NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
LiverTox: Clinical and Research Information on Drug-Induced Liver Injury [Internet]. Bethesda (MD): National Institute of Diabetes and Digestive and Kidney Diseases; 2012-.

LiverTox: Clinical and Research Information on Drug-Induced Liver Injury [Internet].
Show detailsOVERVIEW
Introduction
Amiloride is a potassium-sparing diuretic used in the therapy of edema often in combination with thiazide diuretics. Amiloride has been linked to rare cases of clinically apparent drug induced liver disease.
Background
Amiloride (a mil' oh ride) is a pyrazinoylguanidine derivative that acts on the sodium channels of renal epithelial cells causing an increase in sodium excretion with little or no effect on potassium excretion, thus accounting for its potassium-sparing characteristics. Amiloride is similar in action to triamterene, but differs in chemical structure. Amiloride was approved for use in the United States in 1986, but is not widely used. Amiloride is available in 5 mg tablets in generic forms and under the brand name of Midamor. The typical dose of amiloride is 5 to 20 mg in one or two doses daily. Amiloride causes only a modest diuresis and it is often used in combination with a thiazide diuretic (such as hydrochlorothiazide: Moduretic), which takes advantage of it potassium-sparing characteristics to offset the potassium-wasting characteristics of the thiazides. The major side effects of amiloride include hyperkalemia, headache, dizziness, gastrointestinal upset and rash.
Hepatotoxicity
Amiloride therapy has not been associated with serum aminotransferase elevations. Idiosyncratic, clinically apparent liver injury from amiloride is rare, but several instances have been reported as isolated case reports in which the combination of amiloride with hydrochlorothiazide was used (Case 1). The numbers of cases have been too few to characterize the clinical features, but the latency to onset was ranged from 2 to 12 months and the pattern of injury either hepatocellular or mixed. Immunoallergic features and autoantibodies have not been associated with the liver injury from amiloride.
Likelihood score: D (possible rare cause of liver injury).
Mechanism of Injury
The mechanism of amiloride hepatic injury is unknown, but is likely due to metabolic idiosyncrasy.
Outcome and Management
The rare instances of clinically apparent liver injury due to amiloride/hydrochlorothiazide combinations have been associated with jaundice and at least one case resulted in cirrhosis and ultimately death from liver disease. There is unlikely to be cross reactivity to the liver injury with other potassium-sparing diuretics, which have quite different chemical structures.
Drug Class: Diuretics, Potassium-Sparing Diuretics
Other Drugs in the Subclass: Eplerenone, Spironolactone, Triamterene
CASE REPORT
Case 1. Amiloride/hydrochlorothiazide induced acute liver injury.(1)
A 37 year old man with hypertension developed jaundice and hepatitis 2 months after starting the combination of amiloride (2.5 mg) and hydrochlorothiazide (25 mg). On examination, he was jaundiced and had mild fever (37.6o C), but no rash or organomegaly. Laboratory testing showed serum bilirubin of 5.8 mg/dL with marked elevations in serum aminotransferase levels (Table). White blood cell counts, eosinophil counts, prothrombin time, and serum albumin were normal. Tests for hepatitis B and for autoantibodies were negative. Magnetic resonance imaging of the liver and biliary system were normal. The diuretics were stopped, but liver tests worsened for the next three weeks, serum bilirubin rising to as high as 28.3 mg/dL. A liver biopsy showed an intrahepatic cholestasis typical of drug induced hepatic injury with some degree of bile duct injury. Prednisolone (60 mg daily) was initiated, and he improved slowly. Four months later and 6 weeks after stopping prednisolone therapy, he was asymptomatic, but serum enzyme levels were still mildly elevated. A note in follow up mentioned that he developed pancytopenia and was retreated with corticosteroids, but that serum bilirubin and aminotransferase levels were normal.
Key Points
| Medication: | Amiloride (2.5 mg) and hydrochlorothiazide (25 mg daily) |
|---|---|
| Pattern: | Hepatocellular (R=32.5) |
| Severity: | 3+ (jaundice, hospitalization) |
| Latency: | 2 months |
| Recovery: | Incomplete at 4 months |
| Other medications: | None |
Laboratory Values
| Time After Starting | Time After Stopping | ALT U/L) | Alk P (U/L) | Bilirubin* (mg/dL) | Comments |
|---|---|---|---|---|---|
| 8 weeks | 0 | 2930 | 494 | 11.1 | Diuretics stopped |
| 9 weeks | 1 week | 1466 | 351 | 18.5 | Liver biopsy |
| 11 weeks | 3 weeks | 697 | 309 | 28.3 | Prednisolone started |
| 5 months | 3 months | 29 | 176 | 1.5 | Prednisolone stopped |
| 6 months | 4 months | 196 | 225 | 1.5 | |
| Normal Values | <50 | <275 | <1.2 | ||
- *
Converted from µmol/L to mg/dL.
Comment
This patient developed an acute hepatitis-like illness followed by deep jaundice 2 months after starting a combination of amiloride and a thiazide diuretic for hypertension. A liver biopsy suggested bile duct paucity and the course was typical with prolonged jaundice and persistent alkaline phosphatase elevations in follow up. The course was complicated by the development of pancytopenia during recovery. It is not clear whether the amiloride or the hydrochlorothiazide was responsible for the hepatic injury (and the bone marrow failure). Certainly, other cases of thiazide diuretic induced liver injury have been quite different with a shorter latency and more benign course. No other similar cases of liver injury implicating amiloride have been reported.
PRODUCT INFORMATION
REPRESENTATIVE TRADE NAMES
Amiloride – Generic, Midamor®
DRUG CLASS
Diuretics
Product labeling at DailyMed, National Library of Medicine, NIH
CHEMICAL FORMULA AND STRUCTURE
| DRUG | CAS REGISTRY NUMBER | MOLECULAR FORMULA | STRUCTURE |
|---|---|---|---|
| Amiloride | 2609-46-3 | C6-H8-Cl-N7-O |
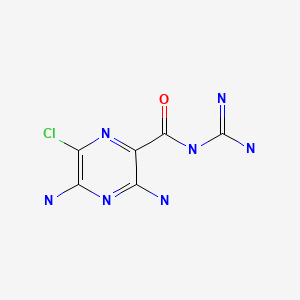
|
CITED REFERENCES
- 1.
- Valhovd M, Kildahl-Andersen O. Tidsskr Nor Laegeforen. 2003;123:1202–3. [Drug-induced severe jaundice] Norwegian. [PubMed: 12789790]
ANNOTATED BIBLIOGRAPHY
References updated: 13 October 2021
- Zimmerman HJ. Diuretic drugs. Drugs used in cardiovascular disease. In, Zimmerman HJ. Hepatotoxicity: the adverse effects of drugs and other chemicals on the liver. 2nd ed. Philadelphia: Lippincott, 1999, pp. 662-4.(Expert review of hepatotoxicity of diuretics published in 1999 mentions that clinically apparent liver injury due to diuretics is rare; hepatocellular jaundice has been reported with triamterene; no mention of amiloride).
- De Marzio DH, Navarro VJ. Hepatotoxicity of cardiovascular and antidiabetic drugs. In, Kaplowitz N, DeLeve LD, eds. Drug-induced liver disease. 3rd ed. Amsterdam: Elsevier, 2013, pp. 519-40.(Review of hepatotoxicity of cardiovascular agents, mentions that thiazide diuretics can rarely cause cholestatic hepatitis; no mention of potassium sparing diuretics).
- Jackson EK. Drugs affecting renal excretory function. In, Brunton LL, Hilal-Dandan R, Knollman BC, eds. Goodman & Gilman’s the pharmacological basis of therapeutics. 13th ed. New York: McGraw-Hill, 2018, pp. 445-70.(Textbook of pharmacology and therapeutics).
- Valhovd M, Kildahl-Andersen O. Tidsskr Nor Laegeforen. 2003;123:1202–3. [Drug-induced severe jaundice] Norwegian. [PubMed: 12789790](37 year old man developed jaundice 2 months after starting hydrochlorothiazide and amiloride for hypertension [bilirubin 5.8 rising to 28.3 mg/dL, ALT 2930 U/L, Alk P twice ULN, INR 1.4], with prolonged jaundice leading to 8 week course of prednisone, recovered but then developed pancytopenia: Case 1).
- Russo MW, Galanko JA, Shrestha R, Fried MW, Watkins P. Liver transplantation for acute liver failure from drug-induced liver injury in the United States. Liver Transpl. 2004;10:1018–23. [PubMed: 15390328](Among ~50,000 liver transplants reported to UNOS between 1990 and 2002, 137 [0.5%] were done for idiosyncratic drug induced acute liver failure, none were attributed to a diuretic).
- Björnsson E, Jerlstad P, Bergqvist A, Olsson R. Fulminant drug-induced hepatic failure leading to death or liver transplantation in Sweden. Scand J Gastroenterol. 2005;40:1095–101. [PubMed: 16165719](Survey of all cases of DILI with fatal outcome from Swedish Adverse Drug Reporting system from 1966-2002; 103 cases were identified one of which was associated with hydrochlorothiazide and one with amiloride use, but other more likely agents were being taken in both instances).
- Andrade RJ, Lucena MI, Fernández MC, Pelaez G, Pachkoria K, García-Ruiz E, García-Muñoz B, et al. Drug-induced liver injury: an analysis of 461 incidences submitted to the Spanish Registry over a 10-year period. Gastroenterology. 2005;129:512–21. [PubMed: 16083708](Reports of drug induced liver injury to a Spanish network found 570 cases; diuretics not mentioned as cause).
- Björnsson E, Olsson R. Suspected drug-induced liver fatalities reported to the WHO database. Dig Liver Dis. 2006;38:33–8. [PubMed: 16054882](Survey of drug induced liver fatalities reported to WHO database between 1968-2003 revealed 4690 reports [89% from the US]; no diuretic found in the 20 most commonly implicated agents).
- Sabaté M, Ibáñez L, Pérez E, Vidal X, Buti M, Xiol X, Mas A, et al. Risk of acute liver injury associated with the use of drugs: a multicentre population survey. Aliment Pharmacol Ther. 2007;25:1401–9. [PubMed: 17539979](Population based survey of 126 cases of acute liver injury [24 with acute liver failure] due to drugs between 1993-1999 in Spain calculated relative risk of injury compared to the general population: hydrochlorothiazide was being taken by 7 and furosemide by 8 patients, but relative risk was not increased in comparison to a control group).
- Chalasani N, Fontana RJ, Bonkovsky HL, Watkins PB, Davern T, Serrano J, Yang H, Rochon J., Drug Induced Liver Injury Network (DILIN). Causes, clinical features, and outcomes from a prospective study of drug-induced liver injury in the United States. Gastroenterology. 2008;135:1924–34. [PMC free article: PMC3654244] [PubMed: 18955056](Among 300 cases of drug induced liver disease in the US collected between 2004 and 2008, no case was attributed to a diuretic).
- Drugs for hypertension. Treat Guidel Med Lett. 2009;7:1–10. [PubMed: 19107095](Brief overview of currently available drugs for hypertension with guidelines on their use and information on prices and toxicities: “thiazide diuretics are the first-line therapy for many patients with hypertension”).
- Björnsson E, Davidsdottir L. The long-term follow-up after idiosyncratic drug-induced liver injury with jaundice. J Hepatol. 2009;50:511–7. [PubMed: 19155082](Among 685 patients with drug induced liver injury, 23 [3.4%] were later hospitalized for chronic liver disease and 8 were showed to have cirrhosis, one of whom had acute icteric liver injury 3 years earlier attributed to the combination of amiloride and hydrochlorothiazide).
- Devarbhavi H, Dierkhising R, Kremers WK, Sandeep MS, Karanth D, Adarsh CK. Single-center experience with drug-induced liver injury from India: causes, outcome, prognosis, and predictors of mortality. Am J Gastroenterol. 2010;105:2396–404. [PubMed: 20648003](Among 313 cases of drug induced liver injury seen over a 12 year period at a large hospital in Bangalore, India, none were attributed to a diuretic).
- Ferrajolo C, Capuano A, Verhamme KM, Schuemie M, Rossi F, Stricker BH, Sturkenboom MC. Drug-induced hepatic injury in children: a case/non-case study of suspected adverse drug reactions in VigiBase. Br J Clin Pharmacol. 2010;70:721–8. [PMC free article: PMC2997312] [PubMed: 21039766](Among 624,673 adverse event reports in children between 2000 and 2006 in the WHO VigiBase, no diuretic was mentioned among the 30 most common causes of liver injury).
- Reuben A, Koch DG, Lee WM., Acute Liver Failure Study Group. Drug-induced acute liver failure: results of a U.S. multicenter, prospective study. Hepatology. 2010;52:2065–76. [PMC free article: PMC3992250] [PubMed: 20949552](Among 1198 patients with acute liver failure enrolled in a US prospective study between 1998 and 2007, 133 were attributed to drug induced liver injury, of which none were attributed to a diuretic).
- Björnsson ES, Bergmann OM, Björnsson HK, Kvaran RB, Olafsson S. Incidence, presentation and outcomes in patients with drug-induced liver injury in the general population of Iceland. Gastroenterology. 2013;144:1419–25. [PubMed: 23419359](In a population based study of drug induced liver injury from Iceland, 96 cases were identified over a 2 year period, none of which were attributed to a diuretic).
- Hernández N, Bessone F, Sánchez A, di Pace M, Brahm J, Zapata R, A, Chirino R, et al. Profile of idiosyncratic drug induced liver injury in Latin America: an analysis of published reports. Ann Hepatol. 2014;13:231–9. [PubMed: 24552865](Among 176 reports of drug induced liver injury from Latin America published between 1996 and 2012, none were attributed to a diuretic).
- Chalasani N, Bonkovsky HL, Fontana R, Lee W, Stolz A, Talwalkar J, Reddy KR, et al. United States Drug Induced Liver Injury Network. Features and outcomes of 899 patients with drug-induced liver injury: The DILIN Prospective Study. Gastroenterology. 2015;148:1340–52.e7. [PMC free article: PMC4446235] [PubMed: 25754159](Among 899 cases of drug induced liver injury enrolled in a US prospective study between 2004 and 2013, none were attributed to a diuretic).
- Drugs for hypertension. Med Lett Drugs Ther. 2020;62(1598):73–80. [PubMed: 32555118](Concise summary of efficacy, safety and costs of drug therapy of hypertension including the diuretics, focusing upon relative usefulness; no mention of hepatic adverse events).
- PMCPubMed Central citations
- PubChem SubstanceRelated PubChem Substances
- PubMedLinks to PubMed
- [Action of trichlormethiazide and amiloride on cellular Na+, K+ and Mg+ concentrations].[Schweiz Med Wochenschr. 1989][Action of trichlormethiazide and amiloride on cellular Na+, K+ and Mg+ concentrations].Kisters K, Zidek W, Rahn KH. Schweiz Med Wochenschr. 1989 Dec 16; 119(50):1837-9.
- Plasma electrolytes in elderly patients taking fixed combination diuretics.[Postgrad Med J. 1986]Plasma electrolytes in elderly patients taking fixed combination diuretics.Bayer AJ, Farag R, Browne S, Pathy MS. Postgrad Med J. 1986 Mar; 62(725):159-62.
- New drug evaluations amiloride (Midamor, Merck, Sharp and Dohme).[Drug Intell Clin Pharm. 1981]New drug evaluations amiloride (Midamor, Merck, Sharp and Dohme).Macfie HL, Colvin CL, Anderson PO. Drug Intell Clin Pharm. 1981 Feb; 15(2):94-8.
- Review Magnesium and potassium-sparing diuretics.[Magnesium. 1986]Review Magnesium and potassium-sparing diuretics.Ryan MP. Magnesium. 1986; 5(5-6):282-92.
- Review Treating essential hypertension. The first choice is usually a thiazide diuretic.[Prescrire Int. 2014]Review Treating essential hypertension. The first choice is usually a thiazide diuretic.. Prescrire Int. 2014 Sep; 23(152):215-20.
- Amiloride - LiverToxAmiloride - LiverTox
Your browsing activity is empty.
Activity recording is turned off.
See more...