NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
LiverTox: Clinical and Research Information on Drug-Induced Liver Injury [Internet]. Bethesda (MD): National Institute of Diabetes and Digestive and Kidney Diseases; 2012-.

LiverTox: Clinical and Research Information on Drug-Induced Liver Injury [Internet].
Show detailsOVERVIEW
Introduction
Cyclosporine is a calcineurin inhibitor and potent immunosuppressive agent used largely as a means of prophylaxis against cellular rejection after solid organ transplantation. Cyclosporine therapy can be associated with mild elevations in serum bilirubin and transient serum enzyme elevations, and to rare instances of clinically apparent cholestatic liver injury.
Background
Cyclosporine (sye" kloe spor' in), also called cyclosporin A, is a cyclic polypeptide of 11 amino acids produced by a fungal species (Beauveria nivea) which has profound immunosuppressive properties, particularly affecting T cells and the cellular immune response. Cyclosporine acts as an inhibitor of calcineurin which is responsible for activating an important signal transduction pathway of T cell activation. The result of the inhibition is a decrease in maturation of T lymphocytes and reduction in lymphokine production, including IL-2. Cyclosporine was introduced into use in the United States in the early 1980s and rapidly became part of the primary regimen of immunosuppression after allogenic, solid organ transplantation. Current indications are for prevention of organ rejection after transplantation and for therapy of active and recalcitrant rheumatoid arthritis and psoriasis. Cyclosporine is available as capsules of 25 and 100 mg in generic forms and under the brand name of Sandimmune, and as a more reliably absorbed microemulsion formulation of 25 and 100 mg in generic forms and under the brand name of Neoral (2003). Cyclosporine is also available in solution for oral and for intravenous use. Because of variable absorption, the usual maintenance dose of cyclosporine varies greatly and proper dosing requires monitoring for drug levels, which is also important because of its many dose dependent side effects and drug-drug interactions. Common side effects of cyclosporine include headache, dizziness, paresthesias, neuropathy, tremor, hypertension, hyperlipidemia, nephropathy, acne, hirsutism and gum hyperplasia. Uncommon but potentially severe adverse events include renal failure, microangiopathic hemolytic anemia, neurotoxicity, serious and opportunistic infections, increase risk of malignancy and anaphylactic reactions. Oral and parenteral cyclosporine should be prescribed only by physicians experienced in immunosuppressive therapy and management of its complications.
Hepatotoxicity
In several large clinical trials, initiation of cyclosporine therapy was associated with mild elevations in serum bilirubin levels, often without significant increases in serum ALT or alkaline phosphatase. Elevations in serum enzymes were also described, but less commonly. Recently, these complications appear to be less frequent, perhaps because of more careful dosing and monitoring of cyclosporine levels. Furthermore, in treatment of autoimmune diseases without the many complications of transplantation, cyclosporine therapy has been associated with mild serum alkaline phosphatase elevations in up to 30% of patients, but the abnormalities are asymptomatic, usually self-limiting and rarely require dose adjustment. In several case series, cyclosporine therapy has also been associated with biliary sludge and cholelithiasis. Isolated case reports of clinically apparent acute liver injury have been attributed to cyclosporine. The time to onset was within a few weeks of starting cyclosporine and the pattern of serum enzyme elevations was cholestatic. Recovery was prompt once cyclosporine was stopped and cases of chronic hepatitis or acute liver failure due to cyclosporine have not been reported.
Likelihood score: C (probable rare cause of clinically apparent liver injury).
Mechanism of Injury
Cyclosporine undergoes extensive hepatic metabolism and because of its interaction with the cytochrome P450 system (CYP 3A4) is susceptible to severe drug-drug interactions. In animal models, cyclosporine decreases bile flow which may account for the mild hyperbilirubinemia that occurs with high doses.
Outcome and Management
The serum bilirubin and liver enzyme elevations that can accompany cyclosporine use are usually mild, asymptomatic and self-limiting; if not, they usually resolve rapidly upon dose reduction. The rare instances of cholestatic liver injury due to cyclosporine usually resolve with discontinuation and most (but not all) patients can tolerate switching to tacrolimus. Cyclosporine has not been associated with instances of acute liver failure or vanishing bile duct syndrome.
Agents used specifically for the prophylaxis against allograft rejection include cyclosporine, mycophenolate mofetil, sirolimus and tacrolimus, as well as azathioprine and corticosteroids.
Drug Class: Transplant Agents; Antirheumatic Agents, Major Immunosuppressive Agents; Dermatologic Agents
Other Drugs in the Class, Transplant Drugs: Mycophenolate, Sirolimus, Tacrolimus
PRODUCT INFORMATION
REPRESENTATIVE TRADE NAMES
Cyclosporine – Generic, Neoral®, Sandimmune®
DRUG CLASS
Dermatologic Agents; Transplant Agents
Product labeling at DailyMed, National Library of Medicine, NIH
CHEMICAL FORMULA AND STRUCTURE
| DRUG | CAS REGISTRY NUMBER | MOLECULAR FORMULA | STRUCTURE |
|---|---|---|---|
| Cyclosporine | 59865-13-3 | C62-H111-N11-O12 |
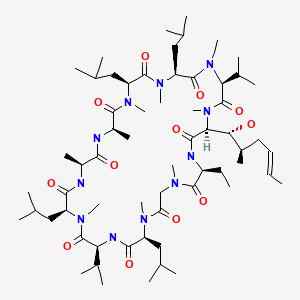
|
ANNOTATED BIBLIOGRAPHY
References updated: 17 February 2020
- Zimmerman HJ. Cyclosporine. Oncotherapeutic and immunosuppressive agents. In, Zimmerman HJ. Hepatotoxicity: the adverse effects of drugs and other chemicals on the liver. 2nd ed. Philadelphia: Lippincott, 1999, pp. 697-8.(Expert review of hepatotoxicity published in 1999; cyclosporine therapy is associated with a high rate of cholestatic liver enzyme elevations ranging from 4-86% and occasional instances of cholestatic hepatitis, some features of which are reproducible in animal models; tacrolimus, sirolimus, and mycophenolate are not discussed).
- Reuben A. Hepatotoxicity of immunosuppressive drugs. In, Kaplowitz N, DeLeve LD, eds. Drug-induced liver disease. 3rd ed. Amsterdam: Elsevier, 2013, pp. 569-92.(Review of hepatotoxicity of immunosuppressive agents mentions that reports of hepatotoxicity of cyclosporine have decreased since the 1980s, perhaps because of monitoring of serum levels and lower doses used; liver injury from tacrolimus, sirolimus and mycophenolate is rare and usually rapidly reversible).
- Krensky AM, Azzi JR, Hafler DA. Immnosuppressants and tolerogens. In, Brunton LL, Hilal-Dandan R, Knollman BC, eds. Goodman & Gilman's the pharmacological basis of therapeutics. 13th ed. New York: McGraw-Hill, 2018, pp. 637-54.(Textbook of pharmacology and therapeutics).
- Calne RY, Rolles K, White DJ, Thiru S, Evans DB, McMaster P, Dunn DC, et al. Cyclosporin A initially as the only immunosuppressant in 34 recipients of cadaveric organs, 32 kidneys, 2 pancreas, and 2 livers. Lancet. 1979;2:1033–6. [PubMed: 91781](Initial experience with cyclosporine in 34 transplant recipients; all but 2 patients had liver test abnormalities early after operation, mostly raised bilirubin and Alk P resolving with lowering dose).
- Starzl TE, Klintmalm GB, Weil R 3rd, Porter KA, Iwatsuki S, Schroter GP, Fernandez-Bueno C, et al. Cyclosporin A and steroid therapy in sixty-six cadaver kidney recipients. Surg Gynecol Obstet. 1981;153:486–94. [PMC free article: PMC2671391] [PubMed: 6269238](Early experience in using cyclosporine in 66 renal transplant recipients; two patents were switched to azathioprine because of hepatotoxicity, and liver function abnormalities occurred in 13 patients [20%], but no details given).
- Loertscher R, Wenk M, Harder F, Brunner F, Follath F, Thiel G. Hyperbilirubinaemia and cyclosporin A levels in renal transplant patients. Lancet. 1981;2:635–6. [PubMed: 6116111](Among 8 patients receiving cyclosporine after renal transplantation, there was only a loose association between bilirubin and cyclosporine levels, serum bilirubin being elevated in 5 patients and decreasing with dose reduction [peak 4.2 mg/dL]).
- Laupacis A, Keown PA, Ulan RA, Sinclair NR, Stiller CR. Hyperbilirubinaemia and cyclosporin A levels. Lancet. 1981;2:1426–7. [PubMed: 6118798](4 of 21 renal transplant recipients developed elevations in serum bilirubin [1.1-4.5 mg/dL] 4-12 days after transplant, which correlated with higher cyclosporine levels).
- Klintmalm GB, Iwatsuki S, Starzl TE. Cyclosporin A hepatotoxicity in 66 renal allograft recipients. Transplantation 1981; 32:4 88-9. [PMC free article: PMC2962575] [PubMed: 7041349](Among 66 renal transplant recipients on cyclosporine, 13 [17%] had rise of bilirubin above 2.0 [range 2.1-4.5] mg/dL, with minimal or no change in ALT or Alk P, and all episodes were mild and easily managed by dose reduction).
- Ferguson RM, Rynasiewicz JJ, Sutherland DE, Simmons RL, Najarian JS. Cyclosporin A in renal transplantation: a prospective randomized trial. Surgery. 1982;92:175–82. [PubMed: 6285533](Controlled trial of cyclosporine and prednisone vs azathioprine, prednisone and antilymphocyte globulin in 100 renal transplant patients, hepatotoxicity was uncommon and mild; 3 of 48 patients on cyclosporine had mild bilirubin elevations [1.6-2.5 mg/dL], which were rapidly reversible with dose adjustment).
- Rodger S, Turney JH, Haynes I, McMaster P, Michael J, Adu D. Normal liver function in renal allograft recipients treated with cyclosporine. Transplantation. 1983;36:451–2. [PubMed: 6353712](Among 35 renal transplant recipients, liver test abnormalities arose in 8 including 4 of 21 on cyclosporine, but other causes were found to be the cause in all eight [infection or heart failure]).
- European Multicentre Trial Group. Cyclosporine in cadaveric renal transplantation: one-year follow-up of a multicentre trial. Lancet. 1983;2:986–9. [PubMed: 6138592](Controlled trial of cyclosporine vs azathioprine and corticosteroids in 232 transplant recipients showing improved graft survival with cyclosporine; "mild, clinically insignificant degrees of hepatic functional impairment were observed in some cyclosporine-treated patients").
- Canadian Multicenter Transplant Study Group. A randomized clinical trial of cyclosporine in cadaveric renal transplantation. N Engl J Med. 1983;309:809–15. [PubMed: 6350878](Controlled trial of cyclosporine vs azathioprine and corticosteroids in 209 transplant recipients showing improved graft survival; 4 instances of hepatotoxicity occurred in cyclosporine recipients usually associated with high plasma levels).
- Najarian JS, Strand M, Fryd DS, Ferguson RM, Simmons RL, Ascher NL, Sutherland DER. Comparison of cyclosporine versus azathioprine-antilymphocyte globulin in renal transplantation. Transplant Proc. 1983;15(4) Suppl 1:2463–8.
- Schade RR, Guglielmi A, van Thiel DH, Thompson ME, Warty V, Griffith B, Sanghvi A, et al. Cholestasis in heart transplant recipients treated with cyclosporine. Transplant Proc. 1983;15(4) Suppl 1:2757–60.
- Atkinson K, Biggs J, Dodds A, Concannon A. Cyclosporine-associated hepatotoxicity after allogeneic marrow transplantation in man: differentiation from other causes of posttransplant liver disease. Transplant Proc. 1983;15(4) Suppl 1:2761–7.
- Cohen DJ, Loertscher R, Rubin MF, Tilney NL, Carpenter CB, Strom TB. Cyclosporine: a new immunosuppressive agent for organ transplantation. Ann Intern Med. 1984;101:667–82. [PubMed: 6385799](Review of mechanism of action, clinical experience and side effects of cyclosporine; elevations in serum bilirubin reported in 20% of patients on cyclosporine after transplant, enzyme elevations were uncommon and "clinically, hepatotoxicity has been of little significance").
- Palestine AG, Nussenblatt RB, Chan CC. Side effects of systemic cyclosporine in patients not undergoing transplantation. Am J Med. 1984;77:652–6. [PubMed: 6486141](Among 22 patients with autoimmune uveitis treated with cyclosporine, side effects were fewer and less severe than after transplantation; only one patient had elevations in serum bilirubin [peak 1.6 mg/dL] and aminotransferase elevations did not occur).
- Welz A, Reichart B, Uberfuhr P, Kemkes B, Klinner W. Cyclosporine as the main immunosuppressant in clinical heart transplantation: correlation of hepatotoxicity and nephrotoxicity. Transplant Proc. 1984;16:1212–3. [PubMed: 6385381](Among 10 patients undergoing heart transplantation and receiving cyclosporine, five with preexisting hepatic congestion had higher cyclosporine levels and higher serum bilirubin levels than the 5 without preexisting liver abnormalities [mean peak 5.8 vs 1.3 mg/dL]).
- McKenzie FN, Moses GC, Henderson AR. Routine "cardiac" and "hepatic" serum enzyme profiles in cardiac transplant patients treated with cyclosporine A: operative and postoperative findings. Clin Chem. 1985;31:822–5. [PubMed: 2859934](Prospective study of liver test abnormalities in 20 heart transplant recipients receiving cyclosporine found that transient elevations in ALT and AST were common during the 2 weeks after transplant).
- Jensen CW, Flechner SM, Van Buren CT, Frazier OH, Cooley DA, Lorber MI, Kahan BD. Exacerbation of cyclosporine toxicity by concomitant administration of erythromycin. Transplantation. 1987;43:263–70. [PubMed: 3544386](Concurrent erythromycin led to elevations in cyclosporine levels and more toxicity in 9 transplant recipients, median serum bilirubin levels being 1.2 before, 2.1 during and 0.8 mg/dL after a course of the macrolide antibiotic).
- Stone BG, Udani M, Sanghvi A, Warty V, Plocki K, Bedetti CD, Van Thiel DH. Cyclosporin A-induced cholestasis. The mechanism in a rat model. Gastroenterology. 1987;93:344–51. [PubMed: 3596172](In rats, cyclosporine led to decrease in bile flow [35%] and rise in serum bile acid levels without change in ALT or bilirubin).
- Kahan BD, Flechner SM, Lorber MI, Golden D, Conley S, Van Buren CT. Complications of cyclosporine-prednisone immunosuppression in 402 renal allograft recipients exclusively followed at a single center for from one to five years. Transplantation. 1987;43:197–204. [PubMed: 3544376](Retrospective analysis of complications of cyclosporine in 402 renal transplant recipients; 50% had at least one liver test abnormality in first month, 20% at one year and 10% at 3 years; no details given).
- Lorber MI, Van Buren CT, Flechner SM, Williams C, Kahan BD. Hepatobiliary and pancreatic complications of cyclosporine therapy in 466 renal transplant recipients. Transplantation. 1987;43:35–40. [PubMed: 3541320](Among 466 patients undergoing renal transplantation, 49% developed liver test abnormalities after transplant [bilirubin in 48%, ALT 73%, Alk P 59%], but abnormalities were usually early [<90 days], mild and self-limiting; among 32 with persistent abnormalities, 11 had cholelithiasis).
- Gulbis B, Adler M, Ooms HA, Desmet JM, Leclerc JL, Primo G. Liver-function studies in heart-transplant recipients treated with cyclosporin A. Clin Chem. 1988;34:1772–4. [PubMed: 2901299](Prospective study of liver tests in 17 heart transplant recipients found rises in bile acid and GGT levels only, which occurred only in those with preexisting liver injury).
- Cadranel JF, Grippon P, Mattei MF, Lunel F, Pauwels A, Rossant P, Karkouche B, et al. Prevalence and causes of long-lasting hepatic dysfunction after heart transplantation: a series of 80 patients. Artif Organs. 1988;12:234–8. [PubMed: 3291831](Among 80 heart transplant recipients, 62% had persistent liver test abnormalities, usually due to heart failure [9%], hepatitis B [26%], non-A, non-B hepatitis [28%] and drug [not cyclosporine] induced liver injury [14%]).
- Kassianides C, Nussenblatt R, Palestine AG, Mellow SD, Hoofnagle JH. Liver injury from cyclosporine A. Dig Dis Sci. 1990;35:693–7. [PubMed: 2344802](Retrospective analysis of liver test abnormalities arising in 59 patients with autoimmune uveitis being treated with cyclosporine; persistent biochemical evidence of mild cholestasis [Alk P and bilirubin elevations] occurred in 32% of patients, but was usually self-limited and asymptomatic, improving spontaneously or with dose modification in all cases).
- Rush DN. Cyclosporine toxicity to organs other than the kidney. Clin Biochem. 1991;24:101–5. [PubMed: 2060127](Review of mechanism of toxicity of cyclosporine; hyperbilirubinemia may be caused by inhibition of bile flow).
- Wisecarver JL, Earl RA, Haven MC, Timmins PW, Shaw BW Jr, Stratta RJ, Langnas AN, et al. Histologic changes in liver allograft biopsies associated with elevated whole blood and tissue cyclosporine concentrations. Mod Pathol. 1992;5:611–6. [PubMed: 1369795](Among 16 patients on cyclosporine after liver transplantation, histology of liver showed minor abnormalities of bile duct epithelium).
- Demetris AJ, Fung JJ, Todo S, McCauley J, Jain A, Takaya S, Alessiani M, et al. Conversion of liver allograft recipients from cyclosporine to FK506 immunosuppressive therapy - a clinicopathologic study of 96 patients. Transplantation. 1992;53:1056–62. [PMC free article: PMC2962565] [PubMed: 1374944](Switching patients from cyclosporine to tacrolimus often improved acute rejection, but rarely improved chronic liver injury or suspected hepatotoxicity).
- Mor E, Sheiner PA, Schwartz ME, Emre S, Guy S, Miller CM. Reversal of severe FK506 side effects by conversion to cyclosporine-based immunosuppression. Transplantation. 1994;58:380–2. [PubMed: 7519800](Severe side effects of tacrolimus therapy requiring dose modification or switching to cyclosporine occurred in 15 of 90 patients [17%] including nephropathy, diabetes and neuropathy, but not hepatotoxicity).
- Jazzar A, Fagiuoli S, Caraceni P, Deal S, Wright HI, Sisson S, Gavaler J, et al. Incidence and etiology of hepatic dysfunction in heart transplant recipients receiving a cyclosporine-based triple immunosuppressive therapy. Transplant Proc. 1994;26:2654. [PubMed: 7940829](Among 100 heart transplant recipients, 52 had abnormal liver tests, causes being viral hepatitis in 27%, azathioprine in 54%, unknown in 23% which were usually mild and spontaneously reversible).
- Kowdley KV, Keeffe EB. Hepatotoxicity of transplant immunosuppressive agents. Gastroenterol Clin North Am. 1995;24:991–1001. [PubMed: 8749908](Review of reports of hepatotoxicity from cyclosporine in form of mild hyperbilirubinemia, mild-to-moderate serum enzyme elevations and biliary sludge and stones).
- Moore RA, Greenberg E, Tangen L. Cyclosporine-induced worsening of hepatic dysfunction in a patient with Crohn's disease and enterocutaneous fistula. South Med J. 1995;88:843–4. [PubMed: 7631211](44 year old man with severe Crohn disease on total parenteral nutrition [TPN] developed marked bilirubin rises after starting cyclosporine [from 4.7 to 17.5 mg/dL], which resolved upon stopping both cyclosporine and TPN).
- Ertörer ME, Paydaş S, Sagliker Y. Hyperbilirubinemia in a renal transplant patient due to cyclosporin A therapy. Nephron. 1997;76:368. [PubMed: 9226250](50 year old male renal transplant recipient developed jaundice and fever [bilirubin 6.0 mg/dL, ALT 20 U/L, Alk P 263 U/L], resolving on stopping cyclosporine and recurring 3 months after restarting [bilirubin 3.4 mg/dL, ALT 72 U/L, Alk P 400 U/L], resolving within 2 weeks of stopping).
- Tsamandas AC, Jain AB, Felekouras ES, Fung JJ, Demetris AJ, Lee RG. Central venulitis in the allograft liver: a clinicopathologic study. Transplantation. 1997;64:252–7. [PubMed: 9256183](Among 27 patients with central venulitis receiving cyclosporine or tacrolimus, there was no association with drug levels and the histological lesion was attributed to rejection rather than drug induced liver injury).
- Ngo MD, Hagè H, Rosa I, Cartier VA, Lons T, Gordin J, Chousterman M. Presse Med. 1999;28:1873–5. [Acute hepatitis in the course of cyclosporine therapy of Crohn's disease] French. [PubMed: 10587720](26 year old woman with Crohn's disease on total parenteral nutrition developed marked rises in ALT [30 times ULN] and minimal increase in Alk P and bilirubin 1 week after starting cyclosporine, resolving within 2 weeks of stopping; multiple other drugs given).
- Yuan QS, Zheng FL, Sun Y, Yu Y, Li Y. Rescue therapy with tacrolimus in renal graft patients with cyclosporine A-induced hepatotoxicity: a preliminary study. Transplant Proc. 2000;32:1694–5. [PubMed: 11119896](7 renal transplant recipients with suspected cyclosporine hepatotoxicity were switched to tacrolimus, ALT levels decreased from 28-119 to 24-43 U/L; no mention of bilirubin, Alk P or symptoms).
- Emre S, Genyk Y, Schluger LK, Fishbein TM, Guy SR, Sheiner PA, Schwartz ME, et al. Treatment of tacrolimus-related adverse effects by conversion to cyclosporine in liver transplant recipients. Transpl Int. 2000;13:73–8. [PubMed: 10743694](Among 388 liver transplant recipients treated with tacrolimus, 70 required conversion to cyclosporine because of side effects, including 6 for late hepatotoxicity, often for steatohepatitis or recurrent autoimmune hepatitis, with improvement in 4).
- Russo MW, Galanko JA, Shrestha R, Fried MW, Watkins P. Liver transplantation for acute liver failure from drug-induced liver injury in the United States. Liver Transpl. 2004;10:1018–23. [PubMed: 15390328](Among ~50,000 liver transplants reported to UNOS between 1990 and 2002, 270 [0.5%] were done for drug induced acute liver failure, 124 for acetaminophen and 137 for other drugs or toxins, but none for agents used to prevent transplant rejection).
- Ganschow R, Albani J, Grabhorn E, Richter A, Burdelski M. Tacrolimus-induced cholestatic syndrome following pediatric liver transplantation and steroid-resistant graft rejection. Pediatr Transplant. 2006;10:220–4. [PubMed: 16573611](Among 112 children undergoing liver transplantation and switched from cyclosporine to tacrolimus because of steroid resistant rejection, 6 [5.4%] developed a cholestatic syndrome within 2 weeks of change of medications).
- Taniai N, Akimaru K, Ishikawa Y, Kanada T, Kakinuma D, Mizuguchi Y, Mamada Y, et al. Hepatotoxicity caused by both tacrolimus and cyclosporine after living donor liver transplantation. J Nippon Med Sch. 2008;75:187–91. [PubMed: 18648179](56 year old liver transplant recipient developed fluctuating ALT elevations [averaging 200-300 U/L] and bilirubin elevations [peak 11 mg/dL] that were not explained by rejection or infection and appeared to respond transiently to changing from tacrolimus to cyclosporine and then recurring, ultimately treated with lower doses of tacrolimus and mycophenolate).
- Chalasani N, Fontana RJ, Bonkovsky HL, Watkins PB, Davern T, Serrano J, Yang H, Rochon J., Drug Induced Liver Injury Network (DILIN). Causes, clinical features, and outcomes from a prospective study of drug-induced liver injury in the United States. Gastroenterology. 2008;135:1924–34. [PMC free article: PMC3654244] [PubMed: 18955056](Among 300 cases of drug induced liver disease in the US collected between 2004 and 2008, none were attributed to cyclosporine, tacrolimus, sirolimus or mycophenolate).
- Reuben A, Koch DG, Lee WM., Acute Liver Failure Study Group. Drug-induced acute liver failure: results of a U.S. multicenter, prospective study. Hepatology. 2010;52:2065–76. [PMC free article: PMC3992250] [PubMed: 20949552](Among 1198 patients with acute liver failure enrolled in a US prospective study between 1998 and 2007, 133 were attributed to drug induced liver injury, but none to an agent used to prevent transplant rejection).
- Björnsson ES, Bergmann OM, Björnsson HK, Kvaran RB, Olafsson S. Incidence, presentation and outcomes in patients with drug-induced liver injury in the general population of Iceland. Gastroenterology. 2013;144:1419–25. [PubMed: 23419359](In a population based study of drug induced liver injury from Iceland, 96 cases were identified over a 2 year period, none of which were attributed to an anti-rejection agent used in transplantation).
- Hernández N, Bessone F, Sánchez A, di Pace M, Brahm J, Zapata R, A, Chirino R, et al. Profile of idiosyncratic drug induced liver injury in Latin America: an analysis of published reports. Ann Hepatol. 2014;13:231–9. [PubMed: 24552865](Among 176 reports of drug induced liver injury from Latin America published between 1996 and 2012, one was attributed to mycophenolate but none to cyclosporine, sirolimus or tacrolimus).
- Ko MS, Choi YH, Jung SH, Lee JS, Kim HS, Lee CH, Kim SG. Tacrolimus therapy causes hepatotoxicity in patients with a history of liver disease. Int J Clin Pharmacol Ther. 2015;53:363–71. [PubMed: 25740263](Analysis of electronic medical records from 2462 Korean patients with a history of liver taking tacrolimus or cyclosporine from 2002-2008, found that peak ALT levels were higher [50 vs 41 U/L] and time to peak was shorter [101 vs 142 days] in the tacrolimus treated patients).
- Chalasani N, Bonkovsky HL, Fontana R, Lee W, Stolz A, Talwalkar J, Reddy KR, et al.; United States Drug Induced Liver Injury Network. Features and outcomes of 899 patients with drug-induced liver injury: The DILIN Prospective Study. Gastroenterology 2015; 148: 1340-52. e7. [PMC free article: PMC4446235] [PubMed: 25754159](Among 899 cases of drug induced liver injury enrolled in a US prospective study between 2004 and 2013, one case was attributed to cyclosporine, but none to tacrolimus, sirolimus or mycophenolate mofetil).
- Fiore M, Leone S, Maraolo AE, Berti E, Damiani G. Liver Illness and Psoriatic Patients. Biomed Res Int. 2018;2018:3140983. [PMC free article: PMC5818942] [PubMed: 29546055](Review of liver disease in psoriasis including drug induced liver injury due to methotrexate, acitretin, TNF inhibitors, cyclosporine, and leflunomide).
- PMCPubMed Central citations
- PubChem SubstanceRelated PubChem Substances
- PubMedLinks to PubMed
- Review Tacrolimus.[LiverTox: Clinical and Researc...]Review Tacrolimus.. LiverTox: Clinical and Research Information on Drug-Induced Liver Injury. 2012
- Review Sirolimus.[LiverTox: Clinical and Researc...]Review Sirolimus.. LiverTox: Clinical and Research Information on Drug-Induced Liver Injury. 2012
- Review Everolimus.[LiverTox: Clinical and Researc...]Review Everolimus.. LiverTox: Clinical and Research Information on Drug-Induced Liver Injury. 2012
- Review Muromonab-CD3.[LiverTox: Clinical and Researc...]Review Muromonab-CD3.. LiverTox: Clinical and Research Information on Drug-Induced Liver Injury. 2012
- Review Transplant Agents.[LiverTox: Clinical and Researc...]Review Transplant Agents.. LiverTox: Clinical and Research Information on Drug-Induced Liver Injury. 2012
- Cyclosporine - LiverToxCyclosporine - LiverTox
Your browsing activity is empty.
Activity recording is turned off.
See more...