30. Pharmacist support
30.1. Introduction
Increasing numbers of patients with multiple co-morbidities are being exposed to large numbers of medications designed to treat each of the conditions from which they may suffer. This, however, is associated with increasing numbers of drug interactions, difficulties with concordance and possible admissions or readmissions associated with drug errors or adverse effects. The introduction of clinical pharmacists has been designed to minimise these difficulties and, in particular, medicines reconciliation has been conducted for many patients to ensure clarity of the drugs prescribed and taken. The presence of a ward based pharmacist is common practice in the UK. However, the precise input required from pharmacy support is still not clear and this question is posed in an attempt to understand the best way in which pharmacy support is used.
30.2. Review question: Do ward-based pharmacists improve outcomes in patients admitted to hospital with a suspected or confirmed acute medical emergency?
For full details see review protocol in Appendix A.
Table 1
PICO characteristics of review question.
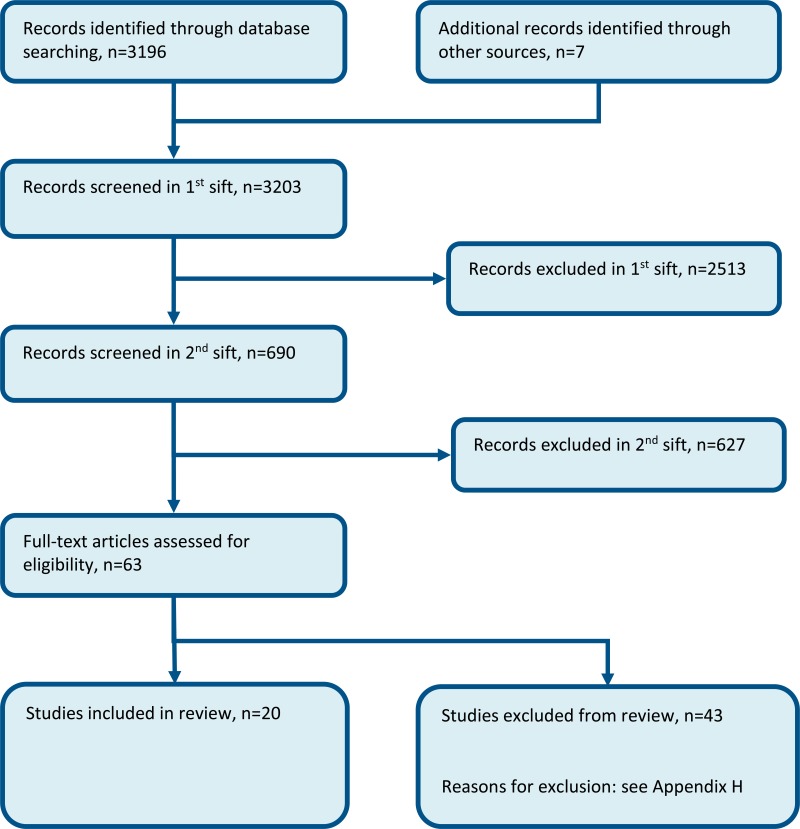
30.3. Clinical evidence
Eighteen studies (20 papers) were included in the review;1,3,8,13,15,17,18,21,31,35,37,39,44,46,57–59,62,69,69,70,70 these were split into 3 strata: regular in-hospital pharmacy support (where the ward-based pharmacist intervention included in-patient monitoring, and typically an admission and discharge service), pharmacist at admission, and pharmacist at discharge. These are summarised respectively in Table 2, Table 3 and Table 4 below. Evidence from these studies is summarised in the clinical evidence summary below (Table 5 to Table 7). See also the study selection flow chart in Appendix B, study evidence tables in Appendix D, forest plots in Appendix C, GRADE tables in Appendix F and excluded studies list in Appendix G.
Table 2
Summary of studies included in the review (regular in-hospital pharmacy support).
Table 3
Summary of studies included in the review (pharmacist at admission).
Table 4
Summary of studies included in the review (pharmacist at discharge).
Table 5
Clinical evidence summary: Regular in-hospital ward based pharmacy support compared to no ward-based pharmacist.
Table 7
Clinical evidence summary: Pharmacist at discharge compared to no ward-based pharmacist.
Outcomes as reported in studies (not analysable):
- Length of stay: intervention group had on average a 0.3-day shorter stay.
- Readmission: intervention group had a 44% reduced readmission rate.
Table 6
Clinical evidence summary: Pharmacist at admission compared to no ward-based pharmacist.
Outcomes reported that were not analysable
The study by Khalil 201631 reported the total number of medication errors:
- Intervention: 29/56.
- Control: 238/54.
30.4. Economic evidence
Published literature
Seven economic evaluations were identified with the relevant comparison and have been included in this review.13,19–21,29,32,66 Similar to the clinical evidence, these were split into 3 strata: regular ward-based pharmacist support (where the ward-based pharmacist intervention included in-patient monitoring, and typically an admission and discharge service) (n=5), pharmacist at admission (n=1), and pharmacist at discharge (n=1). The studies are summarised in the economic evidence profiles below (Table 8, Table 9 and Table 10) and the economic evidence tables in Appendix F.
Table 8
Economic evidence profile: regular ward-based pharmacist support versus no ward-based pharmacist.
Table 9
Economic evidence profile: Pharmacist support at admission versus no ward-based pharmacist.
Table 10
Economic evidence profile: Pharmacist support at discharge versus no ward-based pharmacist.
The economic article selection protocol and flow chart for the whole guideline can found in Appendix 41A and Appendix 41B.
30.5. Evidence statements
Clinical
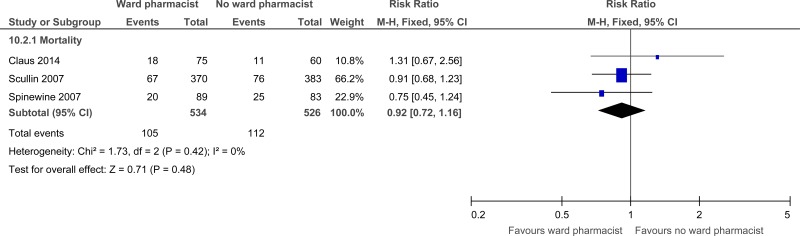
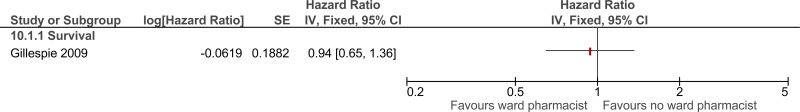
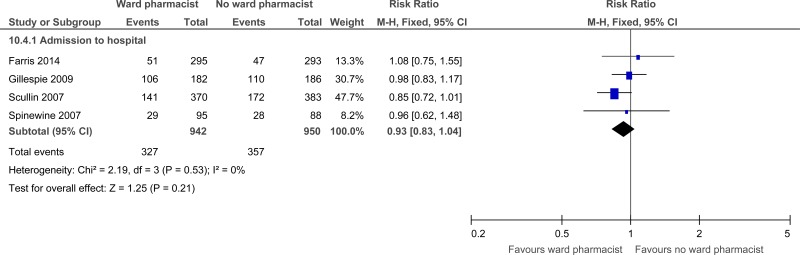
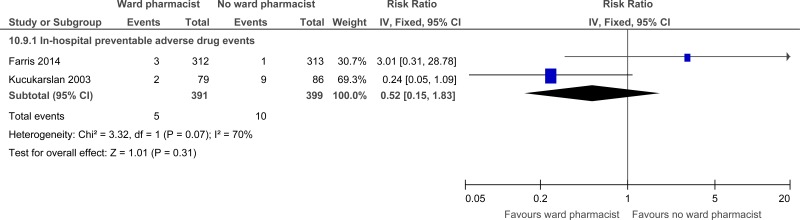
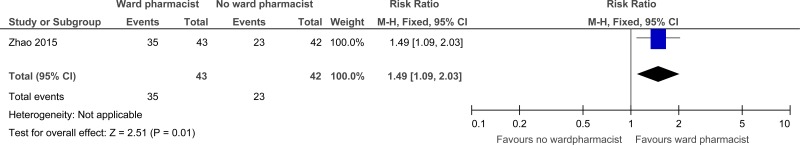
Stratum - Regular in-hospital ward based pharmacy support
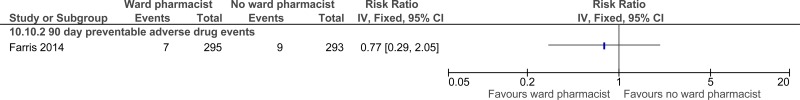
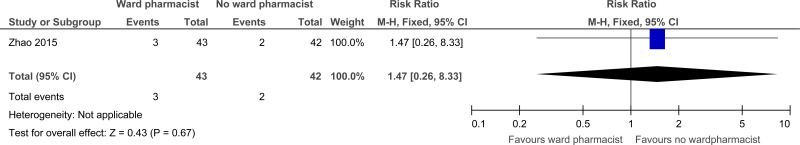
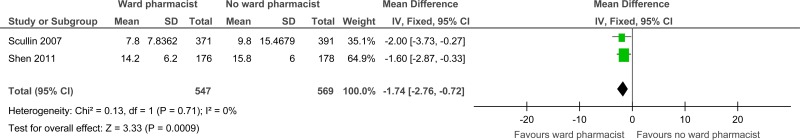
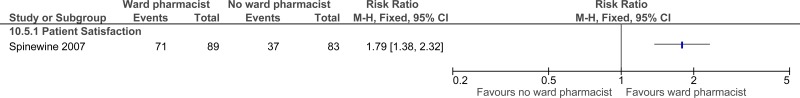
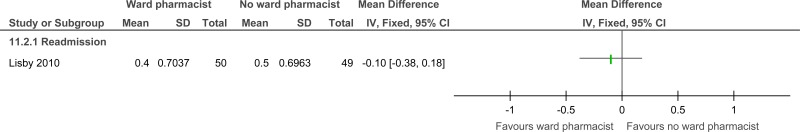
Eight randomised controlled trials comprising 2,303 people evaluated the role of regular in-hospital pharmacist support for improving outcomes in secondary care, in adults and young people at risk of an AME, or with a suspected or confirmed AME. The evidence suggested that regular in-hospital pharmacist support may provide a benefit for reduced mortality (3 studies, very low quality), reduced preventable adverse drug events in hospital (2 studies, very low quality) and at 90 days follow up (1 study, very low quality) and length of stay (2 studies, moderate quality) and increased patient and/or carer satisfaction at discharge and at one month follow-up (1 study, low quality). The evidence suggested that regular in-hospital pharmacist support has no effect on readmission (1 study, very low quality), adverse drug events at 3 to 6 months post discharge (1 study, very low quality) and admission (4 studies, moderate quality). Evidence suggested no difference between the groups for the outcome of reducing prescribing errors at discharge (2 studies, low quality) ; however there were increased prescribing errors at 30 days in regular in-hospital pharmacist support group compared to no pharmacist support group (1 study quality, moderate quality).
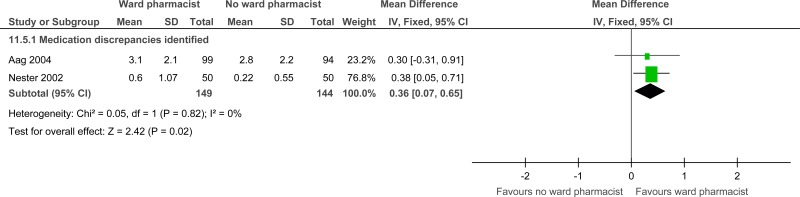
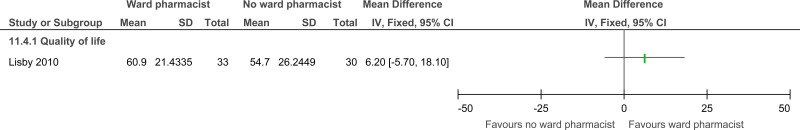
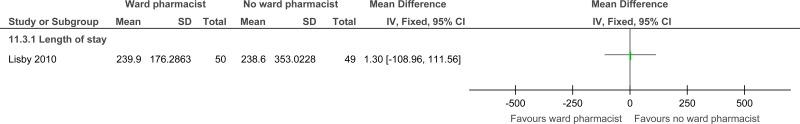
Stratum - Pharmacist at admission
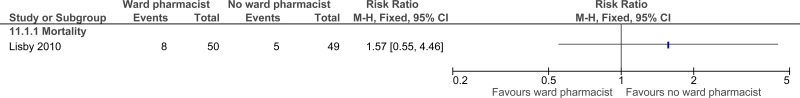
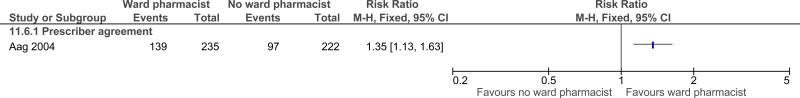
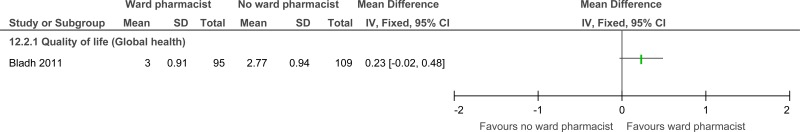
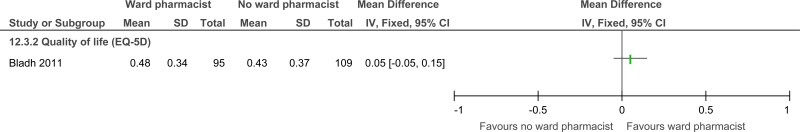
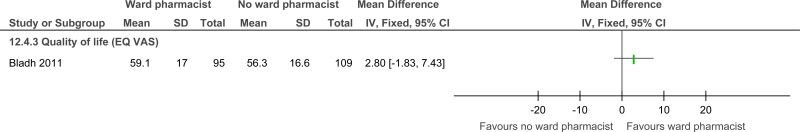
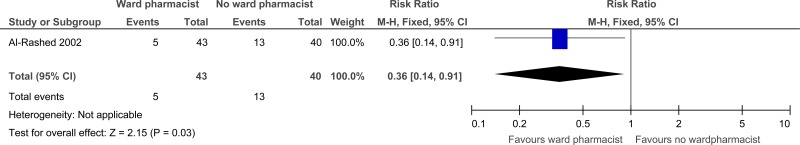
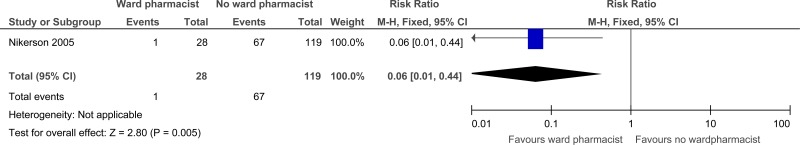
- Six randomised controlled trials comprising 401 people evaluated the role of pharmacists at admission for improving outcomes in secondary care, in adults and young people at risk of an AME, or with a suspected or confirmed AME. The evidence suggested that pharmacists at admission may provide benefit for reduced medicine errors (2 studies, low quality), total medication errors within 24 hours of admission (1 study, moderate quality) and physician agreement (1 study, very low quality). However, there was no difference for quality of life (1 study, low quality), length of stay (1 study, moderate quality), or future hospital admissions (1 study, low quality) and a possible increase in mortality at 3 months (1 study, very low quality).
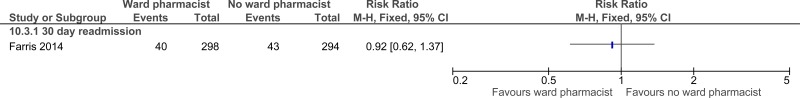
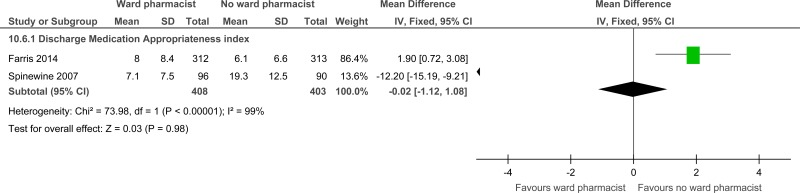
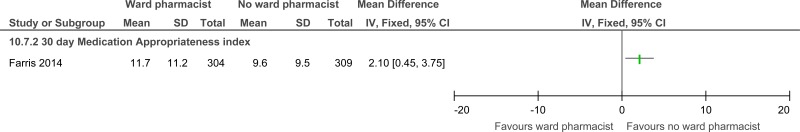
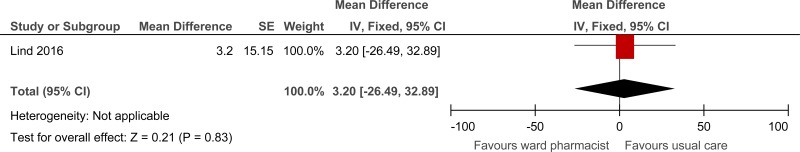
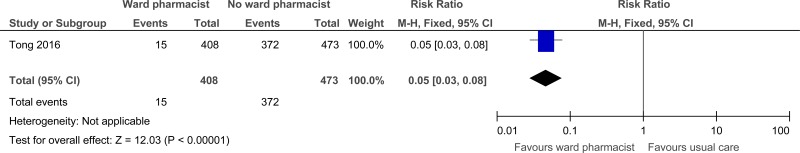
Stratum - Pharmacist at discharge
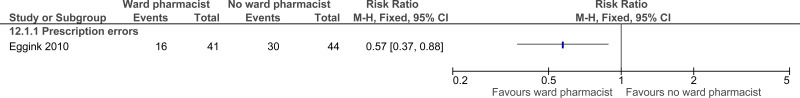
- Four randomised controlled trials comprising 770 people evaluated the role of pharmacists at discharge for improving outcomes in secondary care, in adults and young people at risk of an AME, or with a suspected or confirmed AME. The evidence suggested that pharmacists at discharge may provide a benefit for reduced prescription errors (1 study, low quality), reduced readmissions up to 22 days post discharge (1 study, very low quality) and reducing prescriber errors (drug therapy inconsistencies and omissions) at discharge (1 study, moderate quality). The evidence suggested that pharmacists at discharge have no effect on quality of life scales (1 study, very low to low quality).
Economic
Stratum - Regular ward-based pharmacist support
- Three economic evaluations reported that the ward-based pharmacist intervention was dominant (more effective and less costly) compared to usual care. One of these economic evaluations was a cost-utility analysis reporting a QALY gain of 0.005. These analyses were assessed as partially applicable with potentially serious limitations.
- One cost-utility analysis showed that the ward-based pharmacist intervention was cost-effective with an ICER of £632 per QALY gained (as calculated by the NGC). The analysis was assessed as partially applicable with potentially serious limitations.
- One economic evaluation showed that regular ward-based pharmacist support was less effective and less costly, with no clear conclusion regarding cost effectiveness given the absence of a cost-effectiveness threshold for the reported outcomes. The analysis was assessed as partially applicable with potentially serious limitations.
Stratum – pharmacist at admission
- One comparative cost analysis showed that pharmacist support at admission was cost saving compared to usual care. The analysis was assessed as partially applicable with potentially serious limitations.
Stratum – pharmacist at discharge
- One cost-utility analysis showed that the ward-based pharmacist support at discharge was not cost effective, with an ICER of £327,378 per adjusted QALY gained. The analysis was assessed as partially applicable with minor limitations.
30.6. Recommendations and link to evidence
References
- 1.
- Aag T, Garcia BH, Viktil KK. Should nurses or clinical pharmacists perform medication reconciliation? A randomized controlled trial. European Journal of Clinical Pharmacology. 2014; 70(11):1325–1332 [PubMed: 25187339]
- 2.
- Abu-Oliem AS, Al-Sharayri MG, AlJabra RJ, Hakuz NM. A clinical trial to investigate the role of clinical pharmacist in resolving/preventing drug related problems in ICU patients who receive anti-infective therapy. Jordan Journal of Pharmaceutical Sciences. 2013; 6(3):292–298
- 3.
- Al-Rashed SA, Wright DJ, Roebuck N, Sunter W, Chrystyn H. The value of inpatient pharmaceutical counselling to elderly patients prior to discharge. British Journal of Clinical Pharmacology. 2002; 54(6):657–664 [PMC free article: PMC1874498] [PubMed: 12492615]
- 4.
- Alassaad A, Bertilsson M, Gillespie U, Sundstrom J, Hammarlund-Udenaes M, Melhus H. The effects of pharmacist intervention on emergency department visits in patients 80 years and older: subgroup analyses by number of prescribed drugs and appropriate prescribing. PloS One. 2014; 9(11):e111797 [PMC free article: PMC4218816] [PubMed: 25364817]
- 5.
- Basger BJ, Moles RJ, Chen TF. Impact of an enhanced pharmacy discharge service on prescribing appropriateness criteria: a randomised controlled trial. International Journal of Clinical Pharmacy. 2015; 37(6):1194–1205 [PubMed: 26297239]
- 6.
- Bates DW, Spell N, Cullen DJ, Burdick E, Laird N, Petersen LA et al. The costs of adverse drug events in hospitalized patients. Adverse Drug Events Prevention Study Group. JAMA - Journal of the American Medical Association. 1997; 277(4):307–311 [PubMed: 9002493]
- 7.
- Bessesen MT, Ma A, Clegg D, Fugit RV, Pepe A, Goetz MB et al. Antimicrobial stewardship programs: comparison of a program with infectious diseases pharmacist support to a program with a geographic pharmacist staffing model. Hospital Pharmacy. 2015; 50(6):477–483 [PMC free article: PMC4568108] [PubMed: 26405339]
- 8.
- Bladh L, Ottosson E, Karlsson J, Klintberg L, Wallerstedt SM. Effects of a clinical pharmacist service on health-related quality of life and prescribing of drugs: a randomised controlled trial. BMJ Quality & Safety. 2011; 20(9):738–746 [PubMed: 21209140]
- 9.
- Bolas H, Brookes K, Scott M, McElnay J. Evaluation of a hospital-based community liaison pharmacy service in Northern Ireland. Pharmacy World and Science. 2004; 26(2):114–120 [PubMed: 15085948]
- 10.
- Burnett KM, Scott MG, Fleming GF, Clark CM, McElnay JC. Effects of an integrated medicines management program on medication appropriateness in hospitalized patients. American Journal of Health-System Pharmacy. 2009; 66(9):854–859 [PubMed: 19386949]
- 11.
- Cani CG, Lopes LdSG, Queiroz M, Nery M. Improvement in medication adherence and self-management of diabetes with a clinical pharmacy program: a randomized controlled trial in patients with type 2 diabetes undergoing insulin therapy at a teaching hospital. Clinics. 2015; 70(2):102–106 [PMC free article: PMC4351311] [PubMed: 25789518]
- 12.
- Chen J-H, Ou H-T, Lin T-C, Lai ECC, Yang KYH. Pharmaceutical care of elderly patients with poorly controlled type 2 diabetes mellitus: a randomized controlled trial. International Journal of Clinical Pharmacy. 2016; 38(1):88–95 [PubMed: 26499503]
- 13.
- Claus BOM, Robays H, Decruyenaere J, Annemans L. Expected net benefit of clinical pharmacy in intensive care medicine: a randomized interventional comparative trial with matched before-and-after groups. Journal of Evaluation in Clinical Practice. 2014; 20(6):1172–1179 [PubMed: 25470782]
- 14.
- de Boer M, Ramrattan MA, Kiewiet JJS, Boeker EB, Gombert-Handoko KB, van Lent-Evers NAEM et al. Cost-effectiveness of ward-based pharmacy care in surgical patients: protocol of the SUREPILL (Surgery & Pharmacy In Liaison) study. BMC Health Services Research. 2011; 11:55 [PMC free article: PMC3059300] [PubMed: 21385352]
- 15.
- Eggink RN, Lenderink AW, Widdershoven JWMG, van den Bemt PMLA. The effect of a clinical pharmacist discharge service on medication discrepancies in patients with heart failure. Pharmacy World and Science. 2010; 32(6):759–766 [PMC free article: PMC2993887] [PubMed: 20809276]
- 16.
- Engelhardt JB, McClive-Reed KP, Toseland RW, Smith TL, Larson DG, Tobin DR. Effects of a program for coordinated care of advanced illness on patients, surrogates, and healthcare costs: a randomized trial. American Journal of Managed Care. 2006; 12(2):93–100 [PubMed: 16464138]
- 17.
- Farley TM, Shelsky C, Powell S, Farris KB, Carter BL. Effect of clinical pharmacist intervention on medication discrepancies following hospital discharge. International Journal of Clinical Pharmacy. 2014; 36(2):430–437 [PMC free article: PMC4026363] [PubMed: 24515550]
- 18.
- Farris KB, Carter BL, Xu Y, Dawson JD, Shelsky C, Weetman DB et al. Effect of a care transition intervention by pharmacists: an RCT. BMC Health Services Research. 2014; 14:406 [PMC free article: PMC4262237] [PubMed: 25234932]
- 19.
- Fertleman M, Barnett N, Patel T. Improving medication management for patients: the effect of a pharmacist on post-admission ward rounds. Quality and Safety in Health Care. 2005; 14(3):207–211 [PMC free article: PMC1744029] [PubMed: 15933319]
- 20.
- Ghatnekar O, Bondesson A, Persson U, Eriksson T. Health economic evaluation of the Lund Integrated Medicines Management Model (LIMM) in elderly patients admitted to hospital. BMJ Open. Sweden 2013; 3(1):e001563 [PMC free article: PMC3553390] [PubMed: 23315436]
- 21.
- Gillespie U, Alassaad A, Henrohn D, Garmo H, Hammarlund-Udenaes M, Toss H et al. A comprehensive pharmacist intervention to reduce morbidity in patients 80 years or older: a randomized controlled trial. Archives of Internal Medicine. 2009; 169(9):894–900 [PubMed: 19433702]
- 22.
- Graabaek T, Kjeldsen LJ. Medication reviews by clinical pharmacists at hospitals lead to improved patient outcomes: a systematic review. Basic and Clinical Pharmacology and Toxicology. 2013; 112(6):359–373 [PubMed: 23506448]
- 23.
- Heselmans A, van Krieken J, Cootjans S, Nagels K, Filliers D, Dillen K et al. Medication review by a clinical pharmacist at the transfer point from ICU to ward: a randomized controlled trial. Journal of Clinical Pharmacy and Therapeutics. 2015; 40(5):578–583 [PubMed: 29188903]
- 24.
- Hodgkinson B, Koch S, Nay R, Nichols K. Strategies to reduce medication errors with reference to older adults. International Journal of Evidence-Based Healthcare. 2006; 4(1):2–41 [PubMed: 21631752]
- 25.
- Horn E, Jacobi J. The critical care clinical pharmacist: evolution of an essential team member. Critical Care Medicine. 2006; 34:(Suppl 3):S46–S51 [PubMed: 16477202]
- 26.
- Israel EN, Farley TM, Farris KB, Carter BL. Underutilization of cardiovascular medications: effect of a continuity-of-care program. American Journal of Health-System Pharmacy. 2013; 70(18):1592–1600 [PMC free article: PMC4019344] [PubMed: 23988600]
- 27.
- Jarab AS, Alqudah SG, Khdour M, Shamssain M, Mukattash TL. Impact of pharmaceutical care on health outcomes in patients with COPD. International Journal of Clinical Pharmacy. 2012; 34(1):53–62 [PubMed: 22101426]
- 28.
- Kaboli PJ, Hoth AB, McClimon BJ, Schnipper JL. Clinical pharmacists and inpatient medical care: a systematic review. Archives of Internal Medicine. 2006; 166(9):955–964 [PubMed: 16682568]
- 29.
- Karnon J, McIntosh A, Dean J, Bath P, Hutchinson A, Oakley J et al. Modelling the expected net benefits of interventions to reduce the burden of medication errors. Journal of Health Services Research and Policy. United Kingdom 2008; 13(2):85–91 [PubMed: 18416913]
- 30.
- Karnon J, McIntosh A, Bath P, Hutchinson A, Oakley J, Freeman-Parry L et al. A prospective hazard and improvement analysis of medication errors in a UK secondary care setting, 2007. Available from: http://www
.birmingham .ac.uk/Documents/college-mds /haps/projects /cfhep/psrp/finalreports /PS018FinalReportKarnon.pdf - 31.
- Khalil V, deClifford JM, Lam S, Subramaniam A. Implementation and evaluation of a collaborative clinical pharmacist’s medications reconciliation and charting service for admitted medical inpatients in a metropolitan hospital. Journal of Clinical Pharmacy and Therapeutics. 2016; 41(6):662–666 [PubMed: 27578624]
- 32.
- Klopotowska JE, Kuiper R, vanKan HJ, dePont AC, Dijkgraaf MG, Lie AH et al. On-ward participation of a hospital pharmacist in a Dutch intensive care unit reduces prescribing errors and related patient harm: an intervention study. Critical Care. Netherlands 2010; 14(5):R174 [PMC free article: PMC3219276] [PubMed: 20920322]
- 33.
- Koehler BE, Richter KM, Youngblood L, Cohen BA, Prengler ID, Cheng D et al. Reduction of 30-day postdischarge hospital readmission or emergency department (ED) visit rates in high-risk elderly medical patients through delivery of a targeted care bundle. Journal of Hospital Medicine. 2009; 4(4):211–218 [PubMed: 19388074]
- 34.
- Kucukarslan SN, Corpus K, Mehta N, Mlynarek M, Peters M, Stagner L et al. Evaluation of a dedicated pharmacist staffing model in the medical intensive care unit. Hospital Pharmacy. 2013; 48(11):922–930 [PMC free article: PMC3875111] [PubMed: 24474833]
- 35.
- Kucukarslan SN, Peters M, Mlynarek M, Nafziger DA. Pharmacists on rounding teams reduce preventable adverse drug events in hospital general medicine units. Archives of Internal Medicine. 2003; 163(17):2014–2018 [PubMed: 14504113]
- 36.
- Leape LL, Cullen DJ, Clapp MD, Burdick E, Demonaco HJ, Erickson JI et al. Pharmacist participation on physician rounds and adverse drug events in the intensive care unit. JAMA - Journal of the American Medical Association. 1999; 282(3):267–270 [PubMed: 10422996]
- 37.
- Lind KB, Soerensen CA, Salamon SA, Jensen TM, Kirkegaard H, Lisby M. Impact of clinical pharmacist intervention on length of stay in an acute admission unit: a cluster randomised study. European Journal of Hospital Pharmacy. 2016; 23(3):171–176 [PMC free article: PMC6451522] [PubMed: 31156841]
- 38.
- Lipton HL, Bero LA, Bird JA, McPhee SJ. The impact of clinical pharmacists’ consultations on physicians’ geriatric drug prescribing. A randomized controlled trial. Medical Care. 1992; 30(7):646–658 [PubMed: 1614233]
- 39.
- Lisby M, Thomsen A, Nielsen LP, Lyhne NM, Breum-Leer C, Fredberg U et al. The effect of systematic medication review in elderly patients admitted to an acute ward of internal medicine. Basic and Clinical Pharmacology and Toxicology. 2010; 106(5):422–427 [PubMed: 20059474]
- 40.
- MacLaren R, Bond CA. Effects of pharmacist participation in intensive care units on clinical and economic outcomes of critically ill patients with thromboembolic or infarction-related events. Pharmacotherapy. United States 2009; 29(7):761–768 [PubMed: 19558249]
- 41.
- Makowsky MJ, Koshman SL, Midodzi WK, Tsuyuki RT. Capturing outcomes of clinical activities performed by a rounding pharmacist practicing in a team environment: the COLLABORATE study [NCT00351676]. Medical Care. 2009; 47(6):642–650 [PubMed: 19433997]
- 42.
- Malone DC, Carter BL, Billups SJ, Valuck RJ, Barnette DJ, Sintek CD et al. Can clinical pharmacists affect SF-36 scores in veterans at high risk for medication-related problems? Medical Care. 2001; 39(2):113–122 [PubMed: 11176549]
- 43.
- Mousavi M, Hayatshahi A, Sarayani A, Hadjibabaie M, Javadi M, Torkamandi H et al. Impact of clinical pharmacist-based parenteral nutrition service for bone marrow transplantation patients: a randomized clinical trial. Supportive Care in Cancer. 2013; 21(12):3441–3448 [PubMed: 23949839]
- 44.
- Nester TM, Hale LS. Effectiveness of a pharmacist-acquired medication history in promoting patient safety. American Journal of Health-System Pharmacy. 2002; 59(22):2221–2225 [PubMed: 12455306]
- 45.
- Neto PRO, Marusic S, de Lyra Junior DP, Pilger D, Cruciol-Souza JM, Gaeti WP et al. Effect of a 36-month pharmaceutical care program on the coronary heart disease risk in elderly diabetic and hypertensive patients. Journal of Pharmacy and Pharmaceutical Sciences. 2011; 14(2):249–263 [PubMed: 21733413]
- 46.
- Nickerson A, MacKinnon NJ, Roberts N, Saulnier L. Drug-therapy problems, inconsistencies and omissions identified during a medication reconciliation and seamless care service. Healthcare Quarterly. 2005; 8 Spec No:65–72 [PubMed: 16334075]
- 47.
- O’Dell KM, Kucukarslan SN. Impact of the clinical pharmacist on readmission in patients with acute coronary syndrome. Annals of Pharmacotherapy. 2005; 39(9):1423–1427 [PubMed: 16046491]
- 48.
- O’Sullivan D, O’Mahony D, O’Connor MN, Gallagher P, Gallagher J, Cullinan S et al. Prevention of adverse drug reactions in hospitalised older patients using a software-supported structured pharmacist intervention: a cluster randomised controlled trial. Drugs and Aging. 2016; 33(1):63–73 [PubMed: 26597401]
- 49.
- Okumura LM, Rotta I, Correr CJ. Assessment of pharmacist-led patient counseling in randomized controlled trials: a systematic review. International Journal of Clinical Pharmacy. 2014; 36(5):882–891 [PubMed: 25052621]
- 50.
- Organisation for Economic Co-operation and Development (OECD). Purchasing power parities (PPP), 2007. Available from: http://www
.oecd.org/std/ppp - 51.
- Penm J, Li Y, Zhai S, Hu Y, Chaar B, Moles R. The impact of clinical pharmacy services in China on the quality use of medicines: a systematic review in context of China’s current healthcare reform. Health Policy and Planning. 2014; 29(7):849–872 [PubMed: 24056897]
- 52.
- Phatak A, Prusi R, Ward B, Hansen LO, Williams MV, Vetter E et al. Impact of pharmacist involvement in the transitional care of high-risk patients through medication reconciliation, medication education, and postdischarge call-backs (IPITCH Study). Journal of Hospital Medicine. 2016; 11(1):39–44 [PubMed: 26434752]
- 53.
- Renaudin P, Boyer L, Esteve M-A, Bertault-Peres P, Auquier P, Honore S. Do pharmacist-led medication reviews in hospitals help reduce hospital readmissions? A systematic review and meta-analysis. British Journal of Clinical Pharmacology. 2016; 82(6):1660–1673 [PMC free article: PMC5099542] [PubMed: 27511835]
- 54.
- Roblek T, Deticek A, Leskovar B, Suskovic S, Horvat M, Belic A et al. Clinical-pharmacist intervention reduces clinically relevant drug-drug interactions in patients with heart failure: a randomized, double-blind, controlled trial. International Journal of Cardiology. 2016; 203:647–652 [PubMed: 26580349]
- 55.
- Sadik A, Yousif M, McElnay JC. Pharmaceutical care of patients with heart failure. British Journal of Clinical Pharmacology. 2005; 60(2):183–193 [PMC free article: PMC1884928] [PubMed: 16042672]
- 56.
- Schnipper JL, Kirwin JL, Cotugno MC, Wahlstrom SA, Brown BA, Tarvin E et al. Role of pharmacist counseling in preventing adverse drug events after hospitalization. Archives of Internal Medicine. 2006; 166(5):565–571 [PubMed: 16534045]
- 57.
- Scullin C, Scott MG, Hogg A, McElnay JC. An innovative approach to integrated medicines management. Journal of Evaluation in Clinical Practice. 2007; 13(5):781–788 [PubMed: 17824872]
- 58.
- Shen J, Sun Q, Zhou X, Wei Y, Qi Y, Zhu J et al. Pharmacist interventions on antibiotic use in inpatients with respiratory tract infections in a Chinese hospital. International Journal of Clinical Pharmacy. 2011; 33(6):929–933 [PubMed: 22068326]
- 59.
- Spinewine A, Swine C, Dhillon S, Lambert P, Nachega JB, Wilmotte L et al. Effect of a collaborative approach on the quality of prescribing for geriatric inpatients: a randomized, controlled trial. Journal of the American Geriatrics Society. 2007; 55(5):658–665 [PubMed: 17493184]
- 60.
- Stowasser DA, Collins DM, Stowasser M. A randomised controlled trial of medication liaison services - patient outcomes. Journal of Pharmacy Practice and Research. 2002; 32(2):133–140
- 61.
- Suhaj A, Manu MK, Unnikrishnan MK, Vijayanarayana K, Mallikarjuna Rao C. Effectiveness of clinical pharmacist intervention on health-related quality of life in chronic obstructive pulmonary disorder patients - a randomized controlled study. Journal of Clinical Pharmacy and Therapeutics. 2016; 41(1):78–83 [PubMed: 26775599]
- 62.
- Tong EY, Roman C, Mitra B, Yip G, Gibbs H, Newnham H et al. Partnered pharmacist charting on admission in the General Medical and Emergency Short-stay Unit - a cluster-randomised controlled trial in patients with complex medication regimens. Journal of Clinical Pharmacy and Therapeutics. 2016; 41(4):414–418 [PubMed: 27255463]
- 63.
- Upadhyay DK, Ibrahim MI, Mishra P, Alurkar VM, Ansari M. Does pharmacist-supervised intervention through pharmaceutical care program influence direct healthcare cost burden of newly diagnosed diabetics in a tertiary care teaching hospital in Nepal: a non-clinical randomised controlled trial approach. Daru. 2016; 24(1):6 [PMC free article: PMC4772684] [PubMed: 26926657]
- 64.
- Upadhyay DK, Mohamed Ibrahim MI, Mishra P, Alurkar VM. A non-clinical randomised controlled trial to assess the impact of pharmaceutical care intervention on satisfaction level of newly diagnosed diabetes mellitus patients in a tertiary care teaching hospital in Nepal. BMC Health Services Research. 2015; 15:57 [PMC free article: PMC4448530] [PubMed: 25888828]
- 65.
- Viswanathan M, Kahwati LC, Golin CE, Blalock SJ, Coker-Schwimmer E, Posey R et al. Medication therapy management interventions in outpatient settings: a systematic review and meta-analysis. JAMA Internal Medicine. 2015; 175(1):76–87 [PubMed: 25401788]
- 66.
- Wallerstedt SM, Bladh L, Ramsberg J. A cost-effectiveness analysis of an in-hospital clinical pharmacist service. BMJ Open. Sweden 2012; 2(1):e00032 [PMC free article: PMC3253415] [PubMed: 22223840]
- 67.
- Wang Y, Wu H, Xu F. Impact of clinical pharmacy services on KAP and QOL in cancer patients: a single-center experience. BioMed Research International. 2015; 2015:502431 [PMC free article: PMC4677164] [PubMed: 26697487]
- 68.
- Zhao S, Zhao H, Du S, Qin Y. Impact of pharmaceutical care on the prognosis of patients with coronary heart disease receiving multidrug therapy. Pharmaceutical Care and Research. 2015; 15(3):179–181
- 69.
- Zhao S, Zhao H, Du S, Qin Y. The impact of clinical pharmacist support on patients receiving multi-drug therapy for coronary heart disease in china: a long-term follow-up study. European Journal of Hospital Pharmacy. 2015; 22(6):323–327 [PMC free article: PMC4502145] [PubMed: 26180276]
- 70.
- Zhao SJ, Zhao HW, Du S, Qin YH. The impact of clinical pharmacist support on patients receiving multi-drug therapy for coronary heart disease in China. Indian Journal of Pharmaceutical Sciences. 2015; 77(3):306–311 [PMC free article: PMC4502145] [PubMed: 26180276]
Appendices
Appendix A. Review protocols
Table 11
Review protocol: Pharmacist support.
Appendix B. Clinical article selection
Appendix C. Forest plots
C.1. Regular in-hospital pharmacist support
C.2. Pharmacist at admission
Appendix D. Clinical evidence tables
Download PDF (781K)
Appendix E. Economic evidence tables
E.1. Regular ward-based pharmacist support
Download PDF (573K)
E.2. Pharmacist at admission
Download PDF (425K)
E.3. Pharmacist at discharge
Download PDF (441K)
Appendix F. GRADE tables
Table 12
Clinical evidence profile: Regular in-hospital pharmacy support versus no ward-based pharmacist.
Table 13
Clinical evidence profile: Pharmacist at admission versus no ward-based pharmacist.
Table 14
Clinical evidence profile: Pharmacist at discharge versus no ward-based pharmacist.
Appendix G. Excluded clinical studies
Table 15
Studies excluded from the clinical review.
Appendix H. Excluded economic studies
No studies were excluded.
Footnotes
- (a)
NICE’s guideline on medicines optimisation includes recommendations on medicines-related communication systems when patients move from one care setting to another, medicines reconciliation, clinical decision support, and medicines-related models of organisational and cross-sector working.
Publication Details
Copyright
Publisher
National Institute for Health and Care Excellence (NICE), London
NLM Citation
National Guideline Centre (UK). Emergency and acute medical care in over 16s: service delivery and organisation. London: National Institute for Health and Care Excellence (NICE); 2018 Mar. (NICE Guideline, No. 94.) Chapter 30, Pharmacist support.