NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
LiverTox: Clinical and Research Information on Drug-Induced Liver Injury [Internet]. Bethesda (MD): National Institute of Diabetes and Digestive and Kidney Diseases; 2012-.

LiverTox: Clinical and Research Information on Drug-Induced Liver Injury [Internet].
Show detailsOVERVIEW
Introduction
Sirolimus is macrocyclic antibiotic with potent immunosuppressive activity that is used alone or in combination with calcineurin inhibitors and corticosteroids to prevent cellular rejection after renal transplantation. Sirolimus therapy can be associated with mild serum enzyme elevations and it has been linked to rare instances of clinically apparent cholestatic liver injury.
Background
Sirolimus (sir oh' li mus) is a macrocyclic lactone antibiotic which also has profound immunosuppressive properties particularly affecting T cells and the cellular immune response. Sirolimus binds to the same intracellular receptor as tacrolimus and cyclosporine, but does not inhibit calcineurin, but rather blocks the “mammalian target of rapamycin” (mTOR) which interrupts signaling pathways for several cytokines and growth factors including IL2. The result of the inhibition is inactivation of T cells. Sirolimus was approved for use in the United States in 1999 and current indications are for prevention of organ rejection after renal transplantation alone or in combination with calcineurin inhibitors or corticosteroids. It is also approved as therapy for lymphangioleiomyomatosis. Sirolimus has not been approved for use in liver or lung transplantation but is used off-label for prevention of rejection after other forms of organ transplantation after failure or intolerance to tacrolimus. Sirolimus is available as tablets of 0.5, 1 and 2 mg and in an oral solution of 1 mg/mL generically and under the brand name of Rapamune. After a loading dose, the usual maintenance dose in adults is 2 mg (~1 mg/m2) once daily. Sirolimus has less nephrotoxicity than the calcineurin inhibitors. Common side effects of sirolimus include anxiety, weakness, depression, dizziness, headache, gastrointestinal upset, oral ulcers, edema, bone marrow suppression and rash. Uncommon but potentially severe adverse events include hyperlipidemia, renal dysfunction, severe and opportunistic infections, embryo-fetal toxicity, infertility and hypersensitivity reactions. Sirolimus should be prescribed only by physicians with experience in immunosuppression and management of its complications.
Hepatotoxicity
Serum enzyme elevations occur in a proportion of patients taking sirolimus, but the abnormalities are usually mild, asymptomatic and self-limiting, rarely requiring dose modification or discontinuation. Rare instances of cholestatic hepatitis have been reported with sirolimus use, but the clinical features of the clinically apparent liver injury due to this agent have not been well defined. Most published cases of liver injury attributed to sirolimus occurred in patients exposed to other potentially hepatotoxic agents or who have other underlying possible causes of the abnormalities such as sepsis, cancer or parenteral nutrition. Hepatic artery thrombosis has been reported to be more common with sirolimus therapy after liver transplantation, but this association is still controversial.
Likelihood score: C (probable rare cause of clinically apparent liver injury).
Mechanism of Injury
Sirolimus undergoes extensive hepatic metabolism, largely via the cytochrome P450 system (CYP 3A4) and drug-drug interactions are common. Sirolimus may interfere with wound healing, which has been the usual reason cited for the increased rate of hepatic artery thrombosis with its use.
Outcome and Management
The liver injury associated with sirolimus therapy is usually mild and transient, resolving on its own or with dose modification or discontinuation. Sirolimus has not been linked to cases of acute liver failure or vanishing bile duct syndrome. There does not appear to be cross sensitivity to the hepatic injury between sirolimus and the other agents used for prevention of transplant rejection.
Agents used specifically for the prophylaxis against allograft rejection include cyclosporine, mycophenolate mofetil, sirolimus and tacrolimus, as well as azathioprine and corticosteroids.
Drug Class: Transplant Agents; Antirheumatic Agents, Major Immunosuppressive Agents
Other Drugs in the Class, Transplant Agents: Cyclosporine, Mycophenolate, Tacrolimus
PRODUCT INFORMATION
REPRESENTATIVE TRADE NAMES
Sirolimus – Generic, Rapamune®
DRUG CLASS
Transplant Agents
Product labeling at DailyMed, National Library of Medicine, NIH
CHEMICAL FORMULA AND STRUCTURE
| DRUG | CAS REGISTRY NUMBER | MOLECULAR FORMULA | STRUCTURE |
|---|---|---|---|
| Sirolimus | 53123-88-9 | C51-H79-N-O13 |
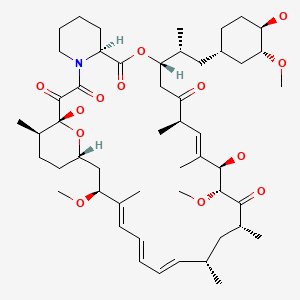
|
ANNOTATED BIBLIOGRAPHY
References updated: 17 February 2020
- Zimmerman HJ. Cyclosporine. Oncotherapeutic and immunosuppressive agents. In, Zimmerman HJ. Hepatotoxicity: the adverse effects of drugs and other chemicals on the liver. 2nd ed. Philadelphia: Lippincott, 1999, pp. 697-8.(Expert review of hepatotoxicity published in 1999; cyclosporine therapy was associated with a high rate of cholestatic liver enzyme elevations ranging from 4-86% and occasional instances of cholestatic hepatitis, some features of which were reproducible in animal models; tacrolimus, sirolimus, and mycophenolate are not discussed).
- Reuben A. Hepatotoxicity of immunosuppressive drugs. In, Kaplowitz N, DeLeve LD, eds. Drug-induced liver disease. 3rd ed. Amsterdam: Elsevier, 2013, pp. 569-92.(Review of hepatotoxicity of immunosuppressive agents mentions that reports of hepatotoxicity of cyclosporine have decreased since the 1980s, perhaps because of monitoring of serum levels and lower doses used; liver injury from tacrolimus, sirolimus and mycophenolate is rare and usually rapidly reversible).
- Krensky AM, Azzi JR, Hafler DA. Immnosuppressants and tolerogens. In, Brunton LL, Hilal-Dandan R, Knollman BC, eds. Goodman & Gilman's the pharmacological basis of therapeutics. 13th ed. New York: McGraw-Hill, 2018, pp. 637-54.(Textbook of pharmacology and therapeutics).
- Kowdley KV, Keeffe EB. Hepatotoxicity of transplant immunosuppressive agents. Gastroenterol Clin North Am. 1995;24:991–1001. [PubMed: 8749908](Review of reports of hepatotoxicity from cyclosporine in form of mild hyperbilirubinemia, mild-to-moderate serum enzyme elevations and biliary sludge and stones).
- Kahan BD. Sirolimus: a comprehensive review. Expert Opin Pharmacother. 2001;2:1903–17. [PubMed: 11825325](Review of chemical structure, pharmacology, mechanism of action, clinical efficacy and safety of sirolimus; most serious adverse effects are hyperlipidemia and myelosuppression; no mention of hepatotoxicity or ALT levels).
- Dunkelberg JC, Trotter JF, Wachs M, Bak T, Kugelmas M, Steinberg T, Everson GT, et al. Sirolimus as primary immunosuppression in liver transplantation is not associated with hepatic artery or wound complications. Liver Transpl. 2003;9:463–8. [PubMed: 12740787](Retrospective analysis of outcome of 170 patients undergoing liver transplantation and treatment with sirolimus found no increase in hepatic artery complications in comparison to historic controls).
- Montalbano M, Neff GW, Yamashiki N, Meyer D, Bettiol M, Slapak-Green G, Ruiz P, et al. A retrospective review of liver transplant patients treated with sirolimus from a single center: an analysis of sirolimus-related complications. Transplantation. 2004;78:264–8. [PubMed: 15280688](Retrospective analysis of complications among 91 liver transplant recipients treated with sirolimus; common side effects were edema, oral ulcers and dermatitis; 12 developed liver test abnormalities that resolved only with stopping drug, and 2 cases of hepatic artery thrombosis).
- Neff GW, Ruiz P, Madariaga JR, Nishida S, Montalbano M, Meyer D, Levi DM, et al. Sirolimus-associated hepatotoxicity in liver transplantation. Ann Pharmacother. 2004;38:1593–6. [PubMed: 15328399](Among 210 liver transplant recipients who received sirolimus, 10 had evidence of hepatotoxicity but 6 had chronic hepatitis C and others rejection as primary or contributing cause).
- Russo MW, Galanko JA, Shrestha R, Fried MW, Watkins P. Liver transplantation for acute liver failure from drug-induced liver injury in the United States. Liver Transpl. 2004;10:1018–23. [PubMed: 15390328](Among ~50,000 liver transplants reported to UNOS between 1990 and 2002, 270 [0.5%] were done for drug induced acute liver failure, 124 for acetaminophen and 137 for other drugs or toxins, but none for agents used to prevent transplant rejection).
- Niemczyk M, Wyzga J, Perkowska A, Porowski D, Paczek L. Sirolimus-associated hepatotoxicity in the kidney graft recipient. Transpl Int. 2005;18:1302–3. [PubMed: 16221163](30 year old man developed persistent ALT elevations 16 months after renal transplant, resolving only when sirolimus was stopped at 24 months).
- Chalasani N, Fontana RJ, Bonkovsky HL, Watkins PB, Davern T, Serrano J, Yang H, Rochon J., Drug Induced Liver Injury Network (DILIN). Causes, clinical features, and outcomes from a prospective study of drug-induced liver injury in the United States. Gastroenterology. 2008;135:1924–34. [PMC free article: PMC3654244] [PubMed: 18955056](Among 300 cases of drug induced liver disease in the US collected between 2004 and 2008, none were attributed to cyclosporine, tacrolimus, sirolimus or mycophenolate).
- Reuben A, Koch DG, Lee WM., Acute Liver Failure Study Group. Drug-induced acute liver failure: results of a U.S. multicenter, prospective study. Hepatology. 2010;52:2065–76. [PMC free article: PMC3992250] [PubMed: 20949552](Among 1198 patients with acute liver failure enrolled in a US prospective study between 1998 and 2007, 133 were attributed to drug induced liver injury, but none to an agent used to prevent transplant rejection).
- Jacques J, Dickson Z, Carrier P, Essig M, Guillaudeau A, Lacour C, Bocquentin F, et al. Severe sirolimus-induced acute hepatitis in a renal transplant recipient. Transpl Int. 2010;23:967–70. [PubMed: 20497403](54 year old man with renal transplant developed jaundice 2 months after switching from cyclosporine to sirolimus [bilirubin 5.4 mg/dL, ALT 609 U/L, GGT 1143 U/L], resolving within 5 weeks of switching back to cyclosporine).
- Czubkowski P, Pawłowska J, Jankowska I, Teisseyre M, Kamińska D, Markiewicz M, Ryżko J. Successful sirolimus rescue in tacrolimus-induced thrombotic microangiopathy after living-related liver transplantation. Pediatr Transplant. 2012;16:E261–4. [PubMed: 22066835](One year old girl with biliary atresia developed tacrolimus induced microangiopathy [hemoglobin 5.6 mg/dL, indirect bilirubin 8.8 mg/dL, ALT 419 U/L, GGT 118 U/L] 8 months after living donor liver transplantation, which resolved after switching to sirolimus).
- Yaich S, El Aoud N, Zaghdane S, Charfeddine K, Kharrat M, Masmoudi M, Hachicha J. Fatal outcome due to sirolimus-induced acute hepatitis, myelosuppression and fever in a kidney allograft recipient. Saudi J Kidney Dis Transpl. 2013;24:580–2. [PubMed: 23640637](33 year old man with a renal transplant developed fever and serum enzyme elevations one month after switching from cyclosporine to sirolimus [bilirubin not given, ALT 85 U/L, Alk P 427 U/L, GGT 180], which improved on switching to tacrolimus but was followed by recurrence of fever, cough and pneumonitis and subsequent multiorgan failure and death).
- Mesar I, Kes P, Hudolin T, Basic-Jukic N. Rescue therapy with sirolimus in a renal transplant recipient with tacrolimus-induced hepatotoxicity. Ren Fail. 2013;35:1434–5. [PubMed: 24028307](54 year old man with end stage renal disease developed evidence liver injury 11 days after transplant and starting tacrolimus, mycophenolate, corticosteroids and basiliximab [bilirubin 0.8 mg/dL, ALT 601 rising to 1242 U/L, GGT 144 to 212], rapidly resolving when he was switched to sirolimus).
- Björnsson ES, Bergmann OM, Björnsson HK, Kvaran RB, Olafsson S. Incidence, presentation and outcomes in patients with drug-induced liver injury in the general population of Iceland. Gastroenterology. 2013;144:1419–25. [PubMed: 23419359](In a population based study of drug induced liver injury from Iceland, 96 cases were identified over a 2 year period, none of which were attributed to an anti-rejection agent used in transplantation).
- Hernández N, Bessone F, Sánchez A, di Pace M, Brahm J, Zapata R, A, Chirino R, et al. Profile of idiosyncratic drug induced liver injury in Latin America: an analysis of published reports. Ann Hepatol. 2014;13:231–9. [PubMed: 24552865](Among 176 reports of drug induced liver injury from Latin America published between 1996 and 2012, one was attributed to mycophenolate but none to cyclosporine, sirolimus or tacrolimus).
- Chalasani N, Bonkovsky HL, Fontana R, Lee W, Stolz A, Talwalkar J, Reddy KR, et al.; United States Drug Induced Liver Injury Network. Features and outcomes of 899 patients with drug-induced liver injury: The DILIN Prospective Study. Gastroenterology 2015; 148: 1340-52. e7. [PMC free article: PMC4446235] [PubMed: 25754159](Among 899 cases of drug induced liver injury enrolled in a US prospective study between 2004 and 2013, one case was attributed to cyclosporine, but none to tacrolimus, sirolimus or mycophenolate mofetil).
- Haliloğlu B, Tüzün H, Flanagan SE, Çelik M, Kaya A, Ellard S, Özbek MN. Sirolimus-induced hepatitis in two patients with hyperinsulinemic hypoglycemia. J Clin Res Pediatr Endocrinol. 2018;10:279–83. [PMC free article: PMC6083472] [PubMed: 29217498](Two infants with congenital hyperinsulinemia and poorly controlled hypoglycemia developed ALT elevations [ALT 302 and 275 U/L, bilirubin and Alk P normal], 2 and 12 months after starting sirolimus which rapidly resolved after stopping sirolimus and rose again on restarting).
- Fiore M, Leone S, Maraolo AE, Berti E, Damiani G. Liver Illness and Psoriatic Patients. Biomed Res Int. 2018;2018:3140983. [PMC free article: PMC5818942] [PubMed: 29546055](Review of liver disease in psoriasis including drug induced liver injury due to methotrexate, acitretin, TNF inhibitors, cyclosporine, and leflunomide).
- PMCPubMed Central citations
- PubChem SubstanceRelated PubChem Substances
- PubMedLinks to PubMed
- Review Tacrolimus.[LiverTox: Clinical and Researc...]Review Tacrolimus.. LiverTox: Clinical and Research Information on Drug-Induced Liver Injury. 2012
- Review Cyclosporine.[LiverTox: Clinical and Researc...]Review Cyclosporine.. LiverTox: Clinical and Research Information on Drug-Induced Liver Injury. 2012
- Review Everolimus.[LiverTox: Clinical and Researc...]Review Everolimus.. LiverTox: Clinical and Research Information on Drug-Induced Liver Injury. 2012
- Review Transplant Agents.[LiverTox: Clinical and Researc...]Review Transplant Agents.. LiverTox: Clinical and Research Information on Drug-Induced Liver Injury. 2012
- Renal function improves in liver transplant recipients when switched from a calcineurin inhibitor to sirolimus.[Liver Transpl. 2003]Renal function improves in liver transplant recipients when switched from a calcineurin inhibitor to sirolimus.Fairbanks KD, Eustace JA, Fine D, Thuluvath PJ. Liver Transpl. 2003 Oct; 9(10):1079-85.
- Sirolimus - LiverToxSirolimus - LiverTox
Your browsing activity is empty.
Activity recording is turned off.
See more...