
- 109.
- Staggers N, Blaz JW. Research on nursing handoffs for medical and surgical settings: an integrative review. Journal of Advanced Nursing. 2013; 69(2):247–262 [PubMed: 22764743]
- 110.
- Starmer AJ, Spector ND, Srivastava R, West DC, Rosenbluth G, Allen AD et al. Changes in medical errors after implementation of a handoff program. New England Journal of Medicine. 2014; 371(19):1803–1812 [PubMed: 25372088]
- 111.
- Stephens RS, Whitman GJR. Postoperative critical care of the adult cardiac surgical patient. Part I: routine postoperative care. Critical Care Medicine. 2015; 43(7):1477–1497 [PubMed: 25962078]
- 112.
- Talbot R, Bleetman A. Retention of information by emergency department staff at ambulance handover: do standardised approaches work? Emergency Medicine Journal. 2007; 24(8):539–542 [PMC free article: PMC2660073] [PubMed: 17652672]
- 113.
- Thompson JE, Collett LW, Langbart MJ, Purcell NJ, Boyd SM, Yuminaga Y et al. Using the ISBAR handover tool in junior medical officer handover: a study in an Australian tertiary hospital. Postgraduate Medical Journal. 2011; 87(1027):340–344 [PubMed: 21310805]
- 114.
- Till A, Sall H, Wilkinson J. Safe handover: safe patients - the electronic handover system. BMJ Quality Improvement Reports. 2014; 2(2) [PMC free article: PMC4663839] [PubMed: 26734244]
- 115.
- Timko C, Below M, Schultz NR, Brief D, Cucciare MA. Patient and program factors that bridge the detoxification-treatment gap: a structured evidence review. Journal of Substance Abuse Treatment. 2015; 52:31–39 [PubMed: 25530425]
- 116.
- Tucker A, Brandling J, Fox P. Improved record-keeping with reading handovers. Nursing Management. 2009; 16(8):30–34 [PubMed: 20050483]
- 117.
- Usher MG, Fanning C, Wu D, Muglia C, Balonze K, Kim D et al. Information handoff and outcomes of critically ill patients transferred between hospitals. Journal of Critical Care. 2016; 36:240–245 [PMC free article: PMC5096986] [PubMed: 27591388]
- 118.
- Van Eaton EG, Horvath KD, Lober WB, Rossini AJ, Pellegrini CA. A randomized, controlled trial evaluating the impact of a computerized rounding and sign-out system on continuity of care and resident work hours. Journal of the American College of Surgeons. 2005; 200(4):538–545 [PubMed: 15804467]
- 119.
- Van Eaton EG, McDonough K, Lober WB, Johnson EA, Pellegrini CA, Horvath KD. Safety of using a computerized rounding and sign-out system to reduce resident duty hours. Academic Medicine. 2010; 85(7):1189–1195 [PubMed: 20592514]
- 120.
- van Sluisveld N, Hesselink G, van der Hoeven JG, Westert G, Wollersheim H, Zegers M. Improving clinical handover between intensive care unit and general ward professionals at intensive care unit discharge. Intensive Care Medicine. 2015; 41(4):589–604 [PMC free article: PMC4392116] [PubMed: 25672275]
- 121.
- Vines MM, Dupler AE, Van Son CR, Guido GW. Improving client and nurse satisfaction through the utilization of bedside report. Journal for Nurses in Professional Development. 2014; 30(4):166–2 [PubMed: 25036080]
- 122.
- Walton H, Munro W. Improving the quality of handover by addressing handover culture and introducing a new, multi-disciplinary, team-based handover meeting. BMJ Quality Improvement Reports. 2015; 4(1) [PMC free article: PMC4693072] [PubMed: 26734418]
- 123.
- Williamson A, Bradley A, Khan K. Using a simple handover to improve the timing of gentamicin levels. BMJ Quality Improvement Reports. 2015; 4(1) [PMC free article: PMC4693051] [PubMed: 26734400]
- 124.
- Wood K, Crouch R, Rowland E, Pope C. Clinical handovers between prehospital and hospital staff: literature review. Emergency Medicine Journal. 2015; 32(7):577–581 [PubMed: 25178977]
- 125.
- World Health Organisation. Communication during patient hand-overs. Switzerland. WHO Press, 2007. Available from: http://www
.who.int/patientsafety /solutions /patientsafety/PS-Solution3.pdf - 126.
- Yao GL, Novielli N, Manaseki-Holland S, Chen Y-F, van der Klink M, Barach P et al. Evaluation of a predevelopment service delivery intervention: an application to improve clinical handovers. BMJ Quality & Safety. 2012; 21:i29–i38 [PMC free article: PMC3551195] [PubMed: 22976505]
- 127.
- Zou XJ, Zhang YP. Rates of nursing errors and handoffs-related errors in a medical unit following implementation of a standardized nursing handoff form. Journal of Nursing Care Quality. 2016; 31(1):61–67 [PubMed: 26035707]
Appendices
Appendix A. Review protocol
Table 8Review protocol: Do structured patient handovers between healthcare professionals improve outcomes?
| Review question | Structured patient handovers |
|---|---|
| Guideline condition and its definition | Acute medical emergencies. |
| Objectives | To see if structured means are better than unstructured for relaying patient information and to assess the best method for conducting handover for example, verbal, paper-based or electronic. |
| Review population | Adults and young people (16 years and over) with a suspected or confirmed AME (in all contexts not just secondary care). |
| Adults. | |
| Line of therapy not an inclusion criterion. | |
|
Interventions and comparators: generic/class; specific/drug (All interventions will be compared with each other, unless otherwise stated) |
Structured (planned framework as defined by the study) between healthcare professionals between shifts in acute settings; this will include (i) set times of the day, (ii) using a structured template or proforma for the handover (iii) recording the information in written or electronic form. Paper-based handover; using paper to conduct the structured handover. Verbal patient handover; verbally conducting the structured handover. Electronic-based handover; using electronic means to conduct the structured handover. Normal handover; routine unstructured handover. |
| Outcomes |
|
| Study design | Systematic reviews (SRs) of RCTs, RCTs, observational studies only to be included if no relevant SRs or RCTs are identified. |
| Unit of randomisation |
Patient Setting |
| Crossover study | Permitted |
| Minimum duration of study | Not defined |
| Other exclusions |
Major trauma Structured reporting around major incidents (not applicable to individual) standardised criteria for admission and discharge covered by other questions. |
| Sensitivity/other analysis | If studies have pre-specified in their protocols that results for any of these subgroup populations will be analysed separately, then they will be included in the subgroup analysis. |
| Subgroup analyses if there is heterogeneity |
|
| Search criteria |
Databases: Medline, Embase, the Cochrane Library Date limits for search: 2005 Language: English |
Appendix B. Clinical article selection
Appendix C. Forest plots
C.1. Intensive Care Unit
C.3. Emergency Department
Appendix D. Clinical evidence tables
Download PDF (443K)
Appendix E. Economic evidence tables
Download PDF (420K)
Appendix F. GRADE tables
Table 9Clinical evidence profile: Intensive care unit
| Quality assessment | No of patients | Effect | Quality | Importance | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| No of studies | Design | Risk of bias | Inconsistency | Indirectness | Imprecision | Other considerations | Structured | Unstructured | Relative (95% CI) | Absolute | ||
| Mortality | ||||||||||||
| 1 | observational studies | serious1 | no serious inconsistency | no serious indirectness | very serious2 | none |
26/389 (6.7%) | 8.5% | RR 0.71 (0.43 to 1.17) | 26 fewer per 1000 (from 48 fewer to 14 more) |
⨁◯◯◯ VERY LOW | CRITICAL |
| Re-admission <48hours | ||||||||||||
| 1 | observational studies | serious1 | no serious inconsistency | no serious indirectness | very serious2 | none |
21/431 (4.9%) | 3.6% | RR 1.35 (0.7 to 2.63) | 13 more per 1000 (from 11 fewer to 59 more) |
⨁◯◯◯ VERY LOW | CRITICAL |
| Length of Stay (Better indicated by lower values) | ||||||||||||
| 1 | observational studies | serious1 | no serious inconsistency | no serious indirectness | no serious imprecision | none | 431 | 389 | - | MD 2.78 lower (4.68 to 0.88 lower) |
⨁◯◯◯ VERY LOW | IMPORTANT |
| Staff satisfaction | ||||||||||||
| 1 | observational studies | serious1 | no serious inconsistency | no serious indirectness | no serious imprecision | none |
34/57 (59.6%) | 18.2% | RR 3.09 (1.7 to 5.61) | 380 more per 1000 (from 127 more to 839 more) |
⨁◯◯◯ VERY LOW | IMPORTANT |
| Staff satisfaction - Attending Physician | ||||||||||||
| 1 | observational studies | serious1 | no serious inconsistency | no serious indirectness | serious2 | none |
6/11 (54.5%) | 18.2% | RR 3 (0.77 to 11.74) | 364 more per 1000 (from 42 fewer to 1000 more) |
⨁◯◯◯ VERY LOW | IMPORTANT |
| Staff satisfaction – Fellows | ||||||||||||
| 1 | observational studies | serious1 | no serious inconsistency | no serious indirectness | very serious2 | none |
6/16 (37.5%) | 43.8% | RR 0.86 (0.37 to 1.99) | 61 fewer per 1000 (from 276 fewer to 434 more) |
⨁◯◯◯ VERY LOW | IMPORTANT |
| Staff satisfaction – Nurses | ||||||||||||
| 1 | observational studies | serious1 | no serious inconsistency | no serious indirectness | no serious imprecision | none |
22/30 (73.3%) | 6.7% | RR 11 (2.83 to 42.7) | 670 more per 1000 (from 123 more to 1000 more) |
⨁◯◯◯ VERY LOW | IMPORTANT |
- 1
All non-randomised studies automatically downgraded due to selection bias. Studies may be further downgraded by 1 increment if other factors suggest additional high risk of bias, or 2 increments if other factors suggest additional very high risk of bias.
- 2
Downgraded by 1 increment if the confidence interval crossed 1 MID or by 2 increments if the confidence interval crossed both MIDs.
Table 10Clinical evidence profile: Neurology Unit
| Quality assessment | No of patients | Effect | Quality | Importance | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| No of studies | Design | Risk of bias | Inconsistency | Indirectness | Imprecision | Other considerations | Structured | Unstructured | Relative (95% CI) | Absolute | ||
| ICU Readmission | ||||||||||||
| 1 | observational studies | serious1 | no serious inconsistency | no serious indirectness | very serious2 | none |
5/131 (3.8%) | 3.1% | RR 1.24 (0.34 to 4.52) | 7 more per 1000 (from 20 fewer to 109 more) |
⨁◯◯◯ VERY LOW | CRITICAL |
| Rapid Response Team Call at 6 Months | ||||||||||||
| 1 | observational studies | serious1 | no serious inconsistency | no serious indirectness | very serious2 | none |
4/131 (3.1%) | 1.5% | RR 1.98 (0.37 to 10.65) | 15 more per 1000 (from 9 fewer to 145 more) |
⨁◯◯◯ VERY LOW | CRITICAL |
- 1
All non-randomised studies automatically downgraded due to selection bias. Studies may be further downgraded by 1 increment if other factors suggest additional high risk of bias, or 2 increments if other factors suggest additional very high risk of bias.
- 2
Downgraded by 1 increment if the confidence interval crossed 1 MID or by 2 increments if the confidence interval crossed both MIDs.
Table 11Clinical evidence profile: Emergency Department
| Quality assessment | No of patients | Effect | Quality | Importance | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| No of studies | Design | Risk of bias | Inconsistency | Indirectness | Imprecision | Other considerations | Electronic | Routine | Relative (95% CI) | Absolute | ||
| Staff satisfaction (Better indicated by higher values) | ||||||||||||
| 1 | observational studies | serious1 | no serious inconsistency | no serious indirectness | no serious imprecision | none | 1058 | 78 | - | MD 0.17 higher (0.33 lower to 0.67 higher) |
⨁◯◯◯ VERY LOW | IMPORTANT |
| Avoidable adverse events (medications administered as prescribed) | ||||||||||||
| 1 | observational studies | serious1 | no serious inconsistency | no serious indirectness | no serious imprecision | none |
149/151 (98.7%) | 97.7% | RR 1.01 (0.98 to 1.04) | 10 more per 1000 (from 20 fewer to 39 more) |
⨁◯◯◯ VERY LOW | CRITICAL |
- 1
All non-randomised studies automatically downgraded due to selection bias. Studies may be further downgraded by 1 increment if other factors suggest additional high risk of bias, or 2 increments if other factors suggest additional very high risk of bias
Table 12Clinical evidence profile: Internal Medicine
| Quality assessment | No of patients | Effect | Quality | Importance | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| No of studies | Design | Risk of bias | Inconsistency | Indirectness | Imprecision | Other considerations | Electronic | Routine | Relative (95% CI) | Absolute | ||
| Critical data omissions | ||||||||||||
| 1 | observational studies | serious1 | no serious inconsistency | no serious indirectness | no serious imprecision | none | 0/19 (0%) | 79.3% | Peto OR 0.04 (0.01 to 0.14) | 660 fewer per 1000 (from 444 fewer to 756 fewer) |
⨁◯◯◯ VERY LOW | CRITICAL |
| Near Misses | ||||||||||||
| 1 | observational studies | serious1 | no serious inconsistency | no serious indirectness | no serious imprecision | none |
0/19 (0%) | 23.1% | Peto OR 0.18 (0.04 to 0.8) | 180 fewer per 1000 (from 37 fewer to 219 fewer) |
⨁◯◯◯ VERY LOW | CRITICAL |
| Adverse events | ||||||||||||
| 1 | observational studies | serious1 | no serious inconsistency | no serious indirectness | very serious2 | none |
0/19 (0%) | 10.3% | Peto OR 0.21 (0.02 to 1.78) | 79 fewer per 1000 (from 101 fewer to 67 more) |
⨁◯◯◯ VERY LOW | CRITICAL |
| Avoidable adverse events (handoffs related errors) | ||||||||||||
| 1 | observational studies | serious1 | no serious inconsistency | no serious indirectness | no serious imprecision | none |
5/1970 (0.25%) | 2.70% | RR 0.09 (0.04 to 0.23) | 25 fewer per 1000 (from 21 fewer to 26 fewer) |
⨁◯◯◯ VERY LOW | CRITICAL |
- 1
All non-randomised studies automatically downgraded due to selection bias. Studies may be further downgraded by 1 increment if other factors suggest additional high risk of bias, or 2 increments if other factors suggest additional very high risk of bias.
- 2
Downgraded by 1 increment if the confidence interval crossed 1 MID or by 2 increments if the confidence interval crossed both MIDs.
Appendix G. Excluded clinical studies
Table 13Studies excluded from the clinical review
| Reference | Reason for exclusion |
|---|---|
| Abraham 20122 | Incorrect comparison (paper based versus paper based handover tools) |
| Abraham 20144 | No useable outcomes |
| Abraham 20143 | Systematic review (incorrect PICO) |
| Ah-kye 20155 | Incorrect population (trauma patients) |
| Ahmed 20126 | Incorrect population and study design (before and after study; acute surgical admissions) |
| Anderson 20157 | Systematic review (incorrect PICO) |
| Anon 201549 | Systematic review (incorrect PICO) |
| AORN 20161 | Evidence appraisal of a RCT Salzwedel 2013- the study has been excluded due to incorrect population (post-anaesthesia patients) |
| Arora 20098 | Systematic review (incorrect PICO) |
| Barnes 20119 | No relevant outcomes |
| Berkenstadt 200810 | No relevant outcomes |
| Blaz 201211 | Systematic review (no references included) |
| Bost 201012 | Incorrect study design (qualitative) |
| Brown 201513 | No relevant outcomes |
| Bump 201214 | Incorrect comparison (does not compare handover types (standard sign out versus additional training.) |
| Christie 200916 | Narrative review |
| Chu 200917 | Incorrect study design (survey) |
| Cohen 201018 | Systematic review (no relevant outcomes) |
| Collins 201119 | Systematic review (incorrect PICO) |
| Cornell 201421 | No relevant outcomes |
| Craig 201222 | No relevant outcomes |
| Curtis 201323 | No relevant outcomes |
| Dawson 201324 | Systematic review (incorrect PICO) |
| Dhillon 201125 | Incorrect population (surgical patients) |
| Dixon 2015A26 | Incorrect population (surgical patients) |
| Donnelly 201228 | Incorrect population (not AME); no relevant outcomes |
| Donnelly 201427 | Incorrect population (not AME) |
| Dowding 200129 | No useable outcomes |
| Downey 201330 | Incorrect population (trauma patients) |
| DRACHZAHAVY 201531 | No useable outcomes |
| DuBosh 201432 | No useable outcomes |
| Dufault 201033 | Systematic review (incorrect PICO) |
| Evans 201435 | Incorrect study design (narrative review) |
| Field 201136 | Incorrect setting (nursing homes) |
| Flanagan 200937 | Incorrect study design (survey) |
| Flemming 201338 | Systematic review (incorrect PICO) |
| Foster 201239 | Systematic review (incorrect PICO) |
| Gakhar 201040 | No relevant outcomes |
| Gardiner 201541 | Systematic review (incorrect PICO) |
| Govier2012A43 | Incorrect study design (audit) |
| GRAAN 201644 | No useable outcomes. |
| Halm 201347 | Systematic review (incorrect PICO) |
| Hesselink 201250 | Incorrect population (patient discharge from hospital to primary care) |
| Hill 201551 | Incorrect intervention (inter-hospital transfer) |
| Iedema 201252 | Incorrect study design (survey) |
| Jensen 201353 | Systematic review (incorrect PICO) |
| Johnson 201654 | Comparator not defined |
| Kaufmnan 201355 | Incorrect population (mainly children and neonates) |
| Keebler 201656 | Systematic review (references screened) |
| Keenan 200657 | Description of handover tool only. |
| Kessler 201359 | Incorrect study design (narrative review) |
| Kitson 201460 | Incorrect study design (narrative review) |
| Kochendorfer 201061 | Incorrect intervention (electronic rounding report) |
| KUHN 201662 | Surgical patients – patients admitted to neurosurgical service |
| Lamond 200063 | Looking at the information content of handover, not comparing types of handover. |
| Lee 199664 | Pre-1995 study |
| Li 201365 | Systematic review (incorrect PICO) |
| Malekzadeh 201366 | No useable outcomes |
| Manser 201168 | Incorrect study design (narrative review) |
| Manser 201367 | Incorrect study design (narrative review) |
| Mardis 201669 | Systematic review (references screened) |
| Matic 201171 | Incorrect study design (narrative review) |
| Moller 201373 | Incorrect population (surgical patients) |
| Moseley 201274 | Incorrect population (neurology inpatients) |
| MCQUILLAN 201472 | Incorrect population- Paediatric patients |
| Mueller 201675 | Incorrect population (paediatric patients) |
| Nakagawa 201676 | Study abstract |
| Nakhleh 200677 | Incorrect population (surgical patients) |
| O’Byrne 200879 | Incorrect study design (narrative review) |
| Ong 201180 | Systematic review (incorrect PICO) |
| Palmer 201482 | Incorrect intervention (checklist to encourage the completion of outstanding tasks before shift change on Friday evening) |
| Patel 201483 | Comparator not defined |
| Patterson 201085 | Incorrect study design (narrative review) |
| Patterson 201284 | Incorrect study design (narrative review) |
| Payne 201286 | Incorrect study design (before and after study); no useable outcomes |
| Petrovic 201287 | Comparator not defined |
| Phillips 200988 | Incorrect study design (observations and interviews). No comparison group stated. |
| Pincavage 201389 | Incorrect population (primary care setting) |
| Poore 201290 | Incorrect population (surgical patients) |
| Pothier 200591 | No relevant outcomes |
| Pucher 201592 | Incorrect population (surgical patients) |
| Raduma-Tomas 201193 | Systematic review (incorrect PICO) |
| RAITEN 201594 | Review -scanned for relevant references |
| Raptis 200995 | No useable outcomes |
| Reid 200596 | Incorrect study design (audit) |
| Riesenberg 200999 | Systematic review (incorrect PICO) |
| Riesenberg 200998 | Systematic review (incorrect PICO) |
| Riesenberg 201097 | Systematic review (incorrect PICO) |
| Robertson 2014100 | Systematic review (incorrect PICO) |
| Ryan 2011103 | No extractable outcomes (length of stay reported as median and interquartile range) |
| Salzwedel 2013104 | Incorrect population (post-anaesthesia patients) |
| Starmer 2014110 | Incorrect population (paediatrics) |
| Segall 2012106 | Incorrect population (surgical patients) |
| SEGALL 2016105 | Inappropriate study design- surveys, interviews and focus groups |
| Siefferman 2012107 | Incorrect population (rehab patients) |
| Singer 2006108 | Incorrect study design (narrative review) |
| Staggers 2013109 | Systematic review (incorrect PICO) |
| Stephens 2015111 | Incorrect population (surgical patients) |
| Talbot 2007112 | No useable outcomes |
| Thompson 2011113 | No useable outcomes |
| Timko 2015115 | Incorrect population (substance misuse) |
| Till 2014114 | No relevant outcomes |
| USHER 2016117 | Inappropriate intervention- transfer between hospitals (inter-hospital hand-offs) |
| Van Eaton 2005118 | No relevant outcomes |
| Van Eaton 2010119 | Incorrect population (more than 50% surgical patients, trauma and paediatrics) |
| Van Sluisveld 2015120 | Systematic review (incorrect PICO) |
| Vines 2014121 | Systematic review (incorrect PICO) |
| Walton 2015122 | No relevant outcomes |
| Williamson 2015123 | Incorrect population (surgical patients); comparator not defined |
| Wood 2015124 | Systematic review (incorrect PICO) |
Appendix H. Excluded economic studies
No economic studies were excluded.
Footnotes
- a
NICE’s guideline on medicines optimisation includes recommendations on medicines-related communication systems when patients move from one care setting to another, medicines reconciliation, clinical decision support, and medicines-related models of organisational and cross-sector working.
- Structured patient handovers - Emergency and acute medical care in over 16s: ser...Structured patient handovers - Emergency and acute medical care in over 16s: service delivery and organisation
Your browsing activity is empty.
Activity recording is turned off.
See more...