NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
LiverTox: Clinical and Research Information on Drug-Induced Liver Injury [Internet]. Bethesda (MD): National Institute of Diabetes and Digestive and Kidney Diseases; 2012-.

LiverTox: Clinical and Research Information on Drug-Induced Liver Injury [Internet].
Show detailsOVERVIEW
Introduction
Methylphenidate is a central nervous system stimulant used for the therapy of attention deficit disorder and narcolepsy. Methylphenidate has been linked to a low rate of serum aminotransferase elevations during therapy and to rare instances of acute, clinically apparent liver injury, generally after its intravenous abuse.
Background
Methylphenidate (meth" il fen' i date) is a piperidine derivative that is structurally related to amphetamine which acts as a central nervous system (CNS) sympathomimetic stimulant, probably by causing release of norepinephrine at CNS nerve terminals promoting neurotransmission. Methylphenidate may also affect dopaminergic neurotransmission. Therapy with methylphenidate has been shown to increase cognitive abilities and improve psychological functioning and performance in children and adults with suspected attention deficit disorders. It has a paradoxical calming action in children with hyperactivity. Methylphenidate is also used in the therapy of narcolepsy. Methylphenidate was approved for use in the United States for attention deficit disorder in adults in 1955, and its indications were subsequently broadened to include children above the age of 6 and adolescents with attention deficit disorder. Methylphenidate is available in multiple forms for oral administration including capsules, tablets, oral solutions and as extended release and long acting forms in concentrations varying from 2.5 to 54 mg in generic forms and under several brand names including Ritalin, Concerta, Jornay and Quillvant. A transdermal formulation is also available under the brand name Daytrana. The usual initial dose of standard oral methylphenidate in adults is 10 mg two times daily, and average maintenance dosage is 40 to 60 mg daily in 2 or 3 divided doses. The dosage in children varies by formulation. Methylphenidate is a controlled substance (Schedule II) and has abuse potential. Common side effects include headache, insomnia, irritability, palpitations, tachycardia, nasal stuffiness, decreased appetite, nausea, cough and rash. Uncommon, but potentially severe adverse events include psychotic symptoms, cardiovascular events, abuse and dependence and, with long term therapy in children, reduced adult height.
Hepatotoxicity
In prelicensure clinical trials, methylphenidate was not associated with serum aminotransferase elevations or instances of hepatic injury, but reports of enzyme elevations were received by the sponsor and appeared in publications after it was marketed. The elevations were transient, mild-to-moderate in severity and rarely associated with jaundice or symptoms. In addition, there have been several case reports of marked serum enzyme elevations with jaundice and clinically apparent acute liver injury attributed to methylphenidate given intravenously. These cases occurred largely after illicit intravenous use of methylphenidate and frequently in patients with underlying chronic hepatitis C. The onset was generally soon after initiation of therapy. The pattern of liver enzyme elevations was hepatocellular and the clinical phenotype typical of acute hepatic necrosis with rapid onset and rapid recovery. Immunoallergic features were uncommon. A single case associated with low levels of autoantibodies has been published. Some cases have been severe and at least one fatality after intravenous abuse has been reported. Recurrence upon rechallenge was been documented in one instance (Case 1).
Likelihood score: C[HD] (probable cause of clinically apparent liver injury when given in high doses).
Mechanism of Injury
The mechanism by which methylphenidate might cause liver injury is unknown, but the injury occurring after intravenous use is likely due to direct toxicity. Methylphenidate is extensively metabolized in the liver and has many drug-drug interactions.
Outcome and Management
The liver injury due to oral methylphenidate is usually self-limited and resolves rapidity. Injury from intravenous use can be severe and fatalities have been reported. There have been no instances of chronic liver injury or vanishing bile duct syndrome associated with either oral or intravenous methylphenidate. Cross reactivity with other amphetamine related chemicals has not been demonstrated. However, recurrence of injury with reexposure has been demonstrated.
Central nervous system stimulants used for attention deficit disorder, narcolepsy or excessive sleepiness include methylphenidate, atomoxetine, modafinil, armodafinil and the amphetamines. Stimulants that are no longer used for medical conditions, but that are abused, include cocaine and ecstasy or methylenedioxymethamphetamine. Non-stimulants used for attention deficit disorder include the antihypertensive alpha-2 agonists, clonidine and guanfacine.
Drug Class: CNS Stimulants, Attention Deficit Disorder Agents
Other Drugs for Attention Deficit Disorder: Clonidine, Guanfacine
CASE REPORT
Case 1. Acute hepatic necrosis after intravenous injection of methylphenidate.(1)
A 19 year old woman who had been abusing methylphenidate developed fatigue, fever and jaundice. She admitted to intravenous injection of methylphenidate tablets that had been dissolved in water. She had no history of liver disease or alcohol abuse. She was not taking other medications. On physical examination, she was jaundiced and had an enlarged, slightly tender liver. There were no peripheral manifestations of cirrhosis or chronic liver disease. Laboratory tests showed elevations in serum bilirubin (13 mg/dL) and AST (4,942 U/L), with minimal increase in alkaline phosphatase (100 U/L) (Table). Tests for hepatitis A and B were negative. Tests for hepatitis C were not available at the time of this report. A liver biopsy showed focal necrosis and portal inflammation with lymphocytes, plasma cells and eosinophils, typical of drug induced liver injury. Rechallenge with 4 injections of 20 mg of methylphenidate over two days led to rapid recurrence with a similar pattern of injury.
Key Points
| Medication: | Methylphenidate (by injection) |
|---|---|
| Pattern: | Hepatocellular (R=~100) |
| Severity: | 3+ (jaundice, hospitalization) |
| Latency: | Few days |
| Recovery: | Two weeks |
| Other medications: | None mentioned |
Laboratory Values
| Days After Stopping | AST* (U/L) | Alk P* (U/L) | Bilirubin* (mg/dL) | Comments |
|---|---|---|---|---|
| Intravenous abuse of methylphenidate | ||||
| 3 | 4942 | 100 | 13.0 | Admission for jaundice |
| 5 | 2300 | 14.5 | ||
| 6 | 2090 | 16.0 | Liver Biopsy | |
| 7 | 1900 | 17.0 | ||
| 9 | 1650 | 17.2 | ||
| 11 | 900 | 14.0 | ||
| 14 | 250 | 11.0 | ||
| 16 | 80 | 6.0 | ||
| 18 | 25 | 2.5 | ||
| Rechallenge with four injections of 20 mg of methylphenidate | ||||
| 0 | 15 | 0.5 | Started rechallenge | |
| 0 | 450 | 2.5 | Stopped rechallenge | |
| 1 | 900 | 4.0 | ||
| 2 | 550 | 5.1 | ||
| 3 | 100 | 5.2 | ||
| 5 | 50 | 3.0 | ||
| 7 | 20 | 1.0 | Normal | |
| Normal | <42 | <115 | <1.2 | |
- *
Values estimated from Figure 1.
Comment
Abuse of methylphenidate and intravenous injections of dissolved tablets led to marked jaundice and serum enzyme elevations. Tests for hepatitis C were not available at the time of the report, but intravenous rechallenge led to recurrence with a similar pattern of injury. This degree of severity of liver injury has not been reported with oral methylphenidate which is a widely used medication with excellent tolerance. The pattern of injury associated with intravenous methylphenidate abuse is similar to that described with amphetamine, methylenedioxymethamphetamine and cocaine use, with acute hepatic necrosis (often with other organ damage) arising within 2 to 4 days of the exposure or overdose. Typical of methylphenidate, cocaine and amphetamine hepatotoxicity from intravenous exposure is both the rapidity of the rise and rapidity of the fall in serum aminotransferase levels. LDH levels can be similarly elevated, while alkaline phosphatase values are usually normal or near normal.
PRODUCT INFORMATION
REPRESENTATIVE TRADE NAMES
Methylphenidate – Generic, Concerta®, Daytrana®, Jornay PM®, Ritalin®
DRUG CLASS
Central Nervous System Stimulants
Product labeling at DailyMed, National Library of Medicine, NIH
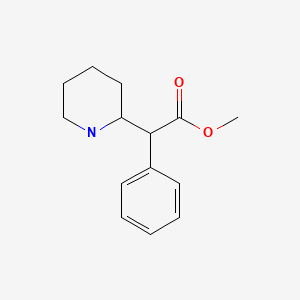
CHEMICAL FORMULA AND STRUCTURE
| DRUG | CAS REGISTRY NUMBER | MOLECULAR FORMULA | STRUCTURE |
|---|---|---|---|
| Methylphenidate | 113-45-1 | C14-H19-N-O2 |
|
CITED REFERENCE
- 1.
- Mehta H, Murray B, LoIudice TA. Hepatic dysfunction due to intravenous abuse of methylphenidate hydrochloride. J Clin Gastroenterol 1984; 6: 149-51. [PubMed: 6715854]
ANNOTATED BIBLIOGRAPHY
References updated: 24 August 2021
Abbreviations: ADHD, attention-deficit/hyperactivity disorder.
- Zimmerman HJ. Methylphenidate. Miscellaneous drugs and diagnostic chemicals. In, Zimmerman, HJ. Hepatotoxicity: the adverse effects of drugs and other chemicals on the liver. 2nd ed. Philadelphia: Lippincott, 1999, pp. 712.(Expert review of hepatotoxicity published in 1999; methylphenidate has been implicated in at least 3 instances of hepatic injury including two with positive rechallenge).
- Larrey D, Ripault MP. Hepatotoxicity of psychotropic drugs and drugs of abuse. In, Kaplowitz N, DeLeve LD, eds. Drug-induced liver disease. 3rd ed. Amsterdam: Elsevier, 2013, pp. 443-62.(Review of hepatotoxicity of antidepressants mentions that methylphenidate has been implicated in hepatocellular injury).
- Westfall TC, Macarthur H, Westfall DP. Methylphenidate. Adrenergic agonists and antagonists. In, Brunton LL, Hilal-Dandan R, Knollman BC, eds. Goodman & Gilman’s the pharmacological basis of therapeutics. 13th ed. New York: McGraw-Hill, 2018, pp. 191-223.(Textbook of pharmacology and therapeutics).
- Goodman CR. Hepatotoxicity due to methylphenidate hydrochloride. N Y State J Med 1972; 72: 2339-40. [PubMed: 4506888](67 year old woman with depression developed mild elevations in ALT [56 U/L] and AST [72 U/L] without symptoms or jaundice 2 weeks after starting methylphenidate, and with rapid resolution on stopping and recurrence after 5 day rechallenge [bilirubin 0.6 mg/dL, ALT 145 U/L, AST 535 U/L, Alk P 18 U/L]).
- Mehta H, Murray B, LoIudice TA. Hepatic dysfunction due to intravenous abuse of methylphenidate hydrochloride. J Clin Gastroenterol 1984; 6: 149-51. [PubMed: 6715854](19 year old woman developed jaundice soon after starting injecting methylphenidate [bilirubin 13.0 mg/dL, AST 4,942 U/L, Alk P 100 U/L], resolving over next few weeks; upon challenge injection of methylphenidate [20 mg] AST rose to ~900 U/L and bilirubin to 5.2 mg/dL in 3-4 days: Case 1).
- Stecyk O, Loludice TA, Demeter S, Jacobs J. Multiple organ failure resulting from intravenous abuse of methylphenidate hydrochloride. Ann Emerg Med 1985; 14: 597-9. [PubMed: 3994088](32 year old woman developed weakness, nausea and dyspnea 2 hours after injecting methylphenidate which she had been doing for ~5 months [bilirubin 1.4 mg/dL, ALT 2,560 U/L, Alk P 174 U/L, lactate 18 mEq/L, arterial pH 7.23, protime 23.7 sec and creatinine 4.0 mg/dL], requiring ICU care, but ultimate recovery over next few weeks).
- Hoover-Stevens S, Kovacevic-Ristanovic R. Management of narcolepsy in pregnancy. Clin Neuropharmacol 2000; 23: 175-81. [PubMed: 11020119](Review of the efficacy of medications for narcolepsy and their safety during pregnancy and breast feeding; there have been no studies on the safety of methylphenidate in pregnancy).
- Leonard BE, McCartan D, White J, King DJ. Methylphenidate: a review of its neuropharmacological, neuropsychological and adverse clinical effects. Hum Psychopharmacol 2004; 19: 151-80. [PubMed: 15079851](Review of mechanism of action, clinical efficacy and safety of methylphenidate; no mention of hepatotoxicity or serum ALT elevations).
- Lewis JJ, Iezzoni JC, Berg CL. Methylphenidate-induced autoimmune hepatitis. Dig Dis Sci 2007; 52: 594-7. [PubMed: 17219064](57 year old man developed marked enzyme elevations 4 years after liver transplantation for hepatitis C and 1 month after starting methylphenidate [bilirubin 2.7 rising to 4.1 mg/dL, ALT 338 U/L, ANA 1:80, IgG 1950 mg/dL], improving upon stopping methylphenidate and falling to baseline on prednisone therapy).
- Chalasani N, Fontana RJ, Bonkovsky HL, Watkins PB, Davern T, Serrano J, Yang H, Rochon J; Drug Induced Liver Injury Network (DILIN). Causes, clinical features, and outcomes from a prospective study of drug-induced liver injury in the United States. Gastroenterology 2008; 135: 1924-34. [PMC free article: PMC3654244] [PubMed: 18955056](Among 300 cases of drug induced liver disease in the US collected between 2004 and 2008, 3 cases were attributed to atomoxetine and one to methylphenidate, but none to cocaine or ecstasy).
- Ferrajolo C, Capuano A, Verhamme KM, Schuemie M, Rossi F, Stricker BH, Sturkenboom MC. Drug-induced hepatic injury in children: a case/non-case study of suspected adverse drug reactions in VigiBase. Br J Clin Pharmacol 2010; 70: 721-8. [PMC free article: PMC2997312] [PubMed: 21039766](Worldwide pharmacovigilance database contained 9036 hepatic adverse drug reactions in children, 2 agents used for attention deficit disorder were among the top 40 causes; methylphenidate [11th, 96 cases] and atomoxetine [14th, 64 cases]).
- Devarbhavi H, Dierkhising R, Kremers WK, Sandeep MS, Karanth D, Adarsh CK. Single-center experience with drug-induced liver injury from India: causes, outcome, prognosis, and predictors of mortality. Am J Gastroenterol 2010; 105: 2396-404. [PubMed: 20648003](Among 313 cases of drug induced liver injury seen between 1997 and 2008 at a large hospital in Bangalore, India, one case was attributed to atomoxetine, none to methylphenidate).
- Reuben A, Koch DG, Lee WM; Acute Liver Failure Study Group. Drug-induced acute liver failure: results of a U.S. multicenter, prospective study. Hepatology 2010; 52: 2065-76. [PMC free article: PMC3992250] [PubMed: 20949552](Among 1198 patients with acute liver failure enrolled in a US prospective study between 1998 and 2007, 133 were attributed to drug induced liver injury, including one attributed to cocaine and one to ecstasy but none to methylphenidate).
- Molleston JP, Fontana RJ, Lopez MJ, Kleiner DE, Gu J, Chalasani N: Drug-induced Liver Injury Network. Characteristics of idiosyncratic drug-induced liver injury in children: results from the DILIN prospective study. J Pediatr Gastroenterol Nutr 2011; 53: 182-9. [PMC free article: PMC3634369] [PubMed: 21788760](Among 30 children with suspected drug induced liver injury, 3 were attributed to atomoxetine and one to methylphenidate).
- Cantrell FL, Ogera P, Mallett P, McIntyre IM. Fatal oral methylphenidate intoxication with postmortem concentrations. J Forensic Sci 2014; 59: 847-9. [PubMed: 24502813](62 year old woman with chronic hepatitis C was found dead at home and autopsy showed high levels of methylphenidate consistent with drug overdose; liver histology showed chronic hepatitis and mild fatty change and no evidence of acute liver injury).
- Björnsson ES, Bergmann OM, Björnsson HK, Kvaran RB, Olafsson S. Incidence, presentation and outcomes in patients with drug-induced liver injury in the general population of Iceland. Gastroenterology 2013; 144: 1419-25. [PubMed: 23419359](In a population based study of drug induced liver injury from Iceland, 96 cases were identified over a 2 year period, none of which were attributed to methylphenidate).
- Hernández N, Bessone F, Sánchez A, di Pace M, Brahm J, Zapata R, A Chirino R, et al. Profile of idiosyncratic drug induced liver injury in Latin America: an analysis of published reports. Ann Hepatol 2014; 13: 231-9. [PubMed: 24552865](Among 176 reports of drug induced liver injury from Latin America published between 1996 and 2012, none of which were attributed methylphenidate).
- Chalasani N, Bonkovsky HL, Fontana R, Lee W, Stolz A, Talwalkar J, Reddy KR, et al.; United States Drug Induced Liver Injury Network. Features and outcomes of 899 patients with drug-induced liver injury: The DILIN Prospective Study. Gastroenterology 2015; 148: 1340-52.e7. [PMC free article: PMC4446235] [PubMed: 25754159](Among 899 cases of drug induced liver injury enrolled in a US prospective study between 2004 and 2013, 12 [1.3%] were attributed to drugs used in transplant rejection, including 10 to azathioprine and 1 to tacrolimus, but none to mycophenolate).
- Newcorn JH, Nagy P, Childress AC, Frick G, Yan B, Pliszka S. Randomized, double-blind, placebo-controlled acute comparator trials of lisdexamfetamine and extended-release methylphenidate in adolescents with attention-deficit/hyperactivity disorder. CNS Drugs 2017; 31: 999-1014. [PMC free article: PMC5730627] [PubMed: 28980198](Among 1013 adolescents with attention deficit/hyperactivity disorder treated with methylphenidate or lisdexamfetamine or placebo for 6 or 8 weeks, both drugs improved symptoms more than placebo but both had higher and similar rates of adverse events; no mention of ALT elevations or hepatoxicity or discontinuations for hepatic adverse events).
- Edvinsson D, Ekselius L. Long-term tolerability and safety of pharmacological treatment of adult attention-deficit/hyperactivity disorder: a 6-year prospective naturalistic study. J Clin Psychopharmacol 2018; 38: 370-5. [PMC free article: PMC6039396] [PubMed: 29927781](Among 112 adults with attention deficit disorder started on methylphenidate and followed for up to 6 years, half had discontinued treatment but no mention is made of ALT elevations, hepatotoxicity or drug discontinuations because of hepatic adverse events).
- Cortese S, Adamo N, Mohr-Jensen C, Hayes AJ, Bhatti S, Carucci S, Del Giovane C, et al.; European ADHD Guidelines Group (EAGG). Comparative efficacy and tolerability of pharmacological interventions for attention-deficit/hyperactivity disorder in children, adolescents and adults: protocol for a systematic review and network meta-analysis. BMJ Open 2017; 7(1): e013967. [PMC free article: PMC5253538] [PubMed: 28073796](Review of the pharmacological therapy of ADHD with discussion of amphetamines, methylphenidate, atomoxetine, guanfacine and clonidine; no mention of ALT elevations during therapy or hepatotoxicity).
- Fekete S, Romanos M, Gerlach M. [Does methylphenidate cause liver damage? An analysis of ad hoc reports to the "Bundesinstitut für Arzneimittel und Medizinprodukte (BfArM)"]. Z Kinder Jugendpsychiatr Psychother 2018; 46: 342-8. German. [PubMed: 29237323](Analysis of cases of suspected methylphenidate liver injury reported to the German Federal Institute for Drugs and Medical Devices between 2006 and 2016 identified 60 cases, but most were unlikely or incomplete, only 11 were considered possible and 9 probable, most marked by serum enzyme elevations without jaundice but one with acute liver failure).
- Schoretsanitis G, de Leon J, Eap CB, Kane JM, Paulzen M. Clinically significant drug-drug interactions with agents for attention-deficit/hyperactivity disorder. CNS Drugs. 2019; 33: 1201-22. [PubMed: 31776871](Review of drug-drug interactions of agents used to treat ADHD mentions that there is little information on the metabolism of clonidine and possible drug-drug interactions).
- Joshi G, DiSalvo M, Wozniak J, Ceranoglu TA, Yule A, Surman C, Fried R, et al. A prospective open-label trial of long-acting liquid methylphenidate for the treatment of attention deficit/hyperactivity disorder in intellectually capable adults with autism spectrum disorder. World J Biol Psychiatry 2020; 21(4): 274-90. [PubMed: 31607204](Among 15 adults with attention deficit disorder treated with long acting methylphenidate, adverse events were frequent including headache [53%], insomnia [33%], anxiety [33%], and decreased appetite [27%]; no mention of ALT elevations or hepatotoxicity).
- Drugs for ADHD. Med Lett Drugs Ther 2020; 62(1590): 9-15. [PubMed: 31999670](Concise review of drugs for attention deficit/hyperactivity disorder mentions that methylphenidate and the CNS stimulants are the first line agents for school age children and adolescents and that adverse events can include decreased appetite, abdominal pain, headache and insomnia, but does not mention ALT elevations or hepatotoxicity).
- Kis B, Lücke C, Abdel-Hamid M, Heßmann P, Graf E, Berger M, Matthies S, et al. Safety profile of methylphenidate under long-term treatment in adult ADHD patients – results of the COMPAS Study. Pharmacopsychiatry 2020; 53: 263-71. [PubMed: 33017854](Among 433 adults with ADHD treated with methylphenidate or placebo combined with cognitive behavioral group psychotherapy, adverse events that were common with methylphenidate included decrease in appetite [22% vs 4%], dry mouth [15% vs 5%], palpitations [11% vs 3%], agitation [11% vs 3%], restlessness [6% vs 2%], sweating and tachycardia, while liver enzyme elevations were rare [0.5% vs none]).
- Weiss MD, Childress AC, Donnelly GAE. Efficacy and safety of PRC-063, extended-release multilayer methylphenidate in adults with ADHD including 6-month open-label extension. J Atten Disord 2021: 25(10): 1417-28. [PMC free article: PMC8273537] [PubMed: 31916473](Among 375 adults with attention deficit/hyperactivity disorder treated with 1 of 4 doses of extended release methylphenidate or placebo once daily for 6 months, adverse events included headache, insomnia, decreased appetite, dry mouth, and nausea, and there were “no clinically significant changes from baseline in laboratory findings”).
- Huang YS, Yeh CB, Chen CH, Shang CY, Gau SS. A randomized, double-blind, placebo-controlled, two-way crossover clinical trial of ORADUR-methylphenidate for treating children and adolescents with attention-deficit/hyperactivity disorder. J Child Adolesc Psychopharmacol 2021; 31: 164-78. [PMC free article: PMC8066345] [PubMed: 33395356](Among 100 children and adolescents with ADHD treated in a 2 week cross over study of extended release methylphenidate vs placebo, ADHD symptoms improved with methylphenidate and “there were no significant changes in laboratory safety profiles”).
- Childress A, Cutler AJ, Marraffino AH, Bhaskar S, Donnelly G. Randomized, double-blind, placebo-controlled, parallel-group, adult laboratory classroom study of the efficacy and safety of PRC-063 (extended-release methylphenidate) for the treatment of ADHD. J Atten Disord. 2022;26(6):857-869. [PMC free article: PMC8859679] [PubMed: 34189995](Among 288 adults with ADHD treated with once daily extended release methylphenidate with dose optimization over 7 weeks, classroom performance improved with therapy and adverse events included headache, decreased appetite, and insomnia but “there were no clinically meaningful changes in mean values for clinical chemistry” results).
- PMCPubMed Central citations
- PubChem SubstanceRelated PubChem Substances
- PubMedLinks to PubMed
- Review Misuse of Methylphenidate.[Curr Top Behav Neurosci. 2017]Review Misuse of Methylphenidate.Clemow DB. Curr Top Behav Neurosci. 2017; 34:99-124.
- Lacunar stroke associated with methylphenidate abuse.[Can J Neurol Sci. 2004]Lacunar stroke associated with methylphenidate abuse.Sadeghian H. Can J Neurol Sci. 2004 Feb; 31(1):109-11.
- Characteristics and outcomes of cases with methylphenidate abuse, dependence or withdrawal: an analysis of spontaneous reports in EudraVigilance.[Int Clin Psychopharmacol. 2023]Characteristics and outcomes of cases with methylphenidate abuse, dependence or withdrawal: an analysis of spontaneous reports in EudraVigilance.Hartmayer LT, Hoffmann F, Bachmann CJ, Jobski K. Int Clin Psychopharmacol. 2023 May 1; 38(3):169-178. Epub 2023 Jan 4.
- Review Methylphenidate: its pharmacology and uses.[Mayo Clin Proc. 2000]Review Methylphenidate: its pharmacology and uses.Challman TD, Lipsky JJ. Mayo Clin Proc. 2000 Jul; 75(7):711-21.
- Review Atomoxetine: a review of its use in attention-deficit hyperactivity disorder in children and adolescents.[Paediatr Drugs. 2009]Review Atomoxetine: a review of its use in attention-deficit hyperactivity disorder in children and adolescents.Garnock-Jones KP, Keating GM. Paediatr Drugs. 2009; 11(3):203-26.
- Methylphenidate - LiverToxMethylphenidate - LiverTox
Your browsing activity is empty.
Activity recording is turned off.
See more...