NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
LiverTox: Clinical and Research Information on Drug-Induced Liver Injury [Internet]. Bethesda (MD): National Institute of Diabetes and Digestive and Kidney Diseases; 2012-.

LiverTox: Clinical and Research Information on Drug-Induced Liver Injury [Internet].
Show detailsOVERVIEW
Introduction
Metronidazole is a nitroimidazole derivative bactericidal agent widely used in the treatment of many anaerobic and certain protozoan and parasitic infections. Metronidazole has been linked to rare instances of acute, clinically apparent liver injury.
Background
Metronidazole (met" roe nid' a zole) is a nitroimidazole antibiotic that is activated by reduction of its nitro group by susceptible organisms. The activated form of metronidazole is a highly reactive radical anion which targets and damages large protein molecules and DNA. Mammalian cells do not ordinarily activate metronidazole, which accounts for its lack of toxicity in humans. Metronidazole was approved for use in the United States in 1963 and currently several million prescriptions are filled yearly. Metronidazole is indicated for treatment and prophylaxis of infections with susceptible anaerobic bacteria and protozoa. It is used frequently in combination with other antibiotics, proton pump inhibitors and bismuth as therapy of Helicobacter pylori infection. The recommended dosage is 500 to 750 mg taken orally three times daily for 5 to 10 days. Metronidazole is available alone in tablets of 250, 375, 500 and 750 mg as well as in combination with other medications, in multiple generic formulations and under several brand names including Flagyl, Metryl, Noritate, Pylera and Helida. Other formulations include injectable solutions, extended release tablets, suppositories, and topical creams. The most common side effects include metallic taste, nausea, vomiting, abdominal discomfort and diarrhea. Uncommon but potentially severe adverse events include seizures, neuropathy and encephalopathy, hypersensitivity reactions and Stevens-Johnson syndrome. Metronidazole has been found to be carcinogenic in rats and mice and long term and unwarranted use should be avoided.
Hepatotoxicity
Despite the wide use of metronidazole, only rare cases of hepatotoxicity have been reported, and metronidazole is not listed among causes of drug induced liver injury and acute liver failure in large case series. High doses of metronidazole given parenterally or in an overdose can cause elevations in serum aminotransferase levels, but these are usually self-limited and minimally symptomatic (Case 1). Acute, clinically apparent liver injury from metronidazole is rare. Ornidazole, another synthetic nitroimidazole that was available in Europe, was implicated in several cases of drug induced liver injury, with a latency of a few days or weeks and a hepatocellular pattern of injury. Metronidazole has been associated with a similar acute hepatitis-like syndrome with a short incubation period, but much more rarely. Fever, rash and eosinophilia are uncommon as are autoimmune features. A fatal recurrence of acute liver injury after reexposure to metronidazole has been published (Case 2). Strikingly, multiple instances of metronidazole hepatoxicity have been reported in the rare genetic disease, Cockayne syndrome in which there is an absence or deficiency in an important DNA repair enzyme responsible for nucleotide excision repair. The cases were marked by a short latency (1 to 7 days) to onset of jaundice, a hepatocellular pattern of enzyme elevations and severe course with a high mortality rate. Whether patients with Cockayne syndrome have a similar high risk for severe hepatitis with other nitroimidazoles (such as tinidazole) is not known.
Likelihood score: C (probable rare cause of clinically apparent liver injury).
Mechanism of Injury
The cause of acute liver injury due to metronidazole is probably immunoallergic, given the short latency period and recurrence with rechallenge. However, the frequency of severe hepatotoxicity in children with Cockayne syndrome suggests a direct toxic effect, probably involving breaks in double stranded DNA. Metronidazole is extensively metabolized in the liver and has multiple drug-drug interactions with agents that induce or inhibit cytochrome P450 enzymes (particularly CYP 3A4).
Outcome and Management
The liver injury from metronidazole is rare, but can result in liver failure and death. In typical cases, recovery is expected in 1 to 3 months. Rechallenge results in prompt recurrence and should be avoided. Patients with Cockayne syndrome should not receive metronidazole and should best avoid other nitroimidazole antibiotics such as tinidazole.
Drug Class: Antiinfective Agents; Gastrointestinal Agents
Other Drugs in the Subclass, Nitroimidazoles: Benznidazole, Secnidazole, Tinidazole
CASE REPORTS
Case 1. Elevations in serum aminotransferase levels during intravenous metronidazole therapy.(1)
A 58 year old man underwent prostate biopsy and cystoscopy and 32 hours later developed fever and was admitted for treatment of suspected urosepsis. After a combination of cephalosporin and tobramycin failed to affect his course, intravenous metronidazole (500 mg every 6 hours) was added. He had rapid clinical improvement, but then complained of abdominal pain, nausea, headache and a metallic taste. Metronidazole was stopped after 5 days and he was switched on oral cefaclor. At the same time, serum ALT and alkaline phosphatase levels were found to be elevated. Physical examination showed slight hepatomegaly without jaundice. Hepatitis B serology was negative. Over the following week, the patient recovered symptomatically and was discharged home. All laboratory tests were normal 4 weeks after stopping metronidazole.
Key Points
Laboratory Values
| Time After Starting | Time After Stopping | ALT (U/L) | Alk P (U/L) | Bilirubin (mg/dL) | Other |
|---|---|---|---|---|---|
| Pre | Pre | 65 | Prostate biopsy, cystoscopy | ||
| Fever 104 oF: cefapirin, tobramycin | |||||
| 0 | Start iv metronidazole | Continued fever | |||
| 5 days | 0 | Stop metronidazole | Started cefaclor | ||
| 6 days | 1 day | 720 | 200 | 0.4 | GGT 459 |
| 7 days | 2 days | 238 | 0.5 | ||
| 9 days | 4 days | 464 | 191 | 0.9 | |
| 10 days | 5 days | 319 | |||
| 2 weeks | 9 days | 167 | 71 | Discharged | |
| 4 weeks | 24 days | 42 | 80 | 0.3 | |
| Normal Values | <42 | <115 | <1.2 | ||
Comment
The serum enzyme elevations were compatible with mild metronidazole hepatotoxicity, given the short latency period and rapid recovery after stopping. The rapid onset and rapid recovery after high doses of intravenous metronidazole suggest direct hepatic injury. However, idiosyncratic cases are also marked by short latency period and rechallenge, even with oral metronidazole should be avoided.
Case 2. Acute hepatocellular injury due to metronidazole with fatal recurrence on reexposure.(2)
A 24 year old woman was treated with metronidazole for Clostridium difficile infection after a course of penicillin for a tooth abscess. Her diarrhea improved, but a few days later she developed nausea and vomiting followed by jaundice. Her past medical history included asthma and frequent upper respiratory infections. Laboratory tests showed total bilirubin of 7.9 mg/dL with marked elevations in serum aminotransferase levels, but modest increase in alkaline phosphatase (Table). Tests for hepatitis A, B and C and for autoantibodies were negative. An ultrasound showed no evidence of biliary obstruction. Metronidazole was discontinued and she began to improve, but her recovery was slow and symptoms persisted for at least two months and laboratory tests did not return to normal for at least nine months. Two years later, she was treated for bacterial vaginitis with metronidazole and tetracycline and one week later developed nausea, vomiting and jaundice. Serum bilirubin was 12.2 mg/dL, ALT and AST were more than 100 fold elevated, and prothrombin index was <9%. She was transferred to a liver transplant center where she developed progressive hepatic coma. Tests for hepatitis A, B and C were again negative. She underwent liver transplantation, but died in the perioperative period. Explant showed massive hepatic necrosis and cholestasis.
Key Points
| Medication: | Metronidazole (dose and duration not given) |
|---|---|
| Pattern: | Hepatocellular (R=62) |
| Severity: | 3+ initially (jaundice and hospitalization) 5+ on reexposure (liver transplantation, death) |
| Latency: | ~5-10 days |
| Recovery: | 10 months after initial exposure |
| Other medications: | Oral tetracycline |
Laboratory Values
| Time After Starting | Time After Stopping | ALT* (U/L) | Alk P (U/L) | Bilirubin (mg/dL) | Other |
|---|---|---|---|---|---|
| 0 | Metronidazole given for C difficile | ||||
| ~10 days | 0 | 5282 | 606 | 7.9 | |
| 15 days | 5 days | 3000 | 500 | 20.1 | |
| 1 mo | 1 mo | 104 | 450 | 10.5 | |
| 2.5 mos | 2.5 mos | 102 | 492 | 1.0 | |
| 9 mos | 9 mos | 84 | <300 | 1.0 | |
| 26 mos | Metronidazole given for bacterial vaginitis | ||||
| ~7 days | 0 | 11104 | 810 | 12.2 | Protime index < 9% |
| ~10 days | ~3 days | 20.5 | Liver transplant, post-operative death | ||
| Normal Values | <42 | <300 | <1.2 | ||
- *
Values estimated from Figure 1. Bilirubin results converted from mol to mg/dL (17.1) and enzyme results converted from kat to U/L (0.01667).
Comment
Severe acute hepatocellular injury from a short course of metronidazole with slow recovery, followed by a rapid and fatal recurrence on reexposure.
PRODUCT INFORMATION
REPRESENTATIVE TRADE NAMES
Metronidazole – Generic, Flagyl®
DRUG CLASS
Antiinfective Agents
Product labeling at DailyMed, National Library of Medicine, NIH
CHEMICAL FORMULA AND STRUCTURE
| DRUG | CAS REGISTRY NO | MOLECULAR FORMULA | STRUCTURE |
|---|---|---|---|
| Metronidazole | 443-48-1 | C6-H9-N3-O3 |
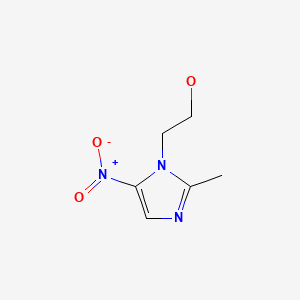
|
CITED REFERENCES
- 1.
- Appleby DH, Vogtland HD. Suspected metronidazole hepatotoxicity. Clin Pharm. 1983;2:373–4. [PubMed: 6883967]
- 2.
- Björnsson E, Nordlinder H, Olsson R. Metronidazol as a probable cause of severe liver injury. Hepatogastroenterology. 2002;49:252–4. [PubMed: 11941968]
ANNOTATED BIBLIOGRAPHY
References updated: 20 February 2020
- Zimmerman HJ. Amebicides. Hepatic injury from antimicrobial agents. In, Zimmerman HJ. Hepatotoxicity: the adverse effects of drugs and other chemicals on the liver. 2nd ed. Philadelphia: Lippincott, 1999, p. 592.(Expert review of liver injury published in 1999 mentions that metronidazole has only rarely been incriminated in causing liver injury).
- Moseley RH. Hepatotoxicity of antimicrobials and antifungal agents. In, Kaplowitz N, DeLeve LD, eds. Drug-induced liver disease. 3rd ed. Amsterdam: Elsevier, 2013, pp. 463-82.(Review of hepatotoxicity of antibiotics; does not discuss metronidazole).
- Wetzel DM, Phillips MA. Chemotherapy of protozoal infections. In, Brunton LL, Hilal-Dandan R, Knollman BC, eds. Goodman & Gilman’s the pharmacological basis of therapeutics. 13th ed. New York: McGraw-Hill, 20181, pp. 987-1000.(Textbook of pharmacology and therapeutics).
- Fagin ID. Jaundice associated with metronidazole. Letter to editor. JAMA. 1965;193:1128.(46 year old man developed fever after 4 days of metronidazole [250 mg/day] and he was given an injection of penicillin; 6 days later, he developed jaundice [bilirubin 5.4 mg/dL, AST 143 U/L, Alk P 1.5 times ULN], resolving in 2 months).
- Bonfiglio G, Donadio G. Results of the clinical testing of a new drug metronidazole in the treatment of chronic alcoholism. Br J Addict. 1967;62:249–55.(Open label trial of metronidazole [750 mg daily] in 60 patients with alcoholism for up to 45 days, most patients had flushing response to alcohol; no mention of hepatotoxicity or ALT elevations).
- Prospective, randomized comparison of metronidazole and clindamycin, each with gentamicin, for the treatment of serious intra-abdominal infection. Surgery. 1983;93(1 Pt 2):221–9. [No authors listed] [PubMed: 6849209](Multicenter study comparing clindamycin to metronidazole in 186 patients with severe infections; similar efficacy, AST elevations in 18% on metronidazole vs 10% on clindamycin, but no frank hepatitis or discontinuation for liver injury).
- Appleby DH, Vogtland HD. Suspected metronidazole hepatotoxicity. Clin Pharm. 1983;2:373–4. [PubMed: 6883967](58 year old man with urosepsis developed ALT [735 U/L] and Alk P [238 U/L] elevations without jaundice after 4 days of iv metronidazole, resolving in 1 week; also received tobramycin and cefapirin: Case 1).
- Uchihara M, Maeda M, Koyama W, Sakamoto S, Kanayama M. A case of metronidazole-induced liver injury. Acta Hepatol Jpn. 1984;25:1612–5.(35 year old man developed fever, abdominal discomfort, eosinophilia and enzymes elevations [bilirubin 1.6 mg/dL, ALT 478 U/L, Alk P 469 U/L] after 2 weeks of oral metronidazole, with positive lymphocyte stimulation test, recovery in 4 weeks).
- Smilack JD, Wilson WR, Cockerill FR 3rd. Tetracyclines, chloramphenicol, erythromycin, clindamycin, and metronidazole. Mayo Clin Proc. 1991;66:1270–80. [PubMed: 1749296](Review of uses and toxicities of antibiotics; no mention of hepatotoxicity of metronidazole).
- Hestin D, Hanesse B, Frimat L, Trechot P, Netter P, Kessler M. Metronidazole-associated hepatotoxicity in a hemodialyzed patient. Nephron. 1994;68:286. [PubMed: 7830880](68 year old woman developed nausea and right upper quadrant pain after 1 week of oral metronidazole therapy; ALT 650 U/L but no jaundice, resolved within 15 days of stopping).
- Lam S, Bank S. Hepatotoxicity caused by metronidazole overdose. Ann Intern Med. 1995;122:803. [PubMed: 7717611](58 year old woman took an overdose of metronidazole ~12.5 g and developed asymptomatic rise in ALT [to 2570 U/L], AST [6120 U/L], but minimal increase in Alk P [95 U/L] and bilirubin [2.1 mg/dL], levels peaking 2-3 days after overdose and resolving to normal within 4 weeks).
- Koşar Y, Sasmaz N, Oguz P, Kacar S, Erden E, Parlak E, Akdogan M. Ornidazole-induced autoimmune hepatitis. Eur J Gastroenterol Hepatol. 2001;13:737–9. [PubMed: 11434605](35 year old woman developed jaundice within a few days of starting oral ornidazole [bilirubin 17 mg/dL, ALT 1140 U/L, Alk P 145 U/L, SMA 1:1280], responding to corticosteroids with no relapse when therapy was stopped, but she was then retreated with ornidazole and promptly redeveloped a similar clinical picture with rise in SMA from 1:80 to 1:1280).
- Björnsson E, Nordlinder H, Olsson R. Metronidazol as a probable cause of severe liver injury. Hepatogastroenterology. 2002;49:252–4. [PubMed: 11941968](24 year old woman treated with metronidazole for pseudomembranous colitis developed symptoms and jaundice a few days later with progression to acute hepatitis [bilirubin 7.9 mg/dL, ALT 100 times ULN, Alk P 2 times ULN], with slow and incomplete recovery, and relapse and acute liver failure with retreatment with metronidazole 2 years later, the explant showing massive necrosis: Case 2).
- Tabak F, Ozaras R, Erzin Y, Celik AF, Ozbay G, Senturk H. Ornidazole-induced liver damage: report of three cases and review of the literature. Liver Int. 2003;23:351–4. [PubMed: 14708896](Ornidazole, a nitroimidazole derivative similar to metronidazole, was linked to 3 cases of acute hepatitis in women ages 25-50 years, arising after 3-4 days of therapy with ALT 977, 3042 and 1160 U/L; Alk P 1062, 422 and 431 U/L; bilirubin 32, 48 and 10 mg/dL, resolving in 1-2 months, no autoantibodies or allergic findings; 6 cases in literature, 4 icteric, 1 fatal).
- Orion E, Matz H, Wolf R. The life-threatening complications of dermatologic therapies. Clin Dermatol. 2005;23:182–92. [PubMed: 15802212](Review of serious complications of medications of skin disorders, mentions hepatotoxicity of metronidazole briefly).
- Chalasani N, Fontana RJ, Bonkovsky HL, Watkins PB, Davern T, Serrano J, Yang H, Rochon J., Drug Induced Liver Injury Network (DILIN). Causes, clinical features, and outcomes from a prospective study of drug-induced liver injury in the United States. Gastroenterology. 2008;135:1924–34. [PMC free article: PMC3654244] [PubMed: 18955056](Among 300 cases of drug induced liver disease in the US collected from 2004 to 2008, no case was attributed to metronidazole).
- Hussein R, El-Halabi M, Ghaith O, Jurdi N, Azar C, Mansour N, Sharara AI. Severe hepatotoxicity associated with the combination of spiramycin plus metronidazole. Arab J Gastroenterol. 2011;12:44–7. [PubMed: 21429456](Three men, ages 22 to 41 years, developed jaundice “a few weeks” to 2 months after treatment with a fixed combination of spiramycin and metronidazole [Rodogyl] for dental infections [bilirubin 28, 8.0 and 11.3 rising to 24 mg/dL, ALT 210, 1900 and 188 U/L, Alk P 109 and 344 U/L], one recovering spontaneously, one treated with prednisone and one undergoing emergency liver transplantation).
- Abdel Ghaffar TY, Elsobky ES, Elsayed SM. Cholestasis in patients with Cockayne syndrome and suggested modified criteria for clinical diagnosis. Orphanet J Rare Dis. 2011;6:13. [PMC free article: PMC3083330] [PubMed: 21477313](Among 9 patients with Cockayne syndrome followed at a single Egyptian referral center, 7 had at least one episode of transient liver injury, 4 with jaundice and 2 resulting in death, often following bacterial infections, an anesthetic agent being implicated in one instance).
- Kancherla D, Gajendran M, Vallabhaneni P, Vipperla K. Metronidazole induced liver injury: a rare immune mediated drug reaction. Case Rep Gastrointest Med. 2013;2013:568193. [PMC free article: PMC3884854] [PubMed: 24455335](54 year old man developed jaundice a few weeks after a 2 week course of metronidazole for Clostridium difficile associated diarrhea [bilirubin 7.2 mg/dL, ALT 973 U/L, Alk P 96 U/L, INR 1.9], with a severe and prolonged course, corticosteroid therapy, but eventual recovery).
- Björnsson ES, Bergmann OM, Björnsson HK, Kvaran RB, Olafsson S. Incidence, presentation and outcomes in patients with drug-induced liver injury in the general population of Iceland. Gastroenterology. 2013;144:1419–25. [PubMed: 23419359](In a population based study of drug induced liver injury from Iceland, 96 cases were identified over a 2 year period, but none of the 96 were attributed to metronidazole).
- Chalasani N, Bonkovsky HL, Fontana R, Lee W, Stolz A, Talwalkar J, Reddy KR, et al.; United States Drug Induced Liver Injury Network. Features and outcomes of 899 patients with drug-induced liver injury: The DILIN Prospective Study. Gastroenterology 2015; 148: 1340-52e7. [PMC free article: PMC4446235] [PubMed: 25754159](Among 899 cases of drug induced liver injury enrolled in a US prospective study between 2004 and 2013, none were attributed to metronidazole).
- Wilson BT, Strong A, O'Kelly S, Munkley J, Stark Z. Metronidazole toxicity in Cockayne syndrome: a case series. Pediatrics. 2015;136:e706–8. [PubMed: 26304821](Case series of 4 patients [ages 1-21 years; 3 girls, 1 boy] with Cockayne syndrome who developed jaundice and severe liver injury within 1-7 days of starting metronidazole usually in high doses [initial bilirubin 1.9-7.5 mg/dL, ALT 544-6206 U/L, Alk P 273-848 U/L, INR 1.4->10], 3 dying and 1 surviving after a prolonged course).
- Blumenthal KG, Youngster I, Rabideau DJ, Parker RA, Manning KS, Walensky RP, Nelson SB. Peripheral blood eosinophilia and hypersensitivity reactions among patients receiving outpatient parenteral antibiotics. J Allergy Clin Immunol 2015; 136: 1288-94. e1. [PMC free article: PMC4640981] [PubMed: 25981739](Among 824 patients receiving outpatient parenteral antibiotic therapy who had concurrent white blood cell and differential counts, eosinophilia [>500 cells/uL] was found in 25%, being most common with vancomycin [30%], the penicillins [28%], carbapenems [28%], cephalosporins [22%], fluoroquinolones [21%], and less common with metronidazole [15%] and there was no association of eosinophilia with liver test abnormalities).
- Mazuski JE, Gasink LB, Armstrong J, Broadhurst H, Stone GG, Rank D, Llorens L, et al. Efficacy and safety of ceftazidime-avibactam plus metronidazole versus meropenem in the treatment of complicated intra-abdominal infection: results from a randomized, controlled, double-blind, phase 3 program. Clin Infect Dis. 2016;62:1380–9. [PMC free article: PMC4872289] [PubMed: 26962078](In a randomized trial of ceftazidime/avibactam and metronidazole vs meropenem only for complicated intra-abdominal infections, cure rates were similar for the two regimens [82% vs 85%] as were adverse events including “liver disorders” of 2.1% vs 1.5%).
- Drugs for Helicobacter pylori infection. Med Lett Drugs Ther. 2017;59(1525):113–7. [PubMed: 28699931](Concise review of the efficacy, safety and costs of drugs for H. pylori infection lists preferred regimens, usually includes metronidazole [500 mg twice daily for 10-14 days] whose adverse effects can include metallic taste, reactions to alcohol, seizures and neuropathy).
- Zhao Z, Bao L, Yu X, Zhu C, Xu J, Wang Y, Yin M, et al. Acute vanishing bile duct syndrome after therapy with cephalosporin, metronidazole, and clotrimazole: A case report. Medicine (Baltimore). 2017;96:e8009. [PMC free article: PMC6392967] [PubMed: 28885366](29 year old woman developed progressive, severe cholestasis and bile duct loss attributed to a 4-5 day course of antibiotics, reportedly “a cephalosporin”, metronidazole and clotrimazole).
- Pandey S, Gupta GK, Wanjari SJ, Nijhawan S. Comparative study of tinidazole versus metronidazole in treatment of amebic liver abscess: A randomized control trial. Indian J Gastroenterol. 2018;37:196–201. [PubMed: 29948994](Among 150 patients with amebic liver abscess treated with metronidazole [14 days] or tinidazole [5 days], time to response was better with tinidazole but ultimate response rates were similar, although metronidazole was associated with a higher rate of adverse events including nausea, vomiting and metallic taste resulting in early discontinuation in 10%; no mention of ALT elevations or hepatotoxicity).
- Shamberg L, Vaziri H. Hepatotoxicity of inflammatory bowel disease medications. J Clin Gastroenterol. 2018;52:674–84. [PubMed: 30036242](Review of the hepatotoxicity of drugs used for inflammatory bowel disease mentions that metronidazole has been reported to cause liver injury but it is rare and does not justify prospective monitoring during therapy).
- Ataee P, Karimi A, Eftekhari K. Hepatic failure following metronidazole in children with Cockayne syndrome. Case Rep Pediatr. 2020;2020:9634196. [PMC free article: PMC7008298] [PubMed: 32082677](Two cases: 2 and 5 years old boys with type B [infant onset] Cockayne syndrome developed jaundice, vomiting and agitation 2 and 3 days after starting oral metronidazole for minor infection [bilirubin 13.7 and 16.0 mg/dL, ALT 2815 and 2248 U/L, Alk P 1265 and 1654 U/L, INR 5.1 and 4.6], one dying within 2 days of admission and the second recovering but with persistent jaundice and serum enzyme elevations one month later).
- PMCPubMed Central citations
- PubChem SubstanceRelated PubChem Substances
- PubMedLinks to PubMed
- Review Symposium on antimicrobial agents. Metronidazole.[Mayo Clin Proc. 1987]Review Symposium on antimicrobial agents. Metronidazole.Rosenblatt JE, Edson RS. Mayo Clin Proc. 1987 Nov; 62(11):1013-7.
- Metronidazole.[Mayo Clin Proc. 1983]Metronidazole.Rosenblatt JE, Edson RS. Mayo Clin Proc. 1983 Mar; 58(3):154-7.
- Review Tinidazole.[LiverTox: Clinical and Researc...]Review Tinidazole.. LiverTox: Clinical and Research Information on Drug-Induced Liver Injury. 2012
- Review Pharmacokinetics and pharmacodynamics of the nitroimidazole antimicrobials.[Clin Pharmacokinet. 1999]Review Pharmacokinetics and pharmacodynamics of the nitroimidazole antimicrobials.Lamp KC, Freeman CD, Klutman NE, Lacy MK. Clin Pharmacokinet. 1999 May; 36(5):353-73.
- Metronidazole: in vitro activity, pharmacology and efficacy in anaerobic bacterial infections.[Pharmacotherapy. 1981]Metronidazole: in vitro activity, pharmacology and efficacy in anaerobic bacterial infections.Tally FP, Sullivan CE. Pharmacotherapy. 1981 Jul-Aug; 1(1):28-38.
- Metronidazole - LiverToxMetronidazole - LiverTox
Your browsing activity is empty.
Activity recording is turned off.
See more...